Ann Rehabil Med.
2016 Oct;40(5):794-805. 10.5535/arm.2016.40.5.794.
Intermittent Oroesophageal Tube Feeding via the Airway in Patients With Dysphagia
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. chhwang1220ciba@gmail.com
- 2School of Electrical Engineering, University of Ulsan, Ulsan, Korea.
- KMID: 2382911
- DOI: http://doi.org/10.5535/arm.2016.40.5.794
Abstract
OBJECTIVE
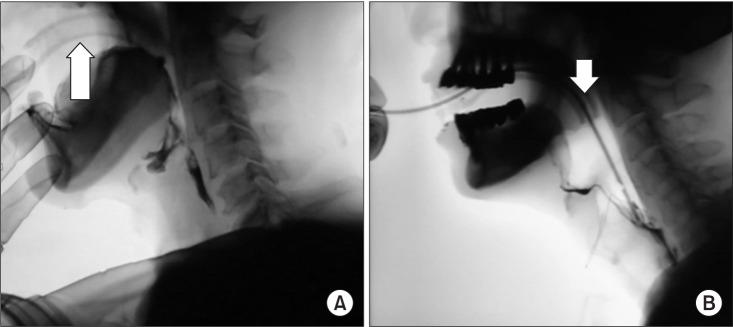
To investigate the feasibility of the use of the oropharyngeal airway (OPA) during intermittent oroesophageal tube (IOET) feeding.
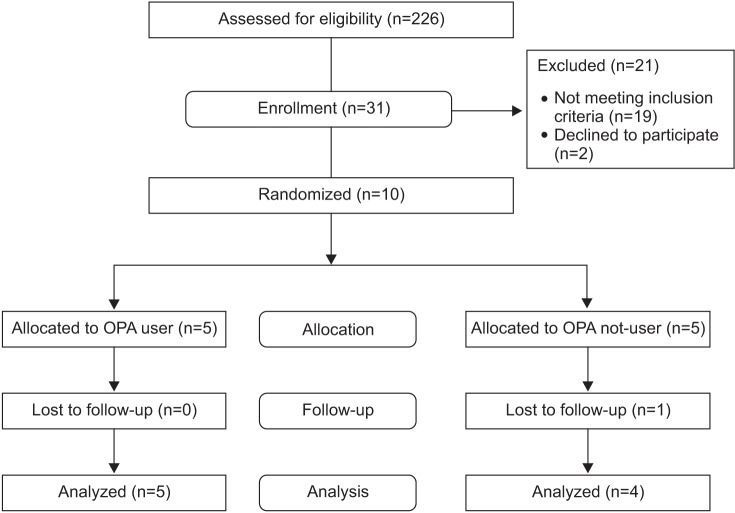
METHODS
Ten patients, who were evaluated using the videofluoroscopic swallowing study (VFSS), were enrolled. One patient withdrew from the study during the study period. Tube insertion time with and without OPA use was recorded in the same patients in a random order during the VFSS. Patients who could safely undergo IOET feeding were then randomly allocated to 2 groups (OPA and non-OPA). Satisfaction Questionnaire with Gastrostomy Feeding (SAGA-8) scores and pneumonia incidence were assessed on the 3rd and 10th day after the VFSS. Non-parametric analysis was used for statistical analyses.
RESULTS
The IOET insertion time was significantly shorter in the OPA group than in the non-OPA group (17.72±5.79 vs. 25.41±10.41 seconds; p=0.017). Complications were not significantly different between the 2 groups (p=0.054). Furthermore, although there were no significant differences in the SAGA-8 scores (25.50±2.38 vs. 21.40±3.13; p=0.066), which reflect the patient/caregiver satisfaction and the ease of tube insertion, patients in the OPA group tended to be more satisfied with the feeding procedure.
CONCLUSION
Although the small size of the study cohort is a limitation of our study, the use of the OPA appears to be beneficial during IOET feeding in patients with dysphagia.
