J Korean Ophthalmol Soc.
2017 May;58(5):600-605. 10.3341/jkos.2017.58.5.600.
A Case Report of Takayasu's Arteritis with Traction Retinal Detachment
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kangsewoong@gmail.com
- KMID: 2378633
- DOI: http://doi.org/10.3341/jkos.2017.58.5.600
Abstract
- PURPOSE
To report a rare case of traction retinal detachment and retinal ischemia in inactive Takayasu's arteritis at ophthalmologic clinic.
CASE SUMMARY
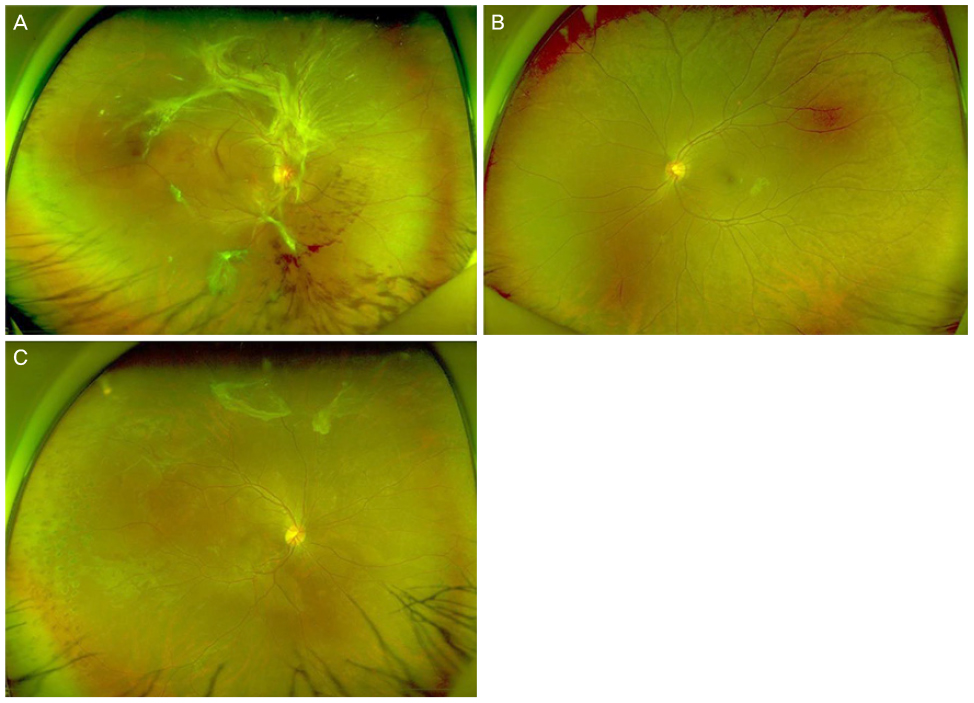
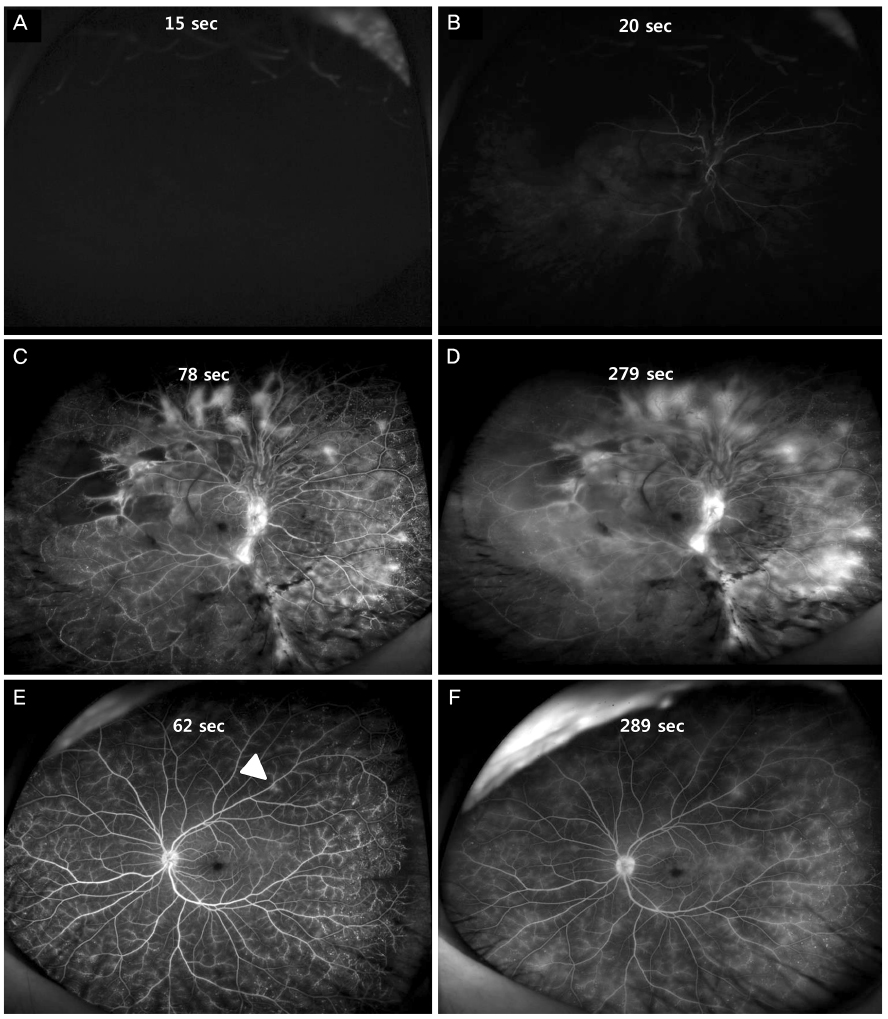
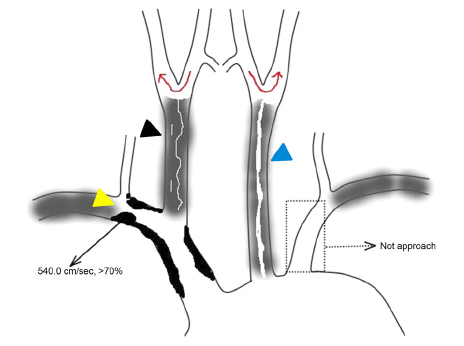
A 23-year-old woman presented with a floater, photophobia, and visual loss in her right eye one week prior to visit. She had no other systemic disease, such as diabetes mellitus or hypertension, or previous ophthalmic abnormalities except for a tumor in the adrenal gland. We found bilateral retinal ischemia and traction retinal detachment in the right eye on fundus examination without iris neovascularization. Pars plana vitrectomy, traction removal, endolaser treatment, and intravitreal bevacizumab injection were performed. Steroid eye drops and steroid systemic administration relieved the inflammation. On carotid doppler sonography, we found severe stenosis and thickness of the inner layer in both carotid arteries. We diagnosed the patient with an inactive phase of Takayasu's arteritis, which was conclusively correlated with the clinical features. Vascular anastomosis surgery along with follow-up was proposed by both the cardiology and vascular surgery departments.
