Urogenit Tract Infect.
2017 Apr;12(1):15-21. 10.14777/uti.2017.12.1.15.
Chronic Prostatitis/Chronic Pelvic Pain Syndrome and Male Bladder Pain Syndrome/Interstitial Cystitis: How Are They Related?
- Affiliations
-
- 1Department of Urology, Kangwon National University School of Medicine, Chuncheon, Korea. paulee@kangwon.ac.kr
- KMID: 2378144
- DOI: http://doi.org/10.14777/uti.2017.12.1.15
Abstract
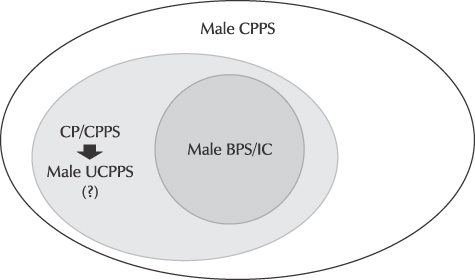
- To date, the heterogeneous pathophysiology of chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) and bladder pain syndrome/interstitial cystitis (BPS/IC) has not been fully elucidated. Thus, it is difficult to make a full comparison between CP/CPPS and male BPS/IC. Controversy and confusion surrounding the terminologies and classifications of CP/CPPS and BPS/IC complicates the issue. CP/CPPS and male BPS/IC are not mutually exclusive conditions, in that they have similarities in their pathogenesis and clinical presentation. Based on the working definitions of these terms, it would be correct to say that male BPS/IC is subsumed by CP/CPPS, and that male BPS/IC can be regarded as CP/CPPS with clear bladder-specific features. Although the term CP/CPPS may be inappropriate, especially since "CP" may be misleading, the perspective that CP/CPPS and male BPS/IC are male urological chronic pain syndromes could enhance the understanding of the relationship between the two. The European Association of Urology classification for chronic pelvic pain is systematic and corresponds well with our knowledge of chronic pain. Therefore, this classification might be the solution to the problems associated with the existing terminologies and taxonomy of CP/CPPS and BPS/IC. In the management of urological chronic pelvic pain in men, clinical phenotyping systems (the UPOINT or UPOINTs system) profile patients and indicate how tailored treatment could be achieved as individualized, multimodal therapeutic regimens. It would be prudent to include bladder-specific features, such as painful filling or painful urgency, in the criteria for the organ-specific domain of the UPOINT(s) system.
Keyword
MeSH Terms
Figure
Reference
-
1. Forrest JB, Nickel JC, Moldwin RM. Chronic prostatitis/chronic pelvic pain syndrome and male interstitial cystitis: enigmas and opportunities. Urology. 2007; 69:4 Suppl. 60–63.
Article2. Forrest JB, Vo Q. Observations on the presentation, diagnosis, and treatment of interstitial cystitis in men. Urology. 2001; 57:6 Suppl 1. 26–29.
Article3. Clemens JQ, Meenan RT, Rosetti MC, Gao SY, Calhoun EA. Prevalence and incidence of interstitial cystitis in a managed care population. J Urol. 2005; 173:98–102.
Article4. Forrest JB, Schmidt S. Interstitial cystitis, chronic nonbacterial prostatitis and chronic pelvic pain syndrome in men: a common and frequently identical clinical entity. J Urol. 2004; 172:2561–2562.
Article5. Suskind AM, Berry SH, Ewing BA, Elliott MN, Suttorp MJ, Clemens JQ. The prevalence and overlap of interstitial cystitis/bladder pain syndrome and chronic prostatitis/chronic pelvic pain syndrome in men: results of the RAND Interstitial Cystitis Epidemiology male study. J Urol. 2013; 189:141–145.
Article6. Arora HC, Shoskes DA. The enigma of men with interstitial cystitis/bladder pain syndrome. Transl Androl Urol. 2015; 4:668–676.7. Parsons CL, Rosenberg MT, Sassani P, Ebrahimi K, Koziol JA, Zupkas P. Quantifying symptoms in men with interstitial cystitis/prostatitis, and its correlation with potassium-sensitivity testing. BJU Int. 2005; 95:86–90.
Article8. Hanno P, Lin A, Nordling J, Nyberg L, van Ophoven A, Ueda T, et al. Bladder pain syndrome international consultation on incontinence. Neurourol Urodyn. 2010; 29:191–198.
