J Cerebrovasc Endovasc Neurosurg.
2017 Mar;19(1):12-18. 10.7461/jcen.2017.19.1.12.
Prophylactic Dual Catheter Technique to Prevent Side Branch Snowplowing Complications during Angioplasty and Stenting
- Affiliations
-
- 1Division of Neurology, Department of Medicine, National University Health System, Singapore.
- 2Division of Neuroradiology, Department of Medical Imaging and Intervention, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan. hfwong@cgmh.org.tw
- 3College of Medicine and School of Medical Technology, Chang Gung University, Taoyuan, Taiwan.
- KMID: 2377622
- DOI: http://doi.org/10.7461/jcen.2017.19.1.12
Abstract
OBJECTIVE
Angioplasty and Stenting of intracranial atherosclerotic lesions have a higher complication rate and a large proportion of this is attributable to side branch arterial occlusion from forceful displacement of the atheroma into the ostia or snowplowing effect. This can result in severe disabilities when it result in small infarcts involving eloquent areas in the posterior circulation or the motor tracts.
MATERIALS AND METHODS
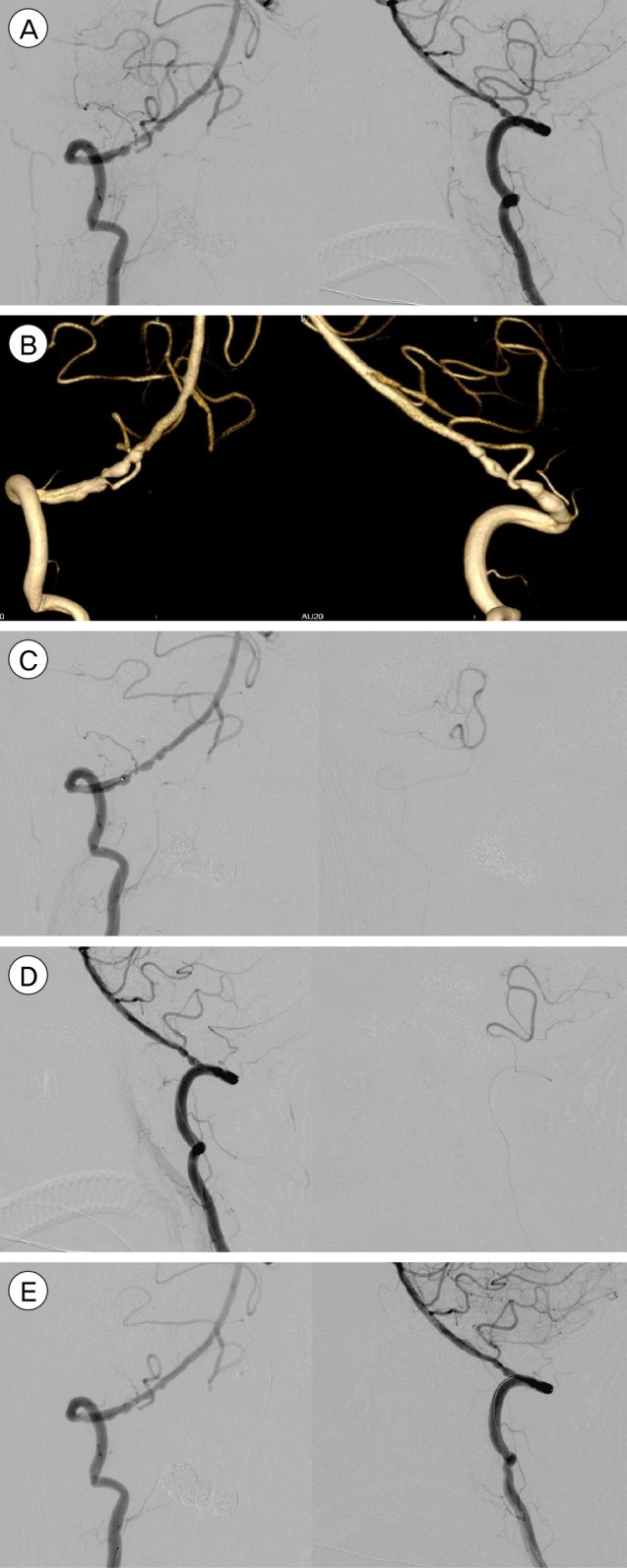
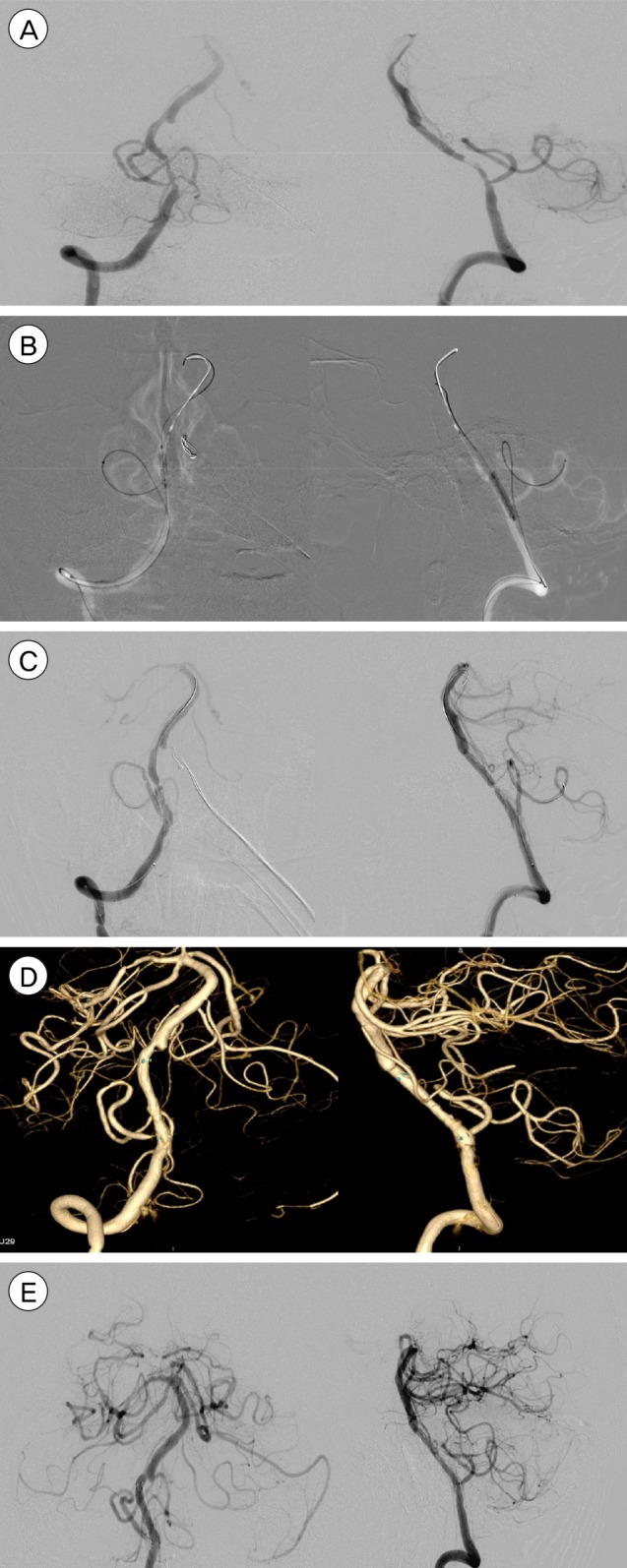
