J Korean Med Sci.
2017 Jul;32(7):1166-1172. 10.3346/jkms.2017.32.7.1166.
Relationship between Mobile Phone Addiction and the Incidence of Poor and Short Sleep among Korean Adolescents: a Longitudinal Study of the Korean Children & Youth Panel Survey
- Affiliations
-
- 1Department of Public Health, Yonsei University College of Medicine, Seoul, Korea.
- 2Institute of Health Services Research, Yonsei University College of Medicine, Seoul, Korea. ecpark@yuhs.ac
- 3Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2379613
- DOI: http://doi.org/10.3346/jkms.2017.32.7.1166
Abstract
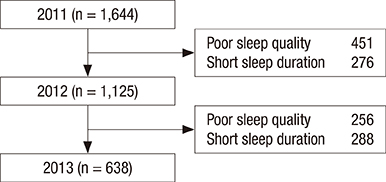
- Three of ten teenagers in Korea are addicted to mobile phones. The aim of this study was to examine the relationship between mobile phone addiction and the incidence of poor sleep quality and short sleep duration in adolescents. We used longitudinal data from the Korean Children & Youth Panel Survey conducted by the National Youth Policy Institute in Korea (2011-2013). A total of 1,125 students at baseline were included in this study after excluding those who already had poor sleep quality or short sleep duration in the previous year. A generalized estimating equation was used to analyze the data. High mobile phone addiction (mobile phone addiction score > 20) increased the risk of poor sleep quality but not short sleep duration. We suggest that consistent monitoring and effective intervention programs are required to prevent mobile phone addiction and improve adolescents' sleep quality.
Figure
Reference
-
1. Groupe Speciale Mobile Association (JP). Children's use of mobile phones and personal relationships: an international comparison 2011 [Internet]. accessed on 8 May 2017. Available at http://www.gsma.com/publicpolicy/wp-content/uploads/2012/03/Childrensuseofmobilephones2011.pdf.2. Ministry of Science, ICT and Future Planning (KR). Internet addiction survey 2014 [Internet]. accessed on 8 May 2017. Available at http://msip.go.kr/SYNAP/skin/doc.html?fn=7d3b3733d68811084a78cc79d78a38bd&rs=/SYNAP/sn3hcv/result/201704/.3. Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, Nugent TF 3rd, Herman DH, Clasen LS, Toga AW, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci USA. 2004; 101:8174–8179.4. Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006; 10:323–337.5. Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004; 1021:276–291.6. Kwon JA, Lee M, Yoo KB, Park EC. Does the duration and time of sleep increase the risk of allergic rhinitis? Results of the 6-year nationwide Korea youth risk behavior web-based survey. PLoS One. 2013; 8:e72507.7. Kim JH, Park EC, Lee SG, Yoo KB. Associations between time in bed and suicidal thoughts, plans and attempts in Korean adolescents. BMJ Open. 2015; 5:e008766.8. Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 2011; 12:110–118.9. Dollman J, Ridley K, Olds T, Lowe E. Trends in the duration of school-day sleep among 10- to 15-year-old South Australians between 1985 and 2004. Acta Paediatr. 2007; 96:1011–1014.10. Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003; 111:302–307.11. Schmidt AT, Li X, Hanten GR, McCauley SR, Faber J, Levin HS. A longitudinal investigation of sleep quality in adolescents and young adults after mild traumatic brain injury. Cogn Behav Neurol. 2015; 28:53–62.12. Kronholm E, Puusniekka R, Jokela J, Villberg J, Urrila AS, Paunio T, Välimaa R, Tynjälä J. Trends in self-reported sleep problems, tiredness and related school performance among Finnish adolescents from 1984 to 2011. J Sleep Res. 2015; 24:3–10.13. Jenni OG, Molinari L, Caflisch JA, Largo RH. Sleep duration from ages 1 to 10 years: variability and stability in comparison with growth. Pediatrics. 2007; 120:e769–e776.14. Punamäki RL, Wallenius M, Nygård CH, Saarni L, Rimpelä A. Use of information and communication technology (ICT) and perceived health in adolescence: the role of sleeping habits and waking-time tiredness. J Adolesc. 