J Korean Foot Ankle Soc.
2017 Jun;21(2):55-60. 10.14193/jkfas.2017.21.2.55.
The Effectiveness of Plantar Aponeurosis Release for the Limitation in First Metatarsophalangeal Joint Extension after Hallux Valgus Surgery
- Affiliations
-
- 1Department of Orthopedic Surgery, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. cool-cool0829@hanmail.net
- 2Department of Orthopedic Surgery, Busan Centum Hospital, Busan, Korea.
- KMID: 2382425
- DOI: http://doi.org/10.14193/jkfas.2017.21.2.55
Abstract
- PURPOSE
Stiffness in the first metatarsophalangeal joint after surgery for hallux valgus has been reported. The goal of this study was to test the efficacy of releasing plantar aponeurosis for improving the range of extension in the first metatarsophalangeal joint that was limited after hallux valgus surgery.
MATERIALS AND METHODS
Thirteen patients (1 man, 12 women [17 feet]; median age, 54.4 years; range, 44~69 years) with limited first metatarsophalangeal joint extension after hallux valgus surgery, who underwent an additional procedure of plantar aponeurosis release between March 2015 and August 2015, were included. Subsequently, the passive range of extension in the first metatarsophalangeal joint was evaluated via knee extension and flexion positions. Hallux valgus angle, inter-metatarsal angle, distal metatarsal articular angle, and talo-first metatarsal angle were measured on weightbearing dorsoplantar and lateral radiographs of the foot preoperatively.
RESULTS
The mean range of extension for the first metatarsophalangeal joint improved significantly, from 2.5° to 40.9° in the knee extension position (p<0.00). The mean extension range for the first metatarsophalangeal joint also improved, from 18.2° to 43.2° in the knee flexion position (p<0.00). In all patients, congruence of the first metatarsophalangeal joint was recovered.
CONCLUSION
Plantar aponeurosis release is an effective additional procedure for improving the extension range of the first metatarsophalangeal joint after hallux valgus surgery.
MeSH Terms
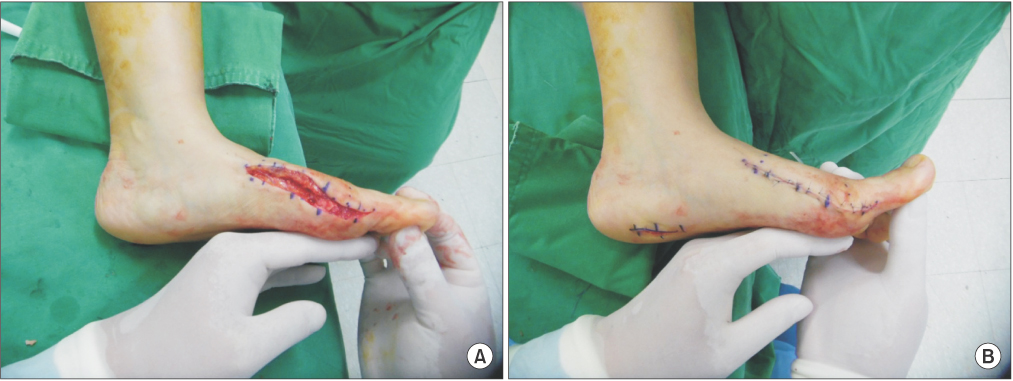
Figure
Reference
-
1. Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010; 3:21.
Article2. Richardson EG, Graves SC, McClure JT, Boone RT. First metatarsal head-shaft angle: a method of determination. Foot Ankle. 1993; 14:181–185.
Article3. Robinson AH, Limbers JP. Modern concepts in the treatment of hallux valgus. J Bone Joint Surg Br. 2005; 87:1038–1045.
Article4. Easley ME, Trnka HJ. Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int. 2007; 28:748–758.
Article5. Klosok JK, Pring DJ, Jessop JH, Maffulli N. Chevron or Wilson metatarsal osteotomy for hallux valgus. A prospective randomised trial. J Bone Joint Surg Br. 1993; 75:825–829.
Article6. Thompson FM. Complications of hallux valgus surgery and salvage. Orthopedics. 1990; 13:1059–1067.
Article7. Wülker N, Mittag F. The treatment of hallux valgus. Dtsch Arztebl Int. 2012; 109:857–867. quiz 868.
Article8. Baravarian B, Ben-Ad R. Revision hallux valgus: causes and correction options. Clin Podiatr Med Surg. 2014; 31:291–298.9. Schuh R, Willegger M, Holinka J, Ristl R, Windhager R, Wanivenhaus AH. Angular correction and complications of proximal first metatarsal osteotomies for hallux valgus deformity. Int Orthop. 2013; 37:1771–1780.
