Ann Rehabil Med.
2016 Oct;40(5):779-785. 10.5535/arm.2016.40.5.779.
Relationship Between HbA1c and Complex Regional Pain Syndrome in Stroke Patients With Type 2 Diabetes Mellitus
- Affiliations
-
- 1Department of Rehabilitation Medicine, Presbyterian Medical Center, Seonam University College of Medicine, Jeonju, Korea. withjoy9@naver.com
- KMID: 2382909
- DOI: http://doi.org/10.5535/arm.2016.40.5.779
Abstract
OBJECTIVE
To investigate the relationship between glycosylated hemoglobin A (HbA1c) and complex regional pain syndrome (CRPS) in stroke patients with type 2 diabetes mellitus (T2DM).
METHODS
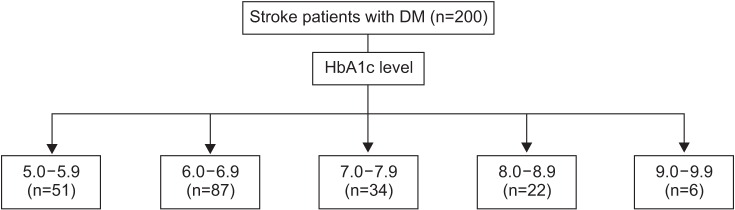
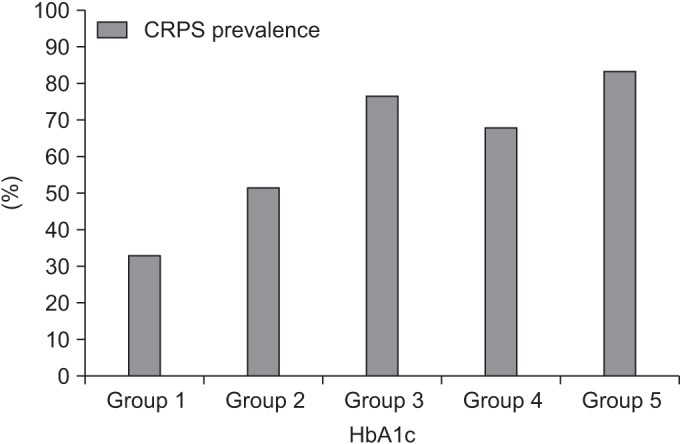
A retrospective chart review was performed of stroke patients from January 2012 to December 2013. We reviewed 331 patients and included 200 in the analysis. We divided them into CRPS and non-CRPS groups and compared them by age, gender, stroke lesion, cause of stroke, duration of T2DM, HbA1c (%), National Institutes of Health Stroke Scale score, affected shoulder flexor muscle strength, Fugl-Meyer Assessment score, motricity index, Functional Independence Measure, Korean version of Modified Barthel Index, blood glucose level on admission day, duration from stroke onset to HbA1c check, and duration from stroke onset to three-phase bone scan for CRPS diagnosis. Thereafter, we classified the patients into five groups by HbA1c level (group 1, 5.0%-5.9%; group 2, 6.0%-6.9%; group 3, 7.0%-7.9%; group 4, 8.0%-8.9%; and group 5, 9.0%-9.9%) and we investigated the difference in CRPS prevalence between the two groups.
RESULTS
Of the 200 patients, 108 were in the CRPS group and 92 were in the non-CRPS group. There were significant differences in HbA1c (p<0.05) between the two groups but no significant differences in any other factors. Across the five HbA1c groups, there were significant differences in CRPS prevalence (p<0.01); specifically, it increased as HbA1c increased.
CONCLUSION
This study suggests that higher HbA1c relates to higher CRPS prevalence and thus that uncontrolled blood glucose can affect CRPS occurrence in stroke patients with diabetes.
MeSH Terms
Figure
Reference
-
1. Stanton-Hicks M, Janig W, Hassenbusch S, Haddox JD, Boas R, Wilson P. Reflex sympathetic dystrophy: changing concepts and taxonomy. Pain. 1995; 63:127–133. PMID: 8577483.
