J Korean Ophthalmol Soc.
2017 Jun;58(6):751-755. 10.3341/jkos.2017.58.6.751.
A Case of Acute Macular Neuroretinopathy in a Young Male
- Affiliations
-
- 1Department of Ophthalmology, Gyeongsang National University School of Medicine, Jinju, Korea. parkjm@gnu.ac.kr
- 2Department of Ophthalmology, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- KMID: 2382688
- DOI: http://doi.org/10.3341/jkos.2017.58.6.751
Abstract
- PURPOSE
We report a rare case of unilateral acute macular neuroretinoapthy in a young male.
CASE SUMMARY
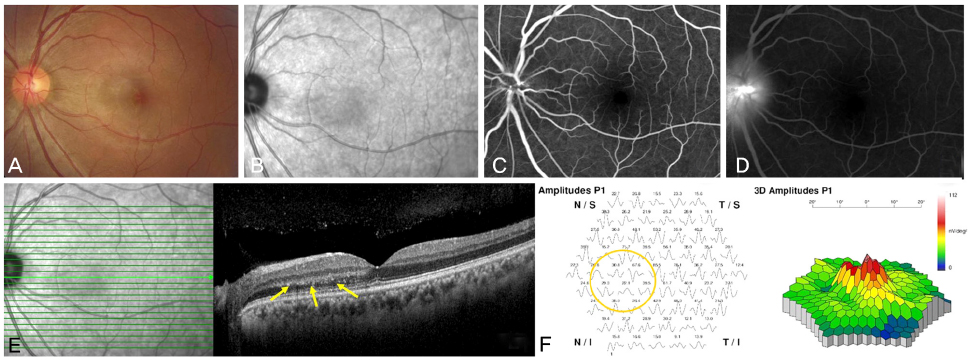
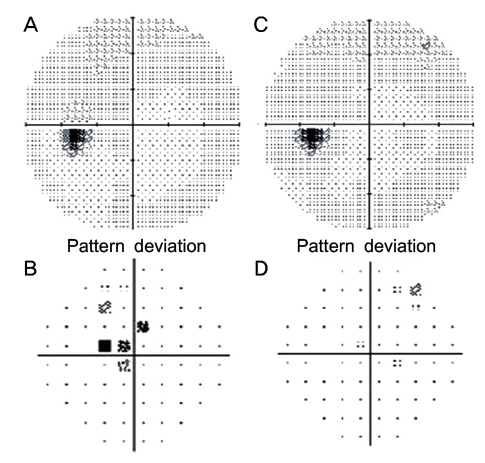
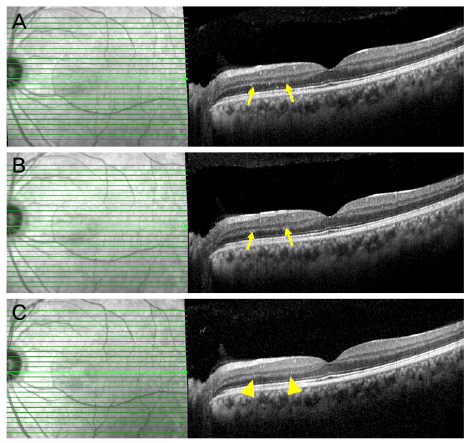
A 35-year-old male presented with a 2-day history of paracentral scotoma. He had suffered for 2 days from a flu-like illness, and his best corrected visual acuity was 20/20 OD and 20/20 OS. Pupillary reflex was normal and no relative afferent pupillary defects were not found. Ocular movement test was normal and pain on ocular movement was not noticed. Ophthalmoscopic examination of the left eye revealed multiple exudates lining the nasal macula toward the fovea. A Humphrey visual field study identified small paracentral scotoma. Spectral domain optical coherence tomography (SD-OCT, Heidelberg Engineering, Heidelberg, Germany) of the lesions showed a hyper-reflective lesion located in the outer plexiform layer and inflammatory cell infiltration. Fluorescent angiography was normal in the macula but showed late leak at the disc. The multifocal electroretinogram (mfERG) showed decreased foveal P1 amplitude in the left eye. The patient was diagnosed with acute macular neuroretinopathy and was treated with 60 mg of prednisolone. His subjective symptoms were improved, the paracentral scotoma disappeared, and the lesions appeared different upon SD-OCT; specifically, the hyper-reflective lesion disappeared and the outer plexiform layer showed thinning.
CONCLUSIONS
Acute macular neuroretinopathy is a rare disease, and we report a case using SD-OCT and mfERG.
