Obstet Gynecol Sci.
2016 Nov;59(6):434-443. 10.5468/ogs.2016.59.6.434.
Differences in clinical presentation and pregnancy outcomes in antepartum preeclampsia and new-onset postpartum preeclampsia: Are these the same disorder?
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Wayne State University/Hutzel Women's Hospital, Detroit, MI, USA. VilchezLagosG@umkc.edu
- 2Universidad Nacional Federico Villareal, Lima, Peru.
- 3Department of Obstetrics and Gynecology, Johns Hopkins University School of Medicine, Baltimore, MD, USA.
- KMID: 2378567
- DOI: http://doi.org/10.5468/ogs.2016.59.6.434
Abstract
OBJECTIVE
New-onset postpartum preeclampsia is a poorly defined condition that accounts for a significant percentage of eclampsia cases. It is unclear whether new-onset postpartum preeclampsia is a different disorder from or belongs to the same spectrum of classic antepartum preeclampsia. The objective of this study was to compare the clinical presentation and pregnancy outcomes of antepartum preeclampsia and new-onset postpartum preeclampsia.
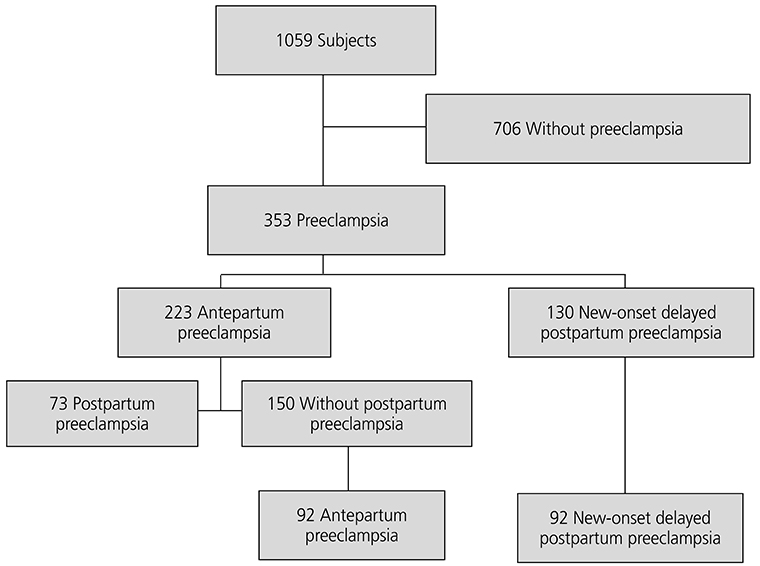
