J Rheum Dis.
2017 Apr;24(2):108-113. 10.4078/jrd.2017.24.2.108.
Rivaroxaban for Thromboprophylaxis in Patients with Antiphospholipid Syndrome
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea. beconst@hanmail.net
- KMID: 2378089
- DOI: http://doi.org/10.4078/jrd.2017.24.2.108
Abstract
- The main treatment for Antiphospholipid syndrome (APS) is long-term anticoagulation with an oral vitamin K antagonist, although these are associated with numerous problems. Rivaroxaban is a direct anti-factor Xa inhibitor, with a predictable anticoagulant effect at fixed doses. There are limited reports of rivaroxaban use in APS. We present four cases of patients with APS who received rivaroxaban treatment for six months without thrombosis recurrence or bleeding. Three of the patients received rivaroxaban as initial therapy. In the systematic review, only five patients were treated with rivaroxaban as a thromboprophylaxis. Of the 71 cases of rivaroxaban use including our study, there were seven cases (9.9%) of thrombosis recurrence and two reports of bleeding. The efficacy of rivaroxaban in APS patients was at least equal to warfarin therapy. This report and systematic review suggest that rivaroxaban can be considered cautiously as a thromboprophylactic or alternative therapy for warfarin in patients with APS.
Keyword
MeSH Terms
Figure
Reference
-
1. Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite anti-phospholipid syndrome (APS). J Thromb Haemost. 2006; 4:295–306.
Article2. Ruiz-Irastorza G, Cuadrado MJ, Ruiz-Arruza I, Brey R, Crowther M, Derksen R, et al. Evidence-based recommendations for the prevention and long-term management of thrombosis in antiphospholipid antibody-positive patients: report of a task force at the 13th International Congress on antiphospholipid antibodies. Lupus. 2011; 20:206–18.
Article3. Erkan D, Aguiar CL, Andrade D, Cohen H, Cuadrado MJ, Danowski A, et al. 14th International Congress on Antiphospholipid Antibodies: task force report on anti-phospholipid syndrome treatment trends. Autoimmun Rev. 2014; 13:685–96.
Article4. EINSTEIN Investigators, Bauersachs R, Berkowitz SD, Brenner B, Buller HR, Decousus H, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010; 363:2499–510.
Article5. EINSTEIN– PE, Büller HR, Prins MH, Lensin AW, Decousus H, Jacobson BF, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012; 366:1287–97.
Article6. Schaefer JK, McBane RD, Black DF, Williams LN, Moder KG, Wysokinski WE. Failure of dabigatran and rivaroxaban to prevent thromboembolism in antiphospholipid syndrome: a case series of three patients. Thromb Haemost. 2014; 112:947–50.
Article7. Win K, Rodgers GM. New oral anticoagulants may not be effective to prevent venous thromboembolism in patients with antiphospholipid syndrome. Am J Hematol. 2014; 89:1017.
Article8. Cohen H, Doré CJ, Clawson S, Hunt BJ, Isenberg D, Khamashta M, et al. Rivaroxaban in antiphospholipid syndrome (RAPS) protocol: a prospective, randomized controlled phase II/III clinical trial of rivaroxaban versus warfarin in patients with thrombotic antiphospholipid syndrome, with or without SLE. Lupus. 2015; 24:1087–94.
Article9. Bayer Pharma AG. XareltoⓇ Summary of product characteristics [Internet]. Berlin: Bayer HealthCare Pharmaceuticals;2015. May [cited 2016 Aug 24]. Available from:. https://www.xarelto.com/static/media/pdf/BHC-Xar-SPC-May-2015-LAY03.xml.10. Bachmeyer C, Elalamy I. Rivaroxaban as an effective treatment for recurrent superficial thrombophlebitis related to primary antiphospholipid syndrome. Clin Exp Dermatol. 2014; 39:840–1.
Article11. Son M, Wypasek E, Celinska-Lowenhoff M, Undas A. The use of rivaroxaban in patients with antiphospholipid syndrome: A series of 12 cases. Thromb Res. 2015; 135:1035–6.
Article12. Sciascia S, Breen K, Hunt BJ. Rivaroxaban use in patients with antiphospholipid syndrome and previous venous thromboembolism. Blood Coagul Fibrinolysis. 2015; 26:476–7.13. Noel N, Dutasta F, Costedoat-Chalumeau N, Bienvenu B, Mariette X, Geffray L, et al. Safety and efficacy of oral direct inhibitors of thrombin and factor Xa in antiphospholipid syndrome. Autoimmun Rev. 2015; 14:680–5.
