Int J Thyroidol.
2017 May;10(1):56-60. 10.11106/ijt.2017.10.1.56.
A Case of Acute Cerebral Infarction and Thyroid Storm Associated with Moyamoya Disease
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Chonbuk National University Hospital, Chonbuk National University Medical School, Jeonju, Korea. kaleey@jbnu.ac.kr
- KMID: 2379363
- DOI: http://doi.org/10.11106/ijt.2017.10.1.56
Abstract
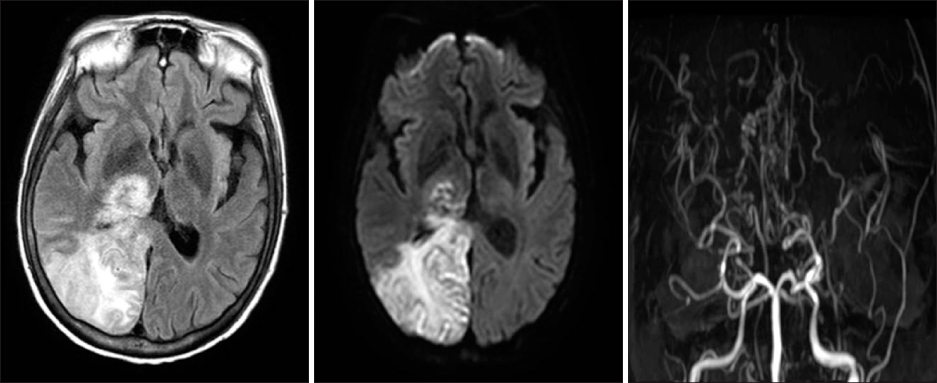
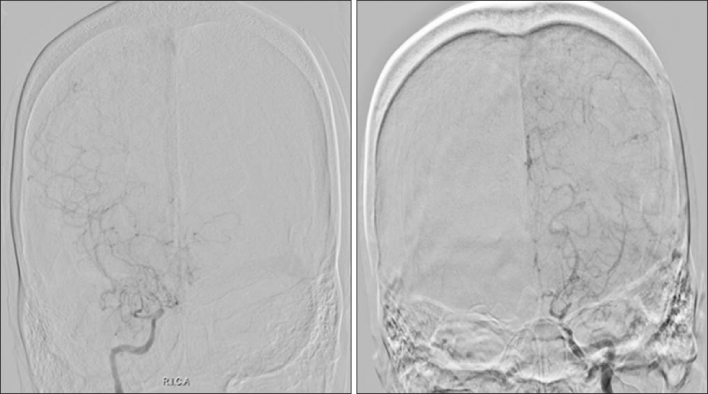
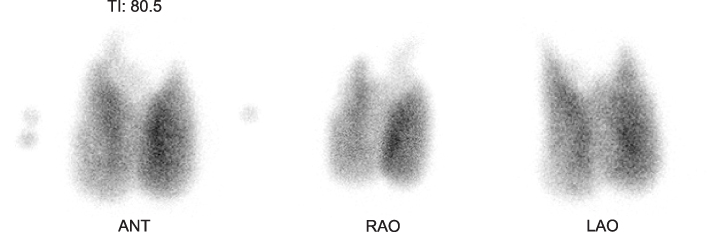
- Coexistence of moyamoya disease and Graves' disease is rare. A 41-year-old woman presented with symptoms of left-sided hemiparesis and dysarthria. Magnetic resonance imaging and angiography revealed acute infarction of the right thalamus and occipital lobe with complete obstruction of the distal internal carotid arteries and obstruction of the right P2. Free thyroxine, thyroid-stimulating hormone (TSH), and TSH receptor antibody levels were 79.33 pmol/L, 0.007 uIU/mL, and 151.5 u/L, respectively. She received antiplatelet therapy and standard antithyroid drug dose. After admission, seizure and unexplained fever occurred. The thyroid storm score (Burch and Wartofsky scale) was 90 points. After intensive treatment, mental status and thyrotoxicosis-related symptoms ameliorated and vital signs stabilized. We describe a case of thyroid storm following cerebrovascular ischemic events in a Korean woman with moyamoya disease and Graves' disease. Thyroid storm combined with cerebrovascular events can lead to severe morbidity and mortality. Prompt recognition and strict management are crucial.
Keyword
MeSH Terms
-
Adult
Angiography
Carotid Artery, Internal
Cerebral Infarction*
Dysarthria
Female
Fever
Graves Disease
Humans
Infarction
Magnetic Resonance Imaging
Mortality
Moyamoya Disease*
Occipital Lobe
Paresis
Receptors, Thyrotropin
Seizures
Thalamus
Thyroid Crisis*
Thyroid Gland*
Thyrotropin
Thyroxine
Vital Signs
Receptors, Thyrotropin
Thyrotropin
Thyroxine
Figure
Cited by 1 articles
-
Acute cerebral infarction combined with a thyroid storm in a patient with both Moyamoya syndrome and Graves’ disease
Jong Han Gill, Taek Kyun Nam, Hoon Kyo Jung, Kyung Min Jang, Hyun Ho Choi, Yong Sook Park, Jeong Taik Kwon
J Cerebrovasc Endovasc Neurosurg. 2022;24(2):160-165. doi: 10.7461/jcen.2021.E2021.07.003.