Article10. Kernozek TW, Sterriker SA. Chevron (Austin) distal metatarsal osteotomy for hallux valgus: comparison of pre- and post-surgical characteristics. Foot Ankle Int. 2002; 23:503–508.
Article11. Hetherington VJ, Johnson RE, Albritton JS. Necessary dorsiflexion of the first metatarsophalangeal joint during gait. J Foot Surg. 1990; 29:218–222.12. Barouk LS. The effect of gastrocnemius tightness on the pathogenesis of juvenile hallux valgus: a preliminary study. Foot Ankle Clin. 2014; 19:807–822.
Article13. Jones RO, Harkless LB, Baer MS, Wilkinson SV. Retrospective statistical analysis of factors influencing the formation of long-term complications following hallux abducto valgus surgery. J Foot Surg. 1991; 30:344–349.14. Laird PO. Functional hallux limitus. Illinois Podiatrists. 1972; 9:4.15. Silfverskiold N. Reduction of the uncrossed two-joints muscles of the leg to one-joint muscles in spastic conditions. Acta Chir Scand. 1924; 56:315–330.16. Abbassian A, Kohls-Gatzoulis J, Solan MC. Proximal medial gastrocnemius release in the treatment of recalcitrant plantar fasciitis. Foot Ankle Int. 2012; 33:14–19.
Article17. Barouk LS, Barouk P, Toulec E. Resulltats de la liberation proximale des Gastrocnemiens [Results of proximal gastrocnemius release]. Paper presented at: Etude Prospective Symposium Brièveté des gastrocnémiens symposium journees de Printemps SFMCP-AFCP, Toulouse. Med Chir Pied. 2006; 22:151–156.18. De los Santos-Real R, Morales-Muñoz P, Payo J, Escalera-Alonso J. Gastrocnemius proximal release with minimal incision: a modified technique. Foot Ankle Int. 2012; 33:750–754.
Article19. Sarrafian SK. Anatomy of the foot and ankle. 2nd ed. Philadelphia: Lippincott William & Wilkins;1993.20. Snow SW, Bohne WH, DiCarlo E, Chang VK. Anatomy of the Achilles tendon and plantar fascia in relation to the calcaneus in various age groups. Foot Ankle Int. 1995; 16:418–421.
Article21. Arandes R, Viladot A. Biomecanica del Calcaneo. Med Clin. 1954; 21:21–25.22. Barouk LS, Barouk P. Hallux valgus et Gastrocnemiens courts: étude de deux series cliniques. Brièveté des gastrocnémiens. Montpellier (France): Sauramps;2012. p. 265–268.23. Drakos MC, DiGiovanni CW. Importance de la brièveté isolée des gastrocné-miens dans la pathologie du pied. Brièveté des Gastrocnémiens: de l'anatomie au traitement. Montpellier (France): Sauramps;2012. p. 231–240.24. Maceira E, Orejana A. Hallux limitus fonctionnel et le système suro- Achilleoplantaire Brièveté des gastrocnémiens. De l'anatomie au traitement. Montpellier (France): Sauramps;2012. p. 147–194.25. Pascual Huerta J. Brièveté des gastrocnémiens et son effet sur l'aponévrose plantaire et le comportement sagittal. Brièveté des gastrocnémiens de l'anatomie au traitement. Montpellier (France): Sauramps;2012. p. 119–140.26. Kowalski C, Diebold P, Pennecot GF. Le tendon Calcaneen court. Paris: Encyclopedie medico Chirurgicale Elsevier;1999. p. 27–60.27. Dananberg HJ. Functional hallux limitus and its relationship to gait efficiency. J Am Podiatr Med Assoc. 1986; 76:648–652.
Article28. Maceira E, Monteagudo M. Functional hallux rigidus and the Achilles-calcaneus-plantar system. Foot Ankle Clin. 2014; 19:669–699.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arthrodesis Of The First Metsatarophalangeal Joint For Rheumatoid Arthritis And Hallux Valgus
- Correlation of Correction Angle with Pain at First Metatarsophalangeal Joint in the Treatment of Hallux Valgus
- Arthrodesis of the First Metatarsophalangeal Joint for Rheumatoid Hallux Valgus, using 2 Crossed Screws
- Triple Osteotomy for Hallux Valgus in Patient with Osteopetrosis: A Case Report
- A Clinical Study of Chevron Osteotomy in Bunion - Hallux Valgus