We present a series of 6 cases utilizing a new dual catheter technique for maintaining the patency of at-risk vessels during angioplasty and stenting. There are several methods previously described to help reduce the incidence of stroke but because they do not have a physical presence in the ostia to protect it, they are unable to guarantee the patency of the vessel.
RESULTS
All 6 patients underwent angioplasty and stenting with the technique. The patients were assessed for complications with post-procedure magnetic resonance imaging and no complications were found.
CONCLUSION
In this preliminary series, the dual catheter technique appears to safe and effective in preventing occlusion of the adjacent branch arteries. This technique may facilitate the use of the Wingspan stent in the treatment of intracranial atherosclerotic stenotic segments by reducing the risk of peri-procedural stroke.
Keyword
MeSH Terms
Figure
Reference
-
1. Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011; 9. 365(11):993–1003. PMID: 21899409.2. Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005; 3. 352(13):1305–1316. PMID: 15800226.
Article3. Henkes H, Miloslavski E, Lowens S, Reinartz J, Liebig T, Kühne D. Treatment of intracranial atherosclerotic stenoses with balloon dilatation and self-expanding stent deployment (WingSpan). Neuroradiology. 2005; 3. 47(3):222–228. PMID: 15912418.
Article4. Jiang WJ, Srivastava T, Gao F, Du B, Dong KH, Xu XT. Perforator stroke after elective stenting of symptomatic intracranial