Article9. Magistro G, Wagenlehner FM, Grabe M, Weidner W, Stief CG, Nickel JC. Contemporary management of chronic prostatitis/chronic pelvic pain syndrome. Eur Urol. 2016; 69:286–297.
Article10. Hanno P, Andersson KE, Birder L, Elneil S, Kanai A, Pontari M. Chronic pelvic pain syndrome/bladder pain syndrome: taking stock, looking ahead: ICI-RS 2011. Neurourol Urodyn. 2012; 31:375–383.
Article11. Janicki TI. Chronic pelvic pain as a form of complex regional pain syndrome. Clin Obstet Gynecol. 2003; 46:797–803.
Article12. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999; 282:236–237.
Article13. Nickel JC. Inflammatory and pain conditions of the male genitourinary tract. In : Wein AJ, Kavoussi LR, Partin AW, Peters C, Campbell MF, Walsh PC, editors. Campbell-Walsh urology. 11th ed. Philadelphia: Elsevier;2016. p. 304–329.14. Shoskes DA, Landis JR, Wang Y, Nickel JC, Zeitlin SI, Nadler R; Chronic Prostatitis Collaborative Research Network Study Group. Impact of post-ejaculatory pain in men with category III chronic prostatitis/chronic pelvic pain syndrome. J Urol. 2004; 172:542–547.
Article15. Engeler D, Baranowski AP, Borovicka J, Cottrell A, Dinis-Oliveira P, Elneil S, et al. The European Association of Urology. Guidelines on chronic pelvic pain [Internet]. Available from: http://uroweb.org/wp-content/uploads/EAU-Guidelines-Chronic-Pelvic-Pain-2015.pdf.16. Shoskes DA, Katz E. Multimodal therapy for chronic prostatitis/chronic pelvic pain syndrome. Curr Urol Rep. 2005; 6:296–299.
Article17. Shoskes DA, Nickel JC, Dolinga R, Prots D. Clinical phenotyping of patients with chronic prostatitis/chronic pelvic pain syndrome and correlation with symptom severity. Urology. 2009; 73:538–542.
Article18. van de Merwe JP, Nordling J, Bouchelouche P, Bouchelouche K, Cervigni M, Daha LK, et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal. Eur Urol. 2008; 53:60–67.
Article19. Hanno PM. Bladder pain syndrome (interstitial cystitis) and related disorders. In : Wein AJ, Kavoussi LR, Partin AW, Peters C, Campbell MF, Walsh PC, editors. Campbell-Walsh urology. 11th ed. Philadelphia: Elsevier;2016. p. 334–370.20. Hanno PM. Re-imagining interstitial cystitis. Urol Clin North Am. 2008; 35:91–99.
Article21. Hanno PM, Burks DA, Clemens JQ, Dmochowski RR, Erickson D, Fitzgerald MP, et al. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol. 2011; 185:2162–2170.
Article22. Pontari MA. Chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: are they related? Curr Urol Rep. 2006; 7:329–334.
Article23. Eisenberg ER, Moldwin RM. Etiology: where does prostatitis stop and interstitial cystitis begin? World J Urol. 2003; 21:64–69.
Article24. Parsons CL. Prostatitis, interstitial cystitis, chronic pelvic pain, and urethral syndrome share a common pathophysiology: lower urinary dysfunctional epithelium and potassium recycling. Urology. 2003; 62:976–982.
Article25. Schaeffer AJ, Landis JR, Knauss JS, Propert KJ, Alexander RB, Litwin MS, et al. Demographic and clinical characteristics of men with chronic prostatitis: the national institutes of health chronic prostatitis cohort study. J Urol. 2002; 168:593–598.
Article26. Lai HH, Krieger JN, Pontari MA, Buchwald D, Hou X, Landis JR. MAPP Research Network. Painful bladder filling and painful urgency are distinct characteristics in men and women with urological chronic pelvic pain syndromes: a MAPP research network study. J Urol. 2015; 194:1634–1641.
Article27. Samplaski MK, Li J, Shoskes DA. Clustering of UPOINT domains and subdomains in men with chronic prostatitis/chronic pelvic pain syndrome and contribution to symptom severity. J Urol. 2012; 188:1788–1793.
Article28. Nickel JC, Shoskes D, Irvine-Bird K. Clinical phenotyping of women with interstitial cystitis/painful bladder syndrome: a key to classification and potentially improved management. J Urol. 2009; 182:155–160.
