J Korean Med Sci.
2017 Jul;32(7):1202-1206. 10.3346/jkms.2017.32.7.1202.
Different Age Distribution between Campylobacteriosis and Nontyphoidal Salmonellosis in Hospitalized Korean Children with Acute Inflammatory Diarrhea
- Affiliations
-
- 1Department of Pediatrics, Korea University College of Medicine, Seoul, Korea.
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. jychang7@snu.ac.kr
- 3Department of Pediatrics, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea.
- 4Department of Laboratory Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Laboratory Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea.
- KMID: 2379618
- DOI: http://doi.org/10.3346/jkms.2017.32.7.1202
Abstract
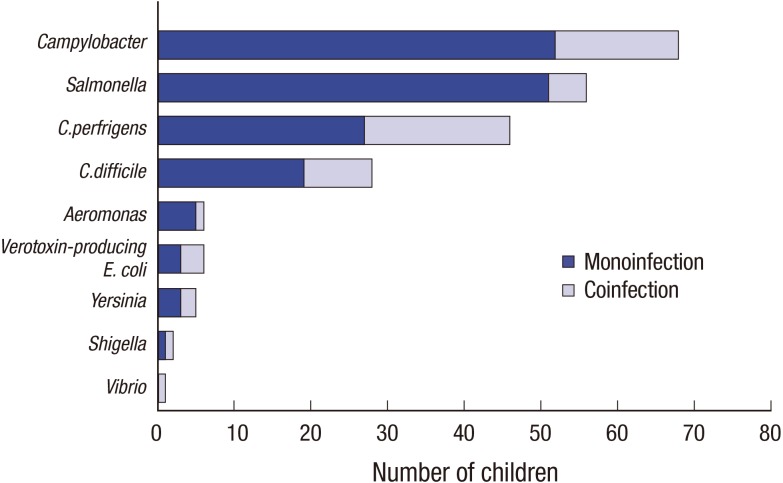
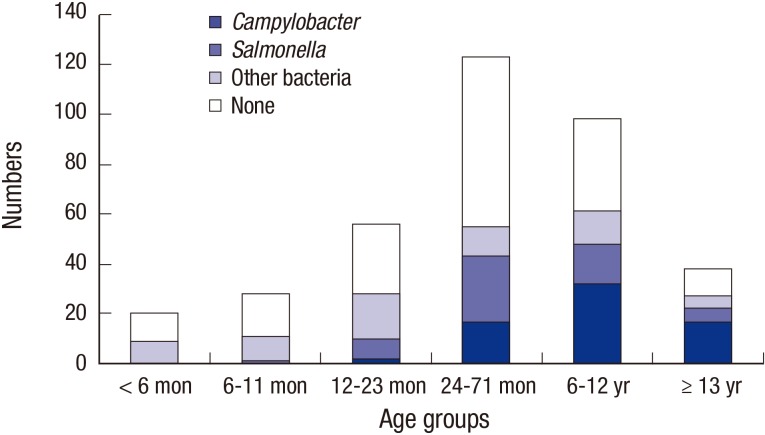
- We investigated recent epidemiologic trends regarding campylobacteriosis vs. nontyphoidal salmonellosis (NTS), a previously known leading cause of bacterial enterocolitis in Korean children. Among 363 hospitalized children with acute inflammatory diarrhea, Campylobacter (18.7%) was the most frequently detected pathogen using multiplex polymerase chain reaction tests followed by Salmonella (15.4%). Children with campylobacteriosis were older than children with NTS (112.6 months [interquartile range (IQR) 66.0-160.1] vs. 53 months [IQR 31.0-124.0], P < 0.001) and had higher prevalences of abdominal cramping and stool hemoglobin. Campylobacteriosis may be suspected as a primary cause of acute inflammatory diarrhea in hospitalized school-aged Korean children and adolescents.