Article14. Crowther MA, Ginsberg JS, Julian J, Denburg J, Hirsh J, Douketis J, et al. A comparison of two intensities of warfarin for the prevention of recurrent thrombosis in patients with the antiphospholipid antibody syndrome. N Engl J Med. 2003; 349:1133–8.
Article15. Finazzi G, Marchioli R, Brancaccio V, Schinco P, Wisloff F, Musial J, et al. A randomized clinical trial of high-intensity warfarin vs. conventional antithrombotic therapy for the prevention of recurrent thrombosis in patients with the antiphospholipid syndrome (WAPS). J Thromb Haemost. 2005; 3:848–53.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antiphospholipid Antibody Syndrome
- Flank ulcer in a patient with primary antiphospholipid syndrome
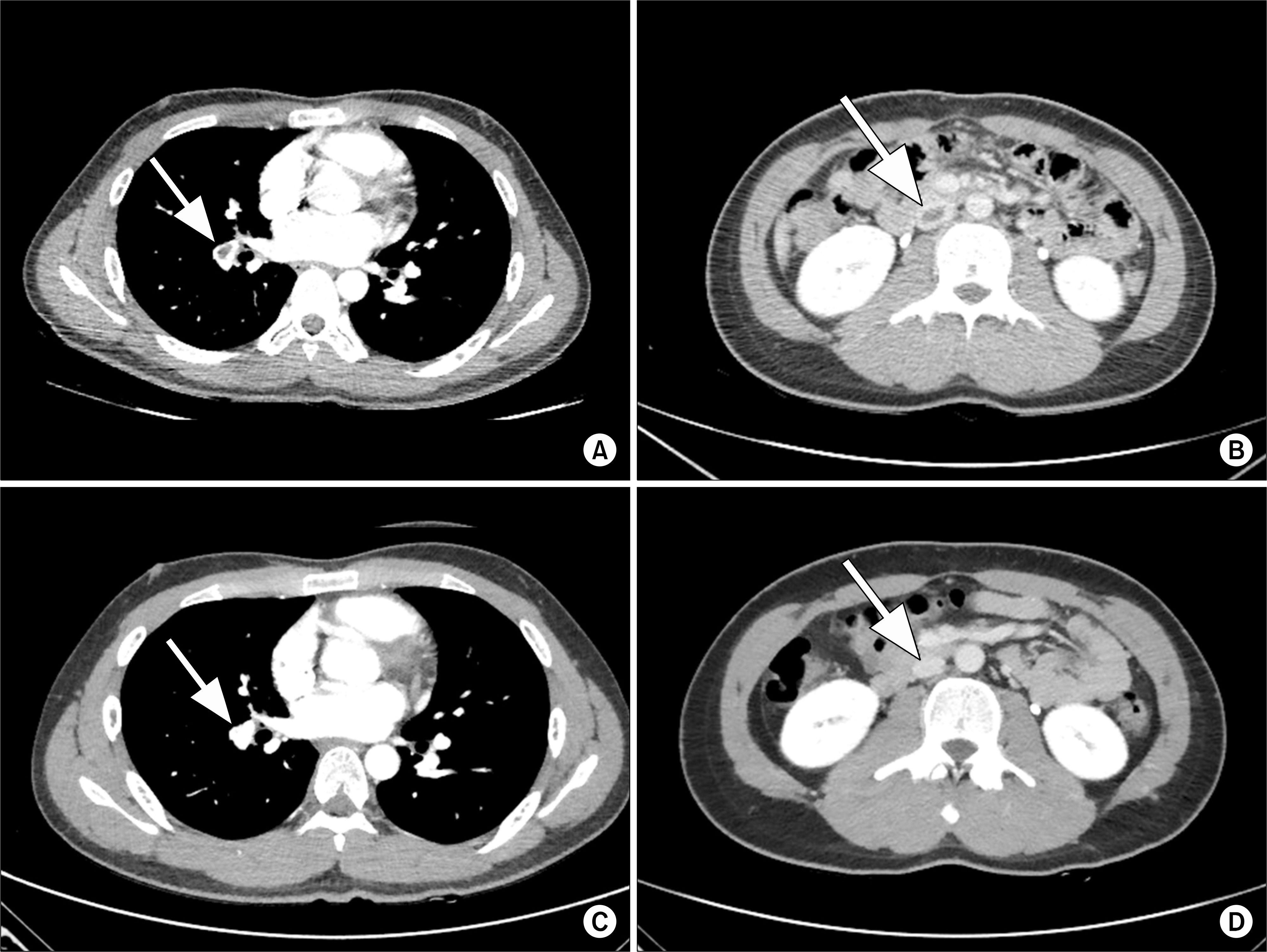
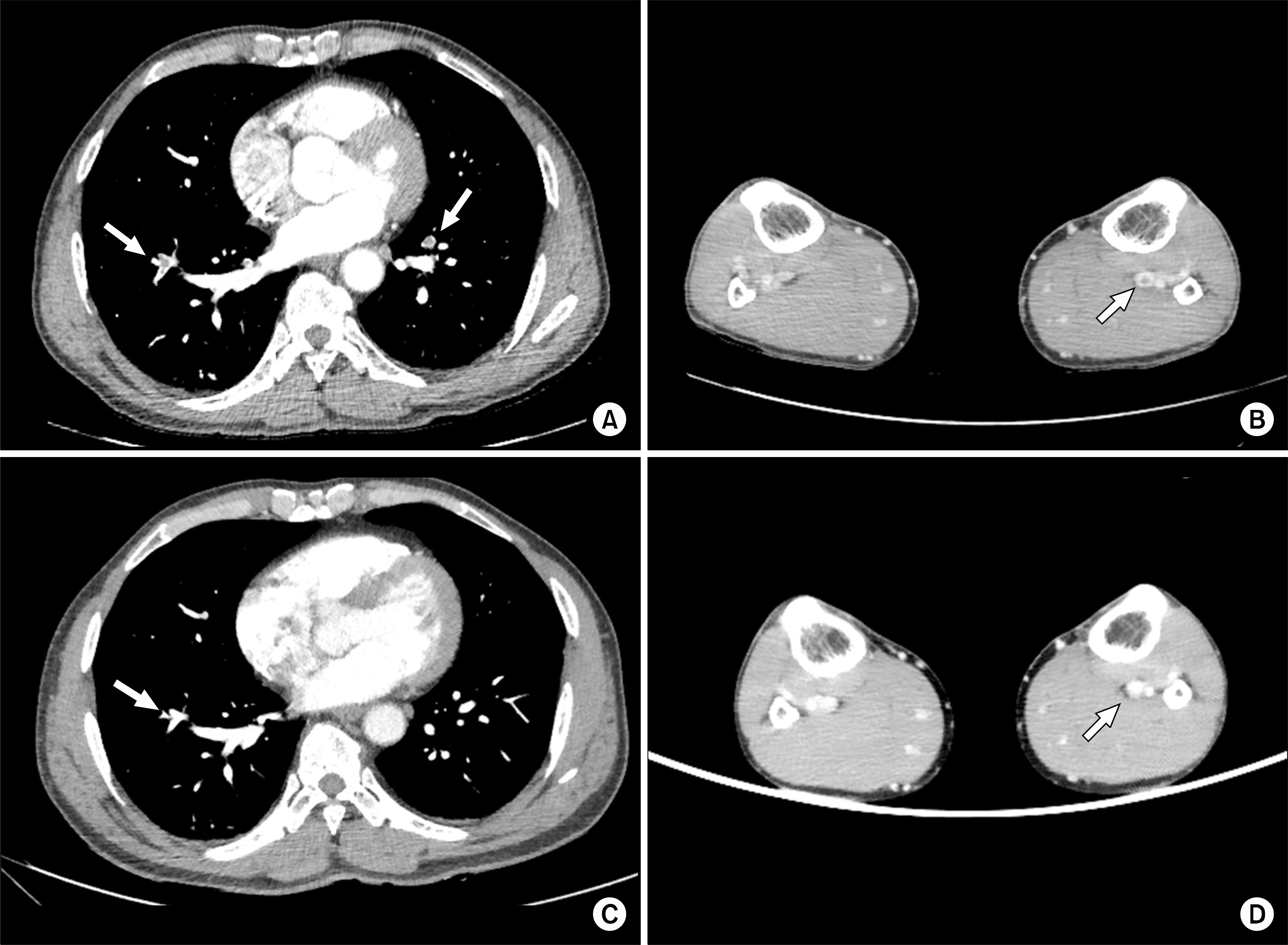
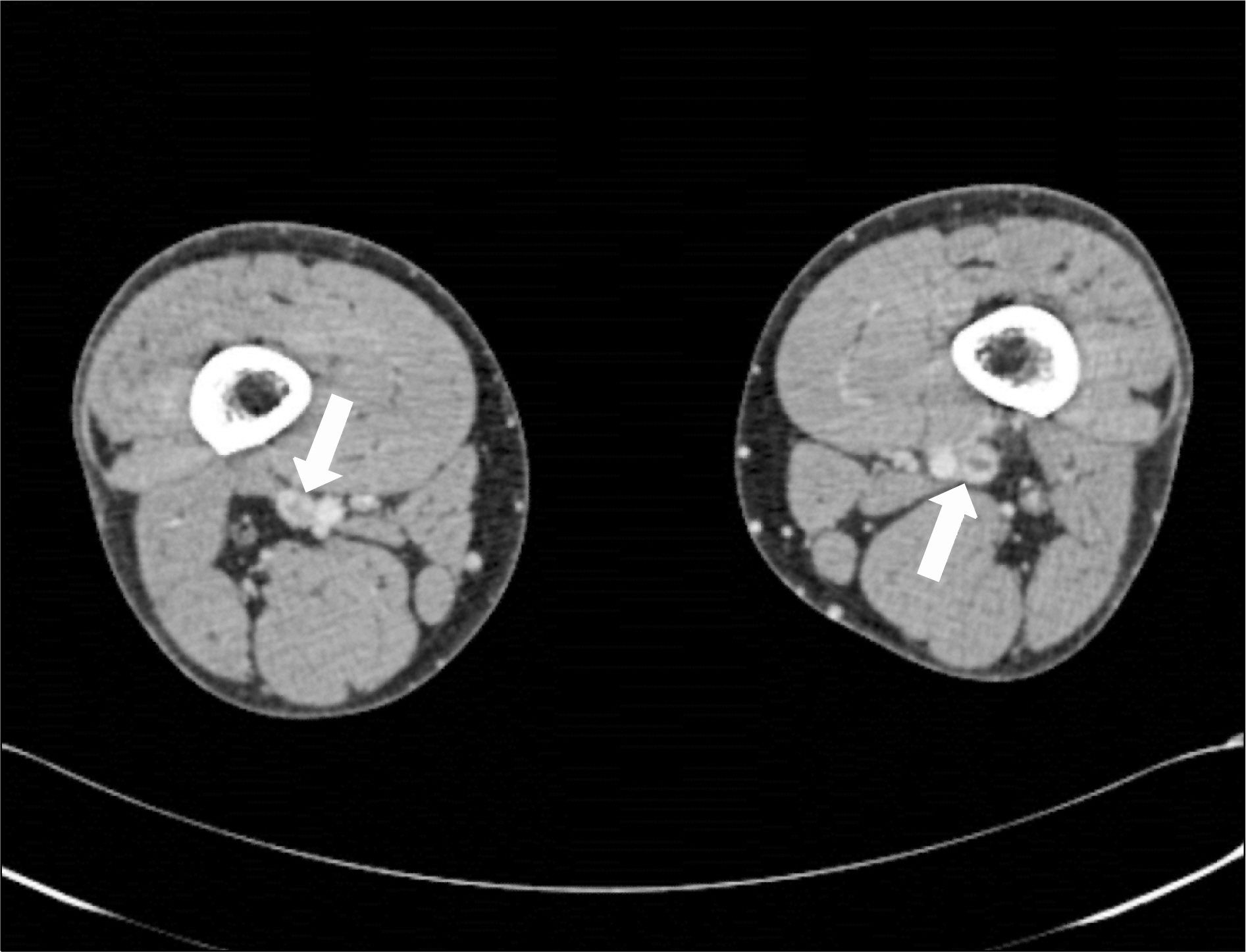
- Antiphospholipid Syndrome Associated with Adenocarcinoma
- A case of Limited Scleroderma Associated with Antiphospholipid Syndrome
- A patient with chorea associated with hyperthyroidism and primary antiphospholipid antibody syndrome