Article29. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178.
Article30. Homma Y. Hypersensitive bladder: a solution to confused terminology and ignorance concerning interstitial cystitis. Int J Urol. 2014; 21:Suppl 1. 43–47.
Article31. Kim SH, Oh SA, Oh SJ. Voiding diary might serve as a useful tool to understand differences between bladder pain syndrome/interstitial cystitis and overactive bladder. Int J Urol. 2014; 21:179–183.
Article32. Homma Y, Ueda T, Tomoe H, Lin AT, Kuo HC, Lee MH, et al. Clinical guidelines for interstitial cystitis and hypersensitive bladder updated in 2015. Int J Urol. 2016; 23:542–549.
Article33. Kuo HC. Potential urine and serum biomarkers for patients with bladder pain syndrome/interstitial cystitis. Int J Urol. 2014; 21:Suppl 1. 34–41.
Article34. Ueda T, Nakagawa M, Okamura M, Tanoue H, Yoshida H, Yoshimura N. New cystoscopic diagnosis for interstitial cystitis/painful bladder syndrome using narrow-band imaging system. Int J Urol. 2008; 15:1039–1043.
Article35. Fall M, Johansson SL, Aldenborg F. Chronic interstitial cystitis: a heterogeneous syndrome. J Urol. 1987; 137:35–38.
Article36. Nordling J, Fall M, Hanno P. Global concepts of bladder pain syndrome (interstitial cystitis). World J Urol. 2012; 30:457–464.
Article37. Shoskes DA, Nickel JC, Rackley RR, Pontari MA. Clinical phenotyping in chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: a management strategy for urologic chronic pelvic pain syndromes. Prostate Cancer Prostatic Dis. 2009; 12:177–183.
Article38. Shoskes DA, Nickel JC, Kattan MW. Phenotypically directed multimodal therapy for chronic prostatitis/chronic pelvic pain syndrome: a prospective study using UPOINT. Urology. 2010; 75:1249–1253.
Article39. Trinchieri A, Magri V, Cariani L, Bonamore R, Restelli A, Garlaschi MC, et al. Prevalence of sexual dysfunction in men with chronic prostatitis/chronic pelvic pain syndrome. Arch Ital Urol Androl. 2007; 79:67–70.40. Lee SW, Liong ML, Yuen KH, Leong WS, Cheah PY, Khan NA, et al. Adverse impact of sexual dysfunction in chronic prostatitis/chronic pelvic pain syndrome. Urology. 2008; 71:79–84.
Article41. Mehik A, Hellstrom P, Sarpola A, Lukkarinen O, Jarvelin MR. Fears, sexual disturbances and personality features in men with prostatitis: a population-based cross-sectional study in Finland. BJU Int. 2001; 88:35–38.
Article42. Magri V, Wagenlehner F, Perletti G, Schneider S, Marras E, Naber KG, et al. Use of the UPOINT chronic prostatitis/chronic pelvic pain syndrome classification in European patient cohorts: sexual function domain improves correlations. J Urol. 2010; 184:2339–2345.
Article43. Davis SN, Binik YM, Amsel R, Carrier S. Is a sexual dysfunction domain important for quality of life in men with urological chronic pelvic pain syndrome? Signs “UPOINT” to yes. J Urol. 2013; 189:146–151.
Article44. Samplaski MK, Li J, Shoskes DA. Inclusion of erectile domain to UPOINT phenotype does not improve correlation with symptom severity in men with chronic prostatitis/chronic pelvic pain syndrome. Urology. 2011; 78:653–658.
Article45. Fall M, Baranowski AP, Fowler CJ, Lepinard V, Malone-Lee JG, Messelink EJ, et al. EAU guidelines on chronic pelvic pain. Eur Urol. 2004; 46:681–689.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Urethral Pain Syndrome Really Part of Bladder Pain Syndrome?
- Update on the Pathology and Diagnosis of Interstitial Cystitis/Bladder Pain Syndrome: A Review
- Combined Use of Duloxetine and Olanzapine in the Treatment of Urologic Chronic Pelvic Pain Syndromes Refractory to Conventional Treatment: A Case Report
- Clinical Approach to Recurrent Voiding Dysfunction, Dysuria, and Pelvic Pain Persisting for at Least 3 Months
- UPOINT System: A Diagnostic/Therapeutic Algorithm for Chronic Prostatitis/Chronic Pelvic Pain Syndrome