Ann Rehabil Med.
2016 Oct;40(5):943-948. 10.5535/arm.2016.40.5.943.
Neuromyelitis Optica Masquerading as Lumbosacral Radiculopathy: A Case Report
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Dongguk University College of Medicine, Goyang, Korea. rusl98@hanmail.net
- KMID: 2382928
- DOI: http://doi.org/10.5535/arm.2016.40.5.943
Abstract
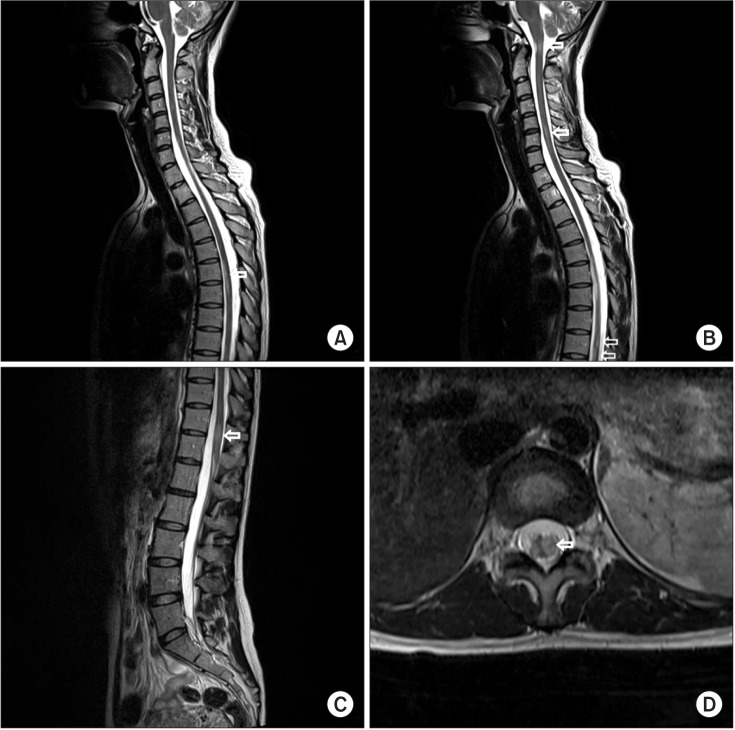
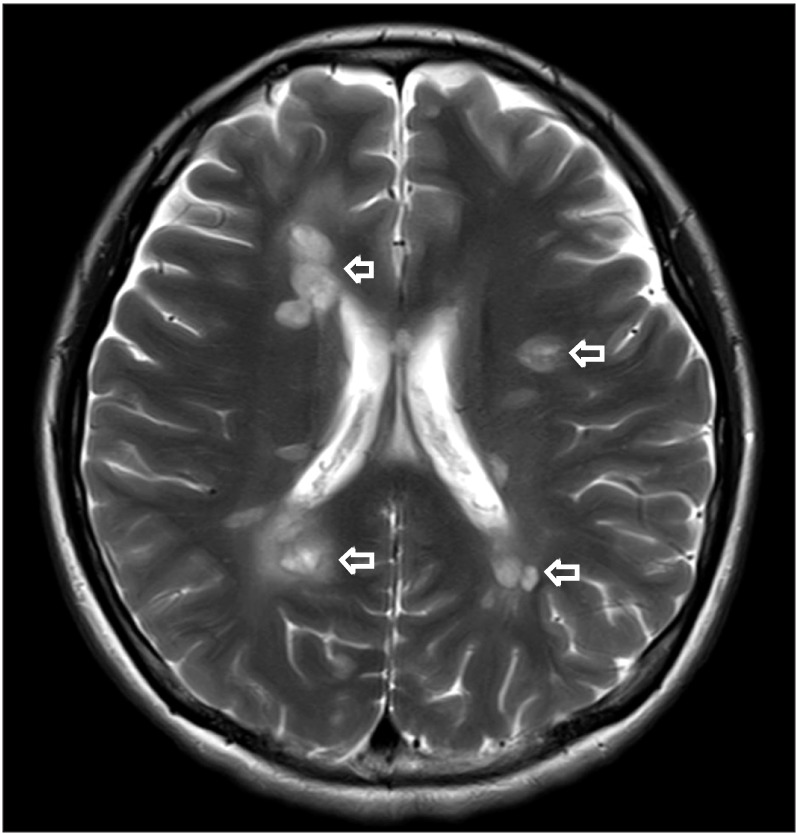
- Neuromyelitis optica spectrum disorders (NMOSD) is a demyelinating syndrome of the central nervous system. This case report describes a 31-year-old woman whose electromyography revealed radiculopathy in the left L5-S1 spinal segment without anatomical abnormalities on lumbosacral magnetic resonance imaging (MRI). She was diagnosed with NMOSD based on gadolinium contrast whole spine and brain MRI and anti-aquaporin-4 antibody findings. Her peripheral nervous system might have been damaged during the early course of NMOSD. Therefore, it is necessary to consider NMOSD for patients who have radiculopathy in electromyography if lumbosacral MRI shows no abnormalities.
MeSH Terms
Figure
Reference
-
1. Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015; 85:177–189. PMID: 26092914.
Article2. Warabi Y, Yamazaki M, Shimizu T, Nagao M. Abnormal nerve conduction study findings indicating the existence of peripheral neuropathy in multiple sclerosis and neuromyelitis optica. Biomed Res Int. 2013; 2013:847670. PMID: 24308009.
Article3. Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011; 69:292–302. PMID: 21387374.
Article4. Papadopoulos MC, Bennett JL, Verkman AS. Treatment of neuromyelitis optica: state-of-the-art and emerging therapies. Nat Rev Neurol. 2014; 10:493–506. PMID: 25112508.
Article5. Kitada M, Suzuki H, Ichihashi J, Inada R, Miyamoto K, Takahashi T, et al. Acute combined central and peripheral demyelination showing anti-aquaporin 4 antibody positivity. Intern Med. 2012; 51:2443–2447. PMID: 22975565.
Article6. Feyissa AM, Shanina E, Shah R, Smith RG. Neuromyelitis optica phenotype associated with therapy-responsive acute peripheral neuropathy. Neurol Neuroimmunol Neuroinflamm. 2015; 2:e83. PMID: 25798448.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postpartum Relapse of Neuromyelitis Optica Spectrum Disorder after a Long Period of Spontaneous Remission
- Neuromyelitis Optica (Devic's Disease)
- Neuromyelitis Optica Spectrum Disorder Presenting with Pseudoathetosis
- Steroid Unresponsive Neuromyelitis Optica Improved With Plasmapheresis
- A Case of the Neuromyelitis Optica (Devic's syndrome)