Korean J Orthod.
2017 Jul;47(4):248-255. 10.4041/kjod.2017.47.4.248.
Clustering of craniofacial patterns in Korean children with snoring
- Affiliations
-
- 1Department of Dentistry, Kyung Hee University Graduate School, Seoul, Korea.
- 2Department of Orthodontics, Chonnam National University School of Dentistry, Gwangju, Korea.
- 3Department of Orthodontics, Center for Advanced Dental Education, Saint Louis University, St. Louis, MO, USA.
- 4Department of Otorhinolaryngology Head and Neck Surgery, Kyung Hee University School of Medicine, Seoul, Korea.
- 5Department of Orthodontics, Kyung Hee University School of Dentistry, Seoul, Korea. ksj113@khu.ac.kr
- KMID: 2379557
- DOI: http://doi.org/10.4041/kjod.2017.47.4.248
Abstract
OBJECTIVE
The purpose of this study was to investigate whether the craniofacial patterns of Korean children with snoring and adenotonsillar hypertrophy (ATH) could be categorized into characteristic clusters according to age.
METHODS
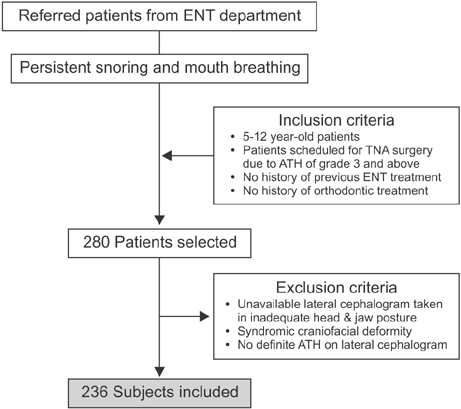
We enrolled 236 children with snoring and ATH (age range, 5-12 years) in this study. They were subdivided into four age groups: 5-6, 7-8, 9-10, and 11-12 years. Based on cephalometric analysis, the sagittal and vertical skeletal patterns of each individual were divided into Class I, II, and III, as well as the normodivergent, hypodivergent, and hyperdivergent patterns, respectively. Cluster analysis was performed using cephalometric principal components in addition to the age factor.
RESULTS
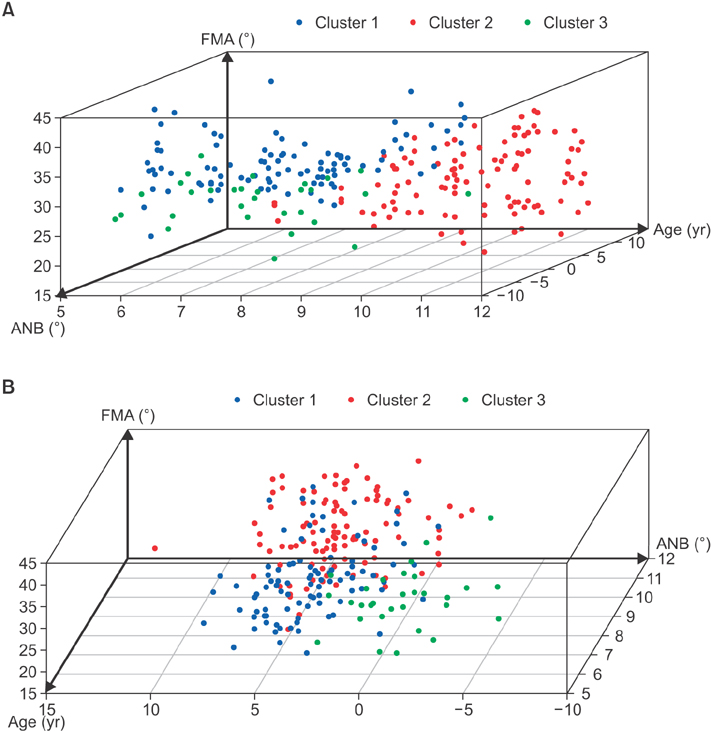
Three heterogeneous clusters of craniofacial patterns were obtained in relation to age: cluster 1 (41.9%) included patients aged 5-8 years with a skeletal Class I or mild Class II and hyperdivergent pattern; cluster 2 (45.3%) included patients aged 9-12 years with a Class II and hyperdivergent pattern; and cluster 3 (12.8%) included patients aged 7-8 years with a Class III and hyperdivergent pattern.