Article2. Merskey H, Bogduk N. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. Seattle: IASP Press;1994.3. Pertoldi S, Di Benedetto P. Shoulder-hand syndrome after stroke: a complex regional pain syndrome. Eura Medicophys. 2005; 41:283–292. PMID: 16474282.4. Tepperman PS, Greyson ND, Hilbert L, Jimenez J, Williams JI. Reflex sympathetic dystrophy in hemiplegia. Arch Phys Med Rehabil. 1984; 65:442–447. PMID: 6466074.5. Cheng PT, Hong CZ. Prediction of reflex sympathetic dystrophy in hemiplegic patients by electromyographic study. Stroke. 1995; 26:2277–2280. PMID: 7491650.
Article6. Daviet JC, Preux PM, Salle JY, Lebreton F, Munoz M, Dudognon P, et al. Clinical factors in the prognosis of complex regional pain syndrome type I after stroke: a prospective study. Am J Phys Med Rehabil. 2002; 81:34–39. PMID: 11807329.7. Marinus J, Moseley GL, Birklein F, Baron R, Maihofner C, Kingery WS, et al. Clinical features and pathophysiology of complex regional pain syndrome. Lancet Neurol. 2011; 10:637–648. PMID: 21683929.
Article8. Wyatt LH, Ferrance RJ. The musculoskeletal effects of diabetes mellitus. J Can Chiropr Assoc. 2006; 50:43–50. PMID: 17549168.9. Pickup JC, Crook MA. Is type II diabetes mellitus a disease of the innate immune system? Diabetologia. 1998; 41:1241–1248. PMID: 9794114.
Article10. Malkani S, Mordes JP. Implications of using hemoglobin A1C for diagnosing diabetes mellitus. Am J Med. 2011; 124:395–401. PMID: 21531226.
Article11. Graf RJ, Halter JB, Pfeifer MA, Halar E, Brozovich F, Porte D Jr. Glycemic control and nerve conduction abnormalities in non-insulin-dependent diabetic subjects. Ann Intern Med. 1981; 94:307–311. PMID: 7013592.
Article12. Marshall AT, Crisp AJ. Reflex sympathetic dystrophy. Rheumatology (Oxford). 2000; 39:692–695. PMID: 10908684.
Article13. Kim RP. The musculoskeletal complications of diabetes. Curr Diab Rep. 2002; 2:49–52. PMID: 12643122.
Article14. Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007; 8:326–331. PMID: 17610454.
Article15. Stanton-Hicks MD, Burton AW, Bruehl SP, Carr DB, Harden RN, Hassenbusch SJ, et al. An updated interdisciplinary clinical pathway for CRPS: report of an expert panel. Pain Pract. 2002; 2:1–16. PMID: 17134466.
Article16. Calder JS, Holten I, McAllister RM. Evidence for immune system involvement in reflex sympathetic dystrophy. J Hand Surg Br. 1998; 23:147–150. PMID: 9607647.
Article17. van der Laan L, Goris RJ. Reflex sympathetic dystrophy: an exaggerated regional inflammatory response. Hand Clin. 1997; 13:373–385. PMID: 9279543.18. Holzer P. Neurogenic vasodilatation and plasma leakage in the skin. Gen Pharmacol. 1998; 30:5–11. PMID: 9457475.
Article19. Birklein F, Schmelz M, Schifter S, Weber M. The important role of neuropeptides in complex regional pain syndrome. Neurology. 2001; 57:2179–2184. PMID: 11756594.
Article20. Schinkel C, Gaertner A, Zaspel J, Zedler S, Faist E, Schuermann M. Inflammatory mediators are altered in the acute phase of posttraumatic complex regional pain syndrome. Clin J Pain. 2006; 22:235–239. PMID: 16514322.
Article21. Huygen FJ, Ramdhani N, van Toorenenbergen A, Klein J, Zijlstra FJ. Mast cells are involved in inflammatory reactions during Complex Regional Pain Syndrome type 1. Immunol Lett. 2004; 91:147–154. PMID: 15019283.