METHODS
A retrospective study including 92 patients with antepartum preeclampsia and 92 patients with new-onset postpartum preeclampsia was performed. Clinical presentation and pregnancy outcomes were compared. Chi-square test was used to analyze categorical variables, and independent t-test and Mann-Whitney U-test for numerical variables. P-values of <0.05 were used to indicate statistical signifi cance.
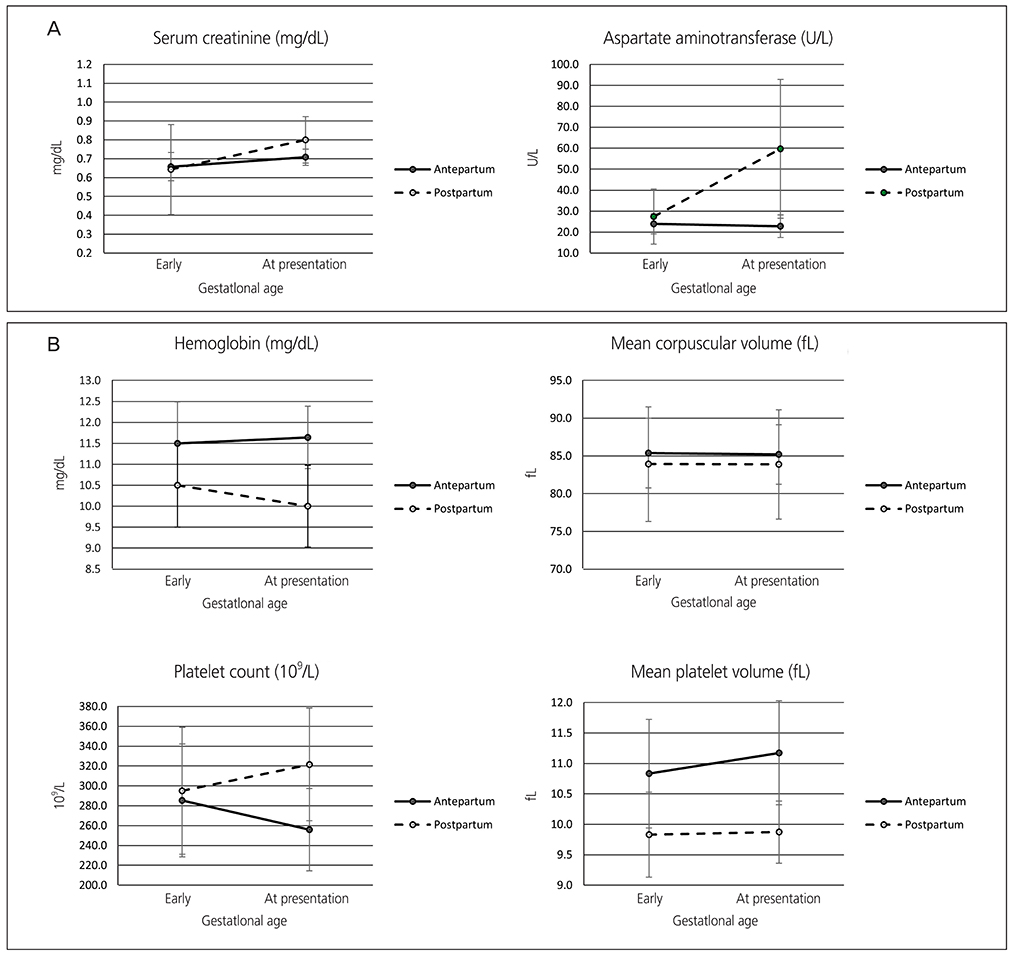
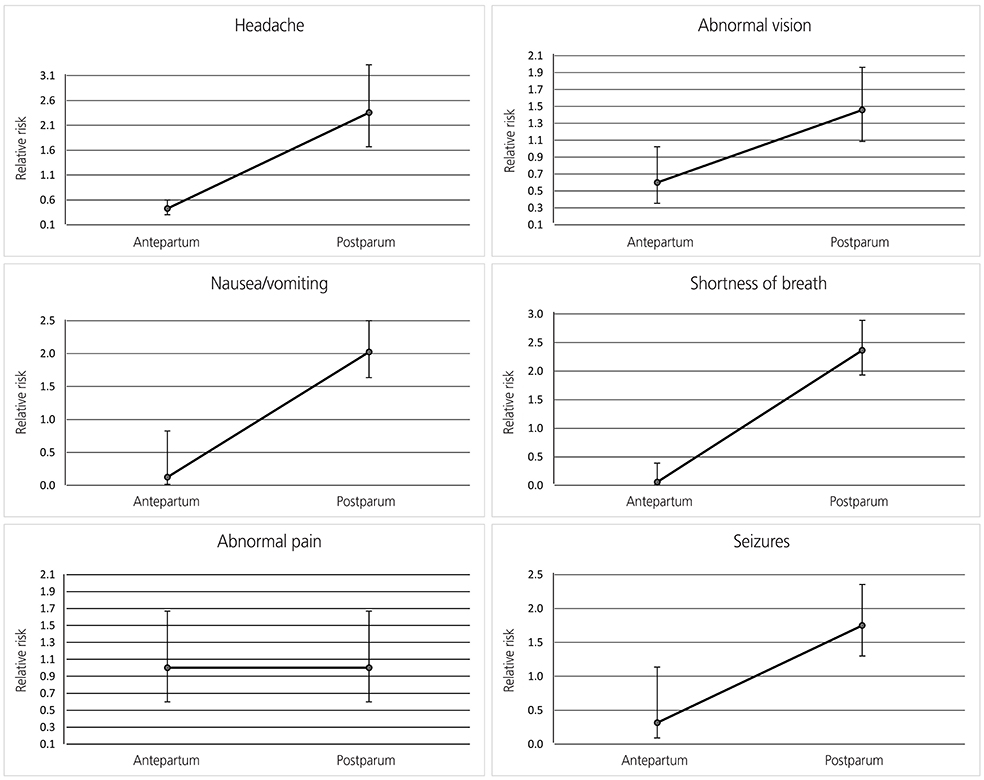
RESULTS
Patients with antepartum preeclampsia and new-onset postpartum preeclampsia differ significantly in profile, symptoms at presentation, laboratory markers and pregnancy outcomes.
CONCLUSION
New-onset postpartum preeclampsia has a distinct patient profile and clinical presentation than antepartum preeclampsia, suggesting they may represent different disorders. Characterization of a patient profile with increased risk of developing this condition will help clinicians to identify patients at risk and provide early and targeted interventions to decrease the morbidity associated with this condition.