CONCLUSIONS
This study found that the craniofacial patterns of Korean children with snoring and ATH could be categorized into three characteristic clusters according to age groups. Although no significantly dominant sagittal skeletal discrepancy was observed, hyperdivergent vertical discrepancy was consistently evident in all clusters.
Figure
Reference
-
1. Li HY, Lee LA. Sleep-disordered breathing in children. Chang Gung Med J. 2009; 32:247–257.2. Lumeng JC, Chervin RD. Epidemiology of pediatric obstructive sleep apnea. Proc Am Thorac Soc. 2008; 5:242–252.
Article3. Sinha D, Guilleminault C. Sleep disordered breathing in children. Indian J Med Res. 2010; 131:311–320.4. Katyal V, Pamula Y, Martin AJ, Daynes CN, Kennedy JD, Sampson WJ. Craniofacial and upper airway morphology in pediatric sleep-disordered breathing: Systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2013; 143:20–30.e3.
Article5. Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012; 130:e714–e755.
Article6. Di Francesco RC, Passerotii G, Paulucci B, Miniti A. Mouth breathing in children: different repercussions according to the diagnosis. Rev Bras Otorrinolaringol. 2004; 70:665–670.7. Chung Leng Muñoz I, Beltri Orta P. Comparison of cephalometric patterns in mouth breathing and nose breathing children. Int J Pediatr Otorhinolaryngol. 2014; 78:1167–1172.
Article8. Feres MF, Hermann JS, Cappellette M Jr, Pignatari SS. Lateral X-ray view of the skull for the diagnosis of adenoid hypertrophy: a systematic review. Int J Pediatr Otorhinolaryngol. 2011; 75:1–11.
Article9. Baroni M, Ballanti F, Franchi L, Cozza P. Craniofacial features of subjects with adenoid, tonsillar, or adenotonsillar hypertrophy. Prog Orthod. 2011; 12:38–44.
Article10. Huang YS, Guilleminault C. Pediatric obstructive sleep apnea and the critical role of oral-facial growth: evidences. Front Neurol. 2013; 3:184.
Article11. Löfstrand-Tideström B, Hultcrantz E. Development of craniofacial and dental arch morphology in relation to sleep disordered breathing from 4 to 12 years. Effects of adenotonsillar surgery. Int J Pediatr Otorhinolaryngol. 2010; 74:137–143.
Article12. Chi L, Comyn FL, Keenan BT, Cater J, Maislin G, Pack AI, et al. Heritability of craniofacial structures in normal subjects and patients with sleep apnea. Sleep. 2014; 37:1689–1698.
Article13. Huang YS, Guilleminault C, Lee LA, Lin CH, Hwang FM. Treatment outcomes of adenotonsillectomy for children with obstructive sleep apnea: a prospective longitudinal study. Sleep. 2014; 37:71–76.
Article14. Arun T, Isik F, Sayinsu K. Vertical growth changes after adenoidectomy. Angle Orthod. 2003; 73:146–150.15. Mitchell RB. Adenotonsillectomy for obstructive sleep apnea in children: outcome evaluated by pre- and postoperative polysomnography. Laryngoscope. 2007; 117:1844–1854.
Article16. Venekamp RP, Hearne BJ, Chandrasekharan D, Blackshaw H, Lim J, Schilder AG. Tonsillectomy or adenotonsillectomy versus non-surgical management for obstructive sleep-disordered breathing in children. Cochrane Database Syst Rev. 2015; (10):CD011165.