Keyword
MeSH Terms
Figure
Reference
-
1. Bos PJ, Deutman AF. Acute macular neuroretinopathy. Am J Ophthalmol. 1975; 80:573–584.2. Priluck IA, Buettner H, Robertson DM. Acute macular neuroretinopathy. Am J Ophthalmol. 1978; 86:775–778.3. Turbeville SD, Cowan LD, Gass JD. Acute macular neuroretinopathy: a review of the literature. Surv Ophthalmol. 2003; 48:1–11.4. Fawzi AA, Pappuru RR, Sarraf D, et al. Acute macular neuroretinopathy: long-term insights revealed by multimodal imaging. Retina. 2012; 32:1500–1513.5. Sarraf D, Rahimy E, Fawzi AA, et al. Paracentral acute middle maculopathy: a new variant of acute macular neuroretinopathy associated with retinal capillary ischemia. JAMA Ophthalmol. 2013; 131:1275–1287.6. Vance SK, Spaide RF, Freund KB, et al. Outer retinal abnormalities in acute macular neuroretinopathy. Retina. 2011; 31:441–445.7. Feigl B, Haas A. Optical coherence tomography (OCT) in acute macular neuroretinopathy. Acta Ophthalmol Scand. 2000; 78:714–716.8. Lee SH, Bae JS, Kim YY. A case of bilateral acute macular neuroretinopathy after URI. J Korean Ophthalmol Soc. 2013; 54:1614–1620.9. Kim SE, Lee SE, Kim YY. A case of acute macular neuroretinopathy after non-ocular trauma. J Korean Ophthalmol Soc. 2016; 57:1970–1975.10. Lee DH, Lee SC, Kim M. Acute macular neuroretinopathy associated with systemic lupus erythematosus. Lupus. 2016; 25:431–435.11. Aziz HA, Kheir WJ, Young RC, et al. Acute macular neuroretinopathy: a case report and review of the literature, 2002–2012. Ophthalmic Surg Lasers Imaging Retina. 2015; 46:114–124.12. Baumüller S, Holz FG. Early spectral-domain optical coherence tomography findings in acute macular neuroretinopathy. Retina. 2012; 32:409–410.13. Heuges EH, Siow YC, Hunyor AP. Acute macular neuroretinopahty: anatomic localization of the lesion with high-resolution OCT. Eye (Lond). 2009; 23:2132–2134.14. Monson BK, Greenberg PB, Greenberg E, et al. High–speed, ultra-high-resolution optical coherence tomography of acute macular neuroretinopathy. Br J Ophthalmol. 2007; 91:119–120.15. Maschi C, Schneider-Lise B, Paoli V, Gastaud P. Acute macular neuroretinopathy: contribution of spectral-domain optical coherence tomography and multifocal ERG. Graefes Arch Clin Exp Ophthalmol. 2011; 249:827–831.16. Maturi RK, Yu M, Sprunger DT. Multifocal electroretinographic evaluation of acute macular neuroretinopathy. Arch Ophthalmol. 2003; 121:1068–1069.17. Birol G, Wang S, Budzynski E, et al. Oxygen distribution and consumption in the macaque retina. Am J Physiol Heart Circ physiol. 2007; 293:1696–1704.18. Stone J, van Driel D, Valter K, et al. The locations of mitochondria in mammalian photoreceptors: relation to retinal vasculature. Brain Res. 2008; 1189:58–69.19. Wangsa-Wirawan ND, Linsenmeier RA. Retinal oxygen: fundamental and clinical aspects. Arch Ophthalmol. 2003; 121:547–557.20. Munk MR, Beck M, Kolb S, et al. Quantification of retinal layer thickness changes in acute macular neuroretinopathy. Br J Ophthalmol. 2017; 101:160–165.21. Dansingani KK, Freund KB. Paracentral Acute Middle Maculopathy and Acute Macular Neuroretinopathy: Related and Distinct Entities. Am J Ophthalmol. 2015; 160:1–3.e2.22. Bhavsar KV, Lin S, Rahimy E, et al. Acute macular neuroretinopathy: A comprehensive review of the literature. Surv Ophthalmol. 2016; 61:538–565.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Acute Macular Neuroretinopathy after Non-ocular Trauma
- A Case of Bilateral Acute Macular Neuroretinopathy after URI
- Acute Isolated Tear of Gluteus Medius in Young Male
- A Case of Bilateral Macular Hole in a Patient with Bilateral Macular Telangiectasia
- Influence of the Macular Curvature on Foveal Migration after Macular Hole Surgery