MeSH Terms
Figure
Reference
-
1. Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006; 367:1066–1074.2. Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009; 33:130–137.3. Tan LK, de Swiet M. The management of postpartum hypertension. BJOG. 2002; 109:733–736.4. Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002; 186:1174–1177.5. Filetti LC, Imudia AN, Al-Safi Z, Hobson DT, Awonuga AO, Bahado-Singh RO. New onset delayed postpartum preeclampsia: different disorders? J Matern Fetal Neonatal Med. 2012; 25:957–960.6. Sibai BM. Etiology and management of postpartum hypertension-preeclampsia. Am J Obstet Gynecol. 2012; 206:470–475.7. Clark SL, Belfort MA, Dildy GA, Englebright J, Meints L, Meyers JA, et al. Emergency department use during the postpartum period: implications for current management of the puerperium. Am J Obstet Gynecol. 2010; 203:38.e1–38.e6.8. Leitch CR, Cameron AD, Walker JJ. The changing pattern of eclampsia over a 60-year period. Br J Obstet Gynaecol. 1997; 104:917–922.9. Andrus SS, Wolfson AB. Postpartum preeclampsia occurring after resolution of antepartum preeclampsia. J Emerg Med. 2010; 38:168–170.10. Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004; 190:1464–1466.11. Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Obstet Gynecol. 2011; 118:1102–1107.12. Vilchez G, Londra L, Hoyos LR, Sokol R, Bahado-Singh R. Intrapartum mean platelet volume is not a useful predictor of new-onset delayed postpartum pre-eclampsia. Int J Gynaecol Obstet. 2015; 131:59–62.13. ACOG Committee on Practice Bulletins: Obstetrics. ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. Obstet Gynecol. 2002; January. 99:159–167.14. Yancey LM, Withers E, Bakes K, Abbott J. Postpartum preeclampsia: emergency department presentation and management. J Emerg Med. 2011; 40:380–384.15. Larsen WI, Strong JE, Farley JH. Risk factors for late postpartum preeclampsia. J Reprod Med. 2012; 57:35–38.16. Vilchez G, Chelliah A, Argoti P, Jeelani R, Bahado-Singh R. Maternal race and neonatal outcomes after elective repeat cesarean delivery. J Matern Fetal Neonatal Med. 2014; 27:368–371.17. Vilchez G, Dai J, Gill N, Lagos M, Bahado-Singh R, Sokol RJ. Racial disparities in the optimal for induction of labor in low-risk term pregnancies: a national population-based study. J Matern Fetal Neonatal Med. 2016; 29:1279–1282.18. Podymow T, August P. Postpartum course of gestational hypertension and preeclampsia. Hypertens Pregnancy. 2010; 29:294–300.19. Atterbury JL, Groome LJ, Hoff C. Blood pressure changes in normotensive women readmitted in the postpartum period with severe preeclampsia/eclampsia. J Matern Fetal Med. 1996; 5:201–205.20. Atterbury JL, Groome LJ, Hoff C, Yarnell JA. Clinical presentation of women readmitted with postpartum severe preeclampsia or eclampsia. J Obstet Gynecol Neonatal Nurs. 1998; 27:134–141.21. Wolfe DS, Williams SF, Ross MG, Beall MH, Apuzzio JJ. Does preeclampsia predict the risk of late postpartum eclampsia? AJP Rep. 2013; 3:13–16.22. Boriboonhirunsarn D, Atisook R, Taveethamsathit T. Mean platelet volume of normal pregnant women and severe preeclamptic women in Siriraj Hospital. J Med Assoc Thai. 1995; 78:586–589.23. Dundar O, Yoruk P, Tutuncu L, Erikci AA, Muhcu M, Ergur AR, et al. Longitudinal study of platelet size changes in gestation and predictive power of elevated MPV in development of pre-eclampsia. Prenat Diagn. 2008; 28:1052–1056.24. Järemo P, Lindahl TL, Lennmarken C, Forsgren H. The use of platelet density and volume measurements to estimate the severity of pre-eclampsia. Eur J Clin Invest. 2000; 30:1113–1118.25. Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol. 2003; 102:181–192.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Increased carboxyhemoglobin and serum iron concentration as an indicator of increased red cell turnover in preeclampsia
- Anesthetic management for preeclampsia: Hemodynamic monitoring and volume therapy
- A study to compare maternal and perinatal outcome in early vs. late onset preeclampsia
- The Plasma Level of Matrix Metalloproteinase (MMP)-2, -9 between Antepartum and Postpartum Period in Preeclampsia
- The Significance of Plasma Homocysteine Level in Pregnant Women with Severe Preeclampsia