Article22. Groeneweg JG, Huygen FJ, Heijmans-Antonissen C, Niehof S, Zijlstra FJ. Increased endothelin-1 and diminished nitric oxide levels in blister fluids of patients with intermediate cold type complex regional pain syndrome type 1. BMC Musculoskelet Disord. 2006; 7:91. PMID: 17137491.
Article23. Uceyler N, Eberle T, Rolke R, Birklein F, Sommer C. Differential expression patterns of cytokines in complex regional pain syndrome. Pain. 2007; 132:195–205. PMID: 17890011.24. Wesseldijk F, Huygen FJ, Heijmans-Antonissen C, Niehof SP, Zijlstra FJ. Six years follow-up of the levels of TNF-alpha and IL-6 in patients with complex regional pain syndrome type 1. Mediators Inflamm. 2008; 2008:469439. PMID: 18596918.25. Parkitny L, McAuley JH, Di Pietro F, Stanton TR, O'Connell NE, Marinus J, et al. Inflammation in complex regional pain syndrome: a systematic review and meta-analysis. Neurology. 2013; 80:106–117. PMID: 23267031.
Article26. Pickup JC. Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care. 2004; 27:813–823. PMID: 14988310.
Article27. Crook MA, Tutt P, Pickup JC. Elevated serum sialic acid concentration in NIDDM and its relationship to blood pressure and retinopathy. Diabetes Care. 1993; 16:57–60. PMID: 8422833.
Article28. Mirza S, Hossain M, Mathews C, Martinez P, Pino P, Gay JL, et al. Type 2-diabetes is associated with elevated levels of TNF-alpha, IL-6 and adiponectin and low levels of leptin in a population of Mexican Americans: a cross-sectional study. Cytokine. 2012; 57:136–142. PMID: 22035595.
Article29. Alexandraki KI, Piperi C, Ziakas PD, Apostolopoulos NV, Makrilakis K, Syriou V, et al. Cytokine secretion in long-standing diabetes mellitus type 1 and 2: associations with low-grade systemic inflammation. J Clin Immunol. 2008; 28:314–321. PMID: 18224429.
Article30. Bastard JP, Pieroni L, Hainque B. Relationship between plasma plasminogen activator inhibitor 1 and insulin resistance. Diabetes Metab Res Rev. 2000; 16:192–201. PMID: 10867719.
Article31. Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nat Rev Immunol. 2011; 11:98–107. PMID: 21233852.
Article32. Pickup JC, Chusney GD, Thomas SM, Burt D. Plasma interleukin-6, tumour necrosis factor alpha and blood cytokine production in type 2 diabetes. Life Sci. 2000; 67:291–300. PMID: 10983873.33. Dandona P, Aljada A, Chaudhuri A, Bandyopadhyay A. The potential influence of inflammation and insulin resistance on the pathogenesis and treatment of atherosclerosis-related complications in type 2 diabetes. J Clin Endocrinol Metab. 2003; 88:2422–2429. PMID: 12788837.
Article34. Veldman PH, Reynen HM, Arntz IE, Goris RJ. Signs and symptoms of reflex sympathetic dystrophy: prospective study of 829 patients. Lancet. 1993; 342:1012–1016. PMID: 8105263.
Article35. Kozin F. Reflex sympathetic dystrophy syndrome: a review. Clin Exp Rheumatol. 1992; 10:401–409. PMID: 1395224.36. Schwartzman RJ, McLellan TL. Reflex sympathetic dystrophy: a review. Arch Neurol. 1987; 44:555–561. PMID: 3495254.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contralateral Mirror Image Spreading in Post-Stroke Complex Regional Pain Syndrome
- Complex Regional Pain Syndrome Type I after Stroke
- The Relationship between Depression, Self-Care Activity and HbA1c in Clients with Type-2 Diabetes Mellitus
- Musculoskeletal Problems in Upper Extremity after Stroke
- Management Strategies for Children and Adolescents with Diabetes Mellitus