Reference
-
1. Im SH, Oh CW, Kwon OK, Kim JE, Han DH. Moyamoya disease associated with Graves disease: special considerations regarding clinical significance and management. J Neurosurg. 2005; 102(6):1013–1017.
Article2. Burch HB, Wartofsky L. Life-threatening thyrotoxicosis. Thyroid storm. Endocrinol Metab Clin North Am. 1993; 22(2):263–277.
Article3. Ren SC, Gao BQ, Yang WL, Feng WX, Xu J, Li SW, et al. Von Willebrand factor and coagulation factor VIII in Moyamoya disease associated with Graves' disease: a case report. Exp Ther Med. 2016; 12(5):3195–3200.
Article4. Back JH, Kang HM, Min BD, Gil SH, Kim SJ, Oh BC, et al. A case of Graves' disease associated with myasthenia gravis and complicated with Moyamoya disease. Korean J Med. 2010; 79(2):195–200.5. Shin DW, Seo JY, Lee JG, Kim JS, Lee KB, Roh H, et al. Acute ischemic stroke in Moyamoya disease associated with thyrotoxic crisis. J Korean Neurol Assoc. 2014; 32(2):95–97.6. Cheon CK, Kim SY, Yoo JH. Two adolescent patients with coexistent Graves' disease and Moyamoya disease in Korea. Korean J Pediatr. 2014; 57(6):287–291.
Article7. Shen AL, Ryu SJ, Lin SK. Concurrent moyamoya disease and Graves' thyrotoxicosis: case report and literature review. Acta Neurol Taiwan. 2006; 15(2):114–119.8. Sasaki T, Nogawa S, Amano T. Co-morbidity of moyamoya disease with Graves' disease. report of three cases and a review of the literature. Intern Med. 2006; 45(9):649–653.
Article9. Siegert CE, Smelt AH, de Bruin TW. Superior sagittal sinus thrombosis and thyrotoxicosis. Possible association in two cases. Stroke. 1995; 26(3):496–497.
Article10. Ni J, Zhou LX, Wei YP, Li ML, Xu WH, Gao S, et al. Moyamoya syndrome associated with Graves' disease: a case series study. Ann Transl Med. 2014; 2(8):77.11. Lei C, Wu B, Ma Z, Zhang S, Liu M. Association of moyamoya disease with thyroid autoantibodies and thyroid function: a case-control study and meta-analysis. Eur J Neurol. 2014; 21(7):996–1001.
Article12. Kim SJ, Heo KG, Shin HY, Bang OY, Kim GM, Chung CS, et al. Association of thyroid autoantibodies with moyamoya-type cerebrovascular disease: a prospective study. Stroke. 2010; 41(1):173–176.
Article13. Colleran KM, Ratliff DM, Burge MR. Potential association of thyrotoxicosis with vitamin B and folate deficiencies, resulting in risk for hyperhomocysteinemia and subsequent thromboembolic events. Endocr Pract. 2003; 9(4):290–295.
Article14. Iso H, Moriyama Y, Sato S, Kitamura A, Tanigawa T, Yamagishi K, et al. Serum total homocysteine concentrations and risk of stroke and its subtypes in Japanese. Circulation. 2004; 109(22):2766–2772.
Article15. van Diemen-Steenvoorde R, van Nieuwenhuizen O, de Klerk JB, Duran M. Quasi-moyamoya disease and heterozygosity for homocystinuria in a five-year-old girl. Neuropediatrics. 1990; 21(2):110–112.
Article16. Lee R, Sung K, Park YM, Yu JJ, Koh YC, Chung S. A case of Moyamoya disease in a girl with thyrotoxicosis. Yonsei Med J. 2009; 50(4):594–598.
Article17. Hsu SW, Chaloupka JC, Fattal D. Rapidly progressive fatal bihemispheric infarction secondary to Moyamoya syndrome in association with Graves thyrotoxicosis. AJNR Am J Neuroradiol. 2006; 27(3):643–647.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute cerebral infarction combined with a thyroid storm in a patient with both Moyamoya syndrome and Graves’ disease
- Acute Ischemic Stroke in Moyamoya Disease Associated With Thyrotoxic Crisis
- Moyamoya Syndrome Associated With Hashimoto's Thyroiditis
- Acute Ischemic Stroke in Moyamoya Syndrome Associated with Thyrotoxicosis
- The Occurrence of a Thyroid Storm in a Patient with Recurrent Refractory Peptic Ulcer: A Case Report