CONCLUSIONS
When a young patient presents with traction retinal detachment and retinal ischemia, Takayasu's arteritis should be considered for differential diagnosis and a systemic work-up should be performed as soon as possible.
MeSH Terms
-
Adrenal Glands
Bevacizumab
Cardiology
Carotid Arteries
Constriction, Pathologic
Diabetes Mellitus
Diagnosis, Differential
Female
Follow-Up Studies
Humans
Hypertension
Inflammation
Iris
Ischemia
Ophthalmic Solutions
Photophobia
Retinal Detachment*
Retinaldehyde*
Takayasu Arteritis*
Traction*
Vitrectomy
Young Adult
Bevacizumab
Ophthalmic Solutions
Retinaldehyde
Figure
Reference
-
1. Panja M, Mondal PC. Current status of aortoarteritis in India. J Assoc Physicians India. 2004; 52:48–52.2. Peter J, Joseph G, David S, Danda D. Regression of takayasu retinopathy after revascularization of occluded branches of the aortic arch by percutaneous angioplasty. Retin Cases Brief Rep. 2013; 7:262–266.3. Baba T, Itakura K, Tanaka R, et al. Importance of fluorescein angiographic study in evaluating early retinal changes in Takayasu disease. Jpn J Ophthalmol. 1999; 43:546–552.4. Chun YS, Park SJ, Park IK, et al. The clinical and ocular manifestations of Takayasu arteritis. Retina. 2001; 21:132–140.5. Kiyosawa M, Baba T. Ophthalmological findings in patients with Takayasu disease. Int J Cardiol. 1998; 66:Suppl 1. S141–S147.6. Sagar S, Kar S, Gupta A, Sharma BK. Ocular changes in Takayasu's arteritis in India. Jpn J Ophthalmol. 1994; 38:97–102.7. Peter J, David S, Danda D, et al. Ocular manifestations of Takayasu arteritis: a cross-sectional study. Retina. 2011; 31:1170–1178.8. Lee JC, Wang MY, Damodar D, et al. Headache and whiteout vision as the presenting symptoms in a case of Takayasu retinopathy. Retin Cases Brief Rep. 2014; 8:273–275.9. Shailaja S, Vivek G, Shetty R, Kamath Y. 'Eye is a window to the pulse': bilateral ocular ischaemic syndrome as a presenting manifestation of Takayasu arteritis. BMJ Case Rep. 2013; 2013:pii: bcr2013009461.10. Peter J, Joseph G, Mathew V, Peter JV. Visual loss in Takayasu Arteritis - Look Beyond the Eye. J Clin Diagn Res. 2014; 8:MD06–MD07.11. Kuwahara C, Imamura Y, Okamura N, et al. Severe proliferative retinopathy progressing to blindness in a japanese woman with takayasu disease. Am J Ophthalmol. 2003; 135:722–723.12. Koz OG, Ates A, Numan Alp M, et al. Bilateral ocular ischemic syndrome as an initial manifestation of Takayasu's arteritis associated with carotid steal syndrome. Rheumatol Int. 2007; 27:299–302.13. Pelegrín L, Mesquida M, Rey A, et al. Blind runner. Surv Ophthalmol. 2012; 57:486–494.14. Elizalde J, Capella MJ. Takayasu's retinopathy. Int Ophthalmol. 2011; 31:533–537.15. Slusher MM, Richards CP. Postsurgical alterations in visual acuity, retinal vasculature, and retinal circulation times in Takayasu's disease. Retina. 2002; 22:116–117.16. Tracci MC, Cherry KJ. Surgical treatment of great vessel occlusive disease. Surg Clin North Am. 2009; 89:821–836. viii17. Goldman DR, Prasad PS, Schwartz SD. Dramatic resolution of extreme ocular ischemia in a case of Takayasu's arteritis. Ophthalmic Surg Lasers Imaging Retina. 2013; 44:198–200.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Takayasu's Arteritis Associated with Serous Retinal Detachment
- Retinal Detachment Associated with Probable Zonular Traction Tufts
- A Case Report of Takayaeu's Arteritis Associated with, a Retinopathy
- Takayasu's Arteritis: report of 2 cases and review of literature
- A Case of Intracranial Aneurysm Associated with Takayasu's Arteritis: Case Report