MeSH Terms
Figure
Reference
-
1. Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter? Stroke. 1996; 27:1200–1204. PMID: 8685928.2. Campbell-Taylor I, Nadon GW, Sclater AL, Fisher R, Harris-Kwan J, Rosen I. Oro-esophageal tube feeding: an alternative to nasogastric or gastrostomy tubes. Dysphagia. 1988; 2:220–221. PMID: 3150829.
Article3. Gomes GF, Pisani JC, Macedo ED, Campos AC. The nasogastric feeding tube as a risk factor for aspiration and aspiration pneumonia. Curr Opin Clin Nutr Metab Care. 2003; 6:327–333. PMID: 12690267.
Article4. Kim Y. Nutritional considerations in tube feeding patients. J Korean Dysphagia Soc. 2011; 1:85–89.5. Han TR, Paik NJ, Park JW. The follow-up of Oro-Esophageal (OE) tube feeding. J Korean Acad Rehabil Med. 2001; 25:58–61.6. Nakajima M, Kimura K, Inatomi Y, Terasaki Y, Nagano K, Yonehara T, et al. Intermittent oro-esophageal tube feeding in acute stroke patients: a pilot study. Acta Neurol Scand. 2006; 113:36–39. PMID: 16367897.7. Han TR, Paik NJ, Park JW, Kwon BS. The prediction of persistent dysphagia beyond six months after stroke. Dysphagia. 2008; 23:59–64. PMID: 17602263.
Article8. Davies JA, Maguire AM. Variability in Guedel airway design. Anaesthesia. 2006; 61:297–298. PMID: 16480360.
Article9. Logemann JA, Gensler G, Robbins J, Lindblad AS, Brandt D, Hind JA, et al. A randomized study of three interventions for aspiration of thin liquids in patients with dementia or Parkinson's disease. J Speech Lang Hear Res. 2008; 51:173–183. PMID: 18230864.
Article10. Kuhlemeier KV, Yates P, Palmer JB. Intra- and interrater variation in the evaluation of videofluorographic swallowing studies. Dysphagia. 1998; 13:142–147. PMID: 9633153.
Article11. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997; 15:300–308.12. Logemann JA. Manual for the videofluorographic study of swallowing. 2nd ed. Austin: Pro-Ed;1993.13. Martinez-Costa C, Calderon C, Pedron-Giner C, Borraz S, Gomez-Lopez L. Psychometric properties of the structured Satisfaction Questionnaire with Gastrostomy Feeding (SAGA-8) for caregivers of children with gastrostomy tube nutritional support. J Hum Nutr Diet. 2013; 26:191–197. PMID: 23190211.
Article14. Best C. Caring for the patient with a nasogastric tube. Nurs Stand. 2005; 20:59–65. PMID: 16223197.
Article15. Ozer S, Benumof JL. Oro- and nasogastric tube passage in intubated patients: fiberoptic description of where they go at the laryngeal level and how to make them enter the esophagus. Anesthesiology. 1999; 91:137–143. PMID: 10422939.
Article16. Kisa T, Igo M, Inagawa T, Fukada M, Saito J, Setoyama M. Intermittent oral catheterization (IOC) for dysphagic stroke patients. Jpn J Rehabil Med. 1997; 34:113–120.17. Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin: Pro-Ed;1998.18. Song YJ, Park EJ, Yoon IJ, Park SJ. Tube feeding of dysphagia: the effect of oroesophageal tube feeding. J Korean Acad Occup Ther. 2009; 18:31–41.19. Santos KW, Scheeren B, Maciel AC, Cassol M. Vocal variability post swallowing in individuals with and without oropharyngeal dysphagia. Int Arch Otorhinolaryngol. 2015; 19:61–66. PMID: 25992153.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gastroesophageal Reflux during Nasogastric Tube Feeding versus Oroesophageal Tube Feeding in Stroke Patients: A 24 Hour Esophageal pH-monitoring
- Selection of Enteral Feeding in Poststroke Dysphagia
- Nutritional Considerations in Tube Feeding Patients
- Comparison of Percutaneous Endoscopic Gastrostomy and Nasogastric Tube Feeding in Dysphagic Stroke
- Swallowed Oro-esophageal Tube: A Case Report