Article17. Valera FC, Travitzki LV, Mattar SE, Matsumoto MA, Elias AM, Anselmo-Lima WT. Muscular, functional and orthodontic changes in pre school children with enlarged adenoids and tonsils. Int J Pediatr Otorhinolaryngol. 2003; 67:761–770.
Article18. Kim DK, Rhee CS, Yun PY, Kim JW. Adenotonsillar hypertrophy as a risk factor of dentofacial abnormal ity in Korean chi ldren. Eur Arch Otorhinolaryngol. 2015; 272:3311–3316.
Article19. Franco LP, Souki BQ, Cheib PL, Abrão M, Pereira TB, Becker HM, et al. Are distinct etiologies of upper airway obstruction in mouth-breathing children associated with different cephalometric patterns? Int J Pediatr Otorhinolaryngol. 2015; 79:223–228.
Article20. Zhong Z, Tang Z, Gao X, Zeng XL. A comparison study of upper airway among different skeletal craniofacial patterns in nonsnoring Chinese children. Angle Orthod. 2010; 80:267–274.
Article21. Alessandri-Bonetti G, Ippolito DR, Bartolucci ML, D'Antò V, Incerti-Parenti S. Cephalometric predictors of treatment outcome with mandibular advancement devices in adult patients with obstructive sleep apnea: a systematic review. Korean J Orthod. 2015; 45:308–321.
Article22. Lee SJ, Lee S, Lim J, Ahn SJ, Kim TW. Cluster analysis of tooth size in subjects with normal occlusion. Am J Orthod Dentofacial Orthop. 2007; 132:796–800.
Article23. Brodsky L, Moore L, Stanievich JF. A comparison of tonsillar size and oropharyngeal dimensions in children with obstructive adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol. 1987; 13:149–156.
Article24. Major MP, Flores-Mir C, Major PW. Assessment of lateral cephalometric diagnosis of adenoid hypertrophy and posterior upper airway obstruction: a systematic review. Am J Orthod Dentofacial Orthop. 2006; 130:700–708.
Article25. Cistulli PA. Craniofacial abnormalities in obstructive sleep apnoea: implications for treatment. Respirology. 1996; 1:167–174.
Article26. Flores-Mir C, Korayem M, Heo G, Witmans M, Major MP, Major PW. Craniofacial morphological characteristics in children with obstructive sleep apnea syndrome: a systematic review and meta-analysis. J Am Dent Assoc. 2013; 144:269–277.
Article27. Hultcrantz E, Larson M, Hellquist R, Ahlquist-Rastad J, Svanholm H, Jakobsson OP. The influence of tonsillar obstruction and tonsillectomy on facial growth and dental arch morphology. Int J Pediatr Otorhinolaryngol. 1991; 22:125–134.
Article28. Peltomäki T. The effect of mode of breathing on craniofacial growth--revisited. Eur J Orthod. 2007; 29:426–429.
Article29. Nelson S, Cakirer B, Lai YY. Longitudinal changes in craniofacial factors among snoring and nonsnoring Bolton-Brush study participants. Am J Orthod Dentofacial Orthop. 2003; 123:338–344.
Article30. Sousa JB, Anselmo-Lima WT, Valera FC, Gallego AJ, Matsumoto MA. Cephalometric assessment of the mandibular growth pattern in mouth-breathing children. Int J Pediatr Otorhinolaryngol. 2005; 69:311–317.
Article31. Park KH, Bayome M, Park JH, Lee JW, Baek SH, Kook YA. New classification of lingual arch form in normal occlusion using three dimensional virtual models. Korean J Orthod. 2015; 45:74–81.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Utility of Adenotonsillectomy to Treat Snoring in Children: Acoustic Evaluation Using Smartphones
- Upper airway and obstructive sleep apnea in children
- Asian Pacific Craniofacial Association and Archives of Craniofacial Surgery
- Gene Expression Pattern Analysis via Latent Variable Models Coupled with Topographic Clustering
- Patterns of Insulin Resistance Syndrome in the Taegu Community for the Development of Nutritional Service Improvement Programs