Keyword
MeSH Terms
Figure
Reference
-
1. World Health Organization. Campylobacter [Internet]. accessed on 2 January 2017. Available at http://www.who.int/mediacentre/factsheets/fs255/en/.2. Schmutz C, Mäusezahl D, Jost M, Baumgartner A, Mäusezahl-Feuz M. Inverse trends of Campylobacter and Salmonella in Swiss surveillance data, 1988–2013. Euro Surveill. 2016; 21:30130.3. Eurosurveillance editorial team. The 2013 joint ECDC/EFSA report on trends and sources of zoonoses, zoonotic agents and food-borne outbreaks published. Euro Surveill. 2015; 20:21021. PMID: 25655057.4. Korea Center for Disease Control and Prevention. Communicable diseases weekly report [Internet]. accessed on 2 January 2017. Available at http://www.cdc.go.kr/CDC/.5. Cho MC, Noh SA, Kim MN, Kim KM. Direct application of multiplex PCR on stool specimens for detection of enteropathogenic bacteria. Korean J Clin Microbiol. 2010; 13:162–168.6. Shim JO, Chang JY, Shin S, Moon JS, Ko JS. Changing distribution of age, clinical severity, and genotypes of rotavirus gastroenteritis in hospitalized children after the introduction of vaccination: a single center study in Seoul between 2011 and 2014. BMC Infect Dis. 2016; 16:287. PMID: 27296987.7. Kim A, Chang JY, Shin S, Yi H, Moon JS, Ko JS, Oh S. Epidemiology and factors related to clinical severity of acute gastroenteritis in hospitalized children after the introduction of rotavirus vaccination. J Korean Med Sci. 2017; 32:465–474. PMID: 28145650.8. Guarino A, Ashkenazi S, Gendrel D, Lo Vecchio A, Shamir R, Szajewska H; European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. European Society for Pediatric Infectious Diseases. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe: update 2014. J Pediatr Gastroenterol Nutr. 2014; 59:132–152. PMID: 24739189.9. Onori M, Coltella L, Mancinelli L, Argentieri M, Menichella D, Villani A, Grandin A, Valentini D, Raponi M, Russo C. Evaluation of a multiplex PCR assay for simultaneous detection of bacterial and viral enteropathogens in stool samples of paediatric patients. Diagn Microbiol Infect Dis. 2014; 79:149–154. PMID: 24656922.10. Wei W, Schüpbach G, Held L. Time-series analysis of Campylobacter incidence in Switzerland. Epidemiol Infect. 2015; 143:1982–1989. PMID: 25400006.11. Pursem VN, Peeroo BM, Mangar TI, Sohawon FM, Seheri LM, Mphahlele MJ, Mwenda JM, Manraj SS. Epidemiology of rotavirus diarrhea and diversity of rotavirus strains among children less than 5 years of age with acute gastroenteritis in Mauritius: June 2008 to December 2010. Pediatr Infect Dis J. 2014; 33(Suppl 1):S49–S53. PMID: 24343614.12. Kittl S, Kuhnert P, Hächler H, Korczak BM. Comparison of genotypes and antibiotic resistance of Campylobacter jejuni isolated from humans and slaughtered chickens in Switzerland. J Appl Microbiol. 2011; 110:513–520. PMID: 21143711.13. Shaw AN, Heresi GP, Murphy JR. Campylobacter. In : Kliegman R, Stanton B, St Geme JW, Schor NF, editors. Nelson Textbook of Pediatrics. 20th ed. Philadelphia, PA: Elsevier;2016. p. 1403–1406.14. Noh SH, Yu KY, Kim JS, Hwang PH, Jo DS. Salmonellosis in children: analysis of 72 Salmonella-positive culture cases during the last 10 years. Korean J Pediatr. 2009; 52:791–797.15. Park HK, Rhie K, Yeom JS, Park JS, Park ES, Seo JH, Lim JY, Park CH, Woo HO, Youn HS, et al. Differences in clinical and laboratory findings between group D and non-group D non-typhoidal Salmonella gastroenteritis in children. Pediatr Gastroenterol Hepatol Nutr. 2015; 18:85–93. PMID: 26157693.16. Ford L, Glass K, Veitch M, Wardell R, Polkinghorne B, Dobbins T, Lal A, Kirk MD. Increasing incidence of Salmonella in Australia, 2000–2013. PLoS One. 2016; 11:e0163989. PMID: 27732615.17. Wensley A, Coole L. Cohort study of a dual-pathogen point source outbreak associated with the consumption of chicken liver pâté, UK, October 2009. J Public Health (Oxf). 2013; 35:585–589. PMID: 23509410.18. Cho IJ, Yim J, Lee Y, Kim MS, Seo Y, Chung HS, Yong D, Jeong SH, Lee K, Chong Y. Trends in isolation and antimicrobial susceptibility of enteropathogenic bacteria in 2001–2010 at a Korean tertiary care hospital. Ann Clin Microbiol. 2013; 16:45–51.19. Lee J, Kim J, Cho H, Oh K, Uh Y, Yoon KJ. Detection of bacterial and viral pathogens in stool specimens using multiplex PCR. J Lab Med Qual Assur. 2015; 37:141–147.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Children with Nontyphoidal Salmonellosis Assumed by Pets
- Prevalence, Laboratory Findings and Clinical Characteristics of Campylobacteriosis Agents among Hospitalized Children with Acute Gastroenteritis in Lebanon
- Pyogenic Spondylitis Caused by Nontyphoidal Salmonella in an Immunocompetent Child
- Diagnosis of Enteropathogens in Children with Acute Gastroenteritis: One Year Prospective Study in a Single Hospital
- Acute viral gastroenteritis in children hospitalized in Iksan, Korea during December 2010-June 2011