2007; 30:569–585.15. Harada T, Morikuni M, Yoshii S, Yamashita Y, Takeuchi H. Usage of mobile phone in the evening or at night makes Japanese students evening-typed and night sleep uncomfortable. Sleep Hypn. 2002; 4:149–153.16. Yen CF, Ko CH, Yen JY, Cheng CP. The multidimensional correlates associated with short nocturnal sleep duration and subjective insomnia among Taiwanese adolescents. Sleep. 2008; 31:1515–1525.17. Thomée S, Härenstam A, Hagberg M. Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults--a prospective cohort study. BMC Public Health. 2011; 11:66.18. Arora T, Broglia E, Thomas GN, Taheri S. Associations between specific technologies and adolescent sleep quantity, sleep quality, and parasomnias. Sleep Med. 2014; 15:240–247.19. Söderqvist F, Carlberg M, Hardell L. Use of wireless telephones and self-reported health symptoms: a population-based study among Swedish adolescents aged 15–19 years. Environ Health. 2008; 7:18.20. Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A. Adolescents' electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. J Youth Adolesc. 2015; 44:405–418.21. Murdock KK. Texting while stressed: implications for students' burnout, sleep, and well-being. Psychol Pop Media Cult. 2013; 2:207–221.22. Maslowsky J, Ozer EJ. Developmental trends in sleep duration in adolescence and young adulthood: evidence from a national United States sample. J Adolesc Health. 2014; 54:691–697.23. Tagaya H, Uchiyama M, Ohida T, Kamei Y, Shibui K, Ozaki A, Tan X, Suzuki H, Aritake S, Li L, et al. Sleep habits and factors associated with short sleep duration among Japanese high-school students: a community study. Sleep Biol Rhythms. 2004; 2:57–64.24. Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, Hazen N, Herman J, Hillard PJ, Katz ES, et al. National Sleep Foundation's updated sleep duration recommendations: final report. Sleep Health. 2015; 1:233–243.25. Van den Bulck J, Van den Bergh B. The influence of perceived parental guidance patterns on children's media use: gender differences and media displacement. J Broadcast Electron Media. 2000; 44:329–348.26. Igarashi T, Takai J, Yoshida T. Gender differences in social network development via mobile phone text messages: a longitudinal study. J Soc Pers Relat. 2005; 22:691–713.27. Lee SY, Park EC, Han KT, Kim SJ, Chun SY, Park S. The association of level of internet use with suicidal ideation and suicide attempts in South Korean adolescents: a focus on family structure and household economic status. Can J Psychiatry. 2016; 61:243–251.28. White AG, Buboltz W, Igou F. Mobile phone use and sleep quality and length in college students. Int J Humanit Soc Sci. 2011; 1:51–58.29. Li J, Lepp A, Barkley JE. Locus of control and cell phone use: implications for sleep quality, academic performance, and subjective well-being. Comput Human Behav. 2015; 52:450–457.30. Gaina A, Sekine M, Kanayama H, Sengoku K, Yamagami T, Kagamimori S. Short–long sleep latency and associated factors in Japanese junior high school children. Sleep Biol Rhythms. 2005; 3:162–165.31. Bertocci MA, Dahl RE, Williamson DE, Iosif AM, Birmaher B, Axelson D, Ryan ND. Subjective sleep complaints in pediatric depression: a controlled study and comparison with EEG measures of sleep and waking. J Am Acad Child Adolesc Psychiatry. 2005; 44:1158–1166.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The moderated mediating effect of parental smartphone addiction in the relationship between smartphone addiction, sleep duration, and depression among adolescents
- The current status of health data on Korean children and adolescents
- Factors Influencing Cell Phone Addiction in Adolescents
- Educational Needs for Prevention of Cell Phone Addiction in Korean Adolescents
- Gender Differences in the Relationship between Social Jet Lag, Depression, and Obesity in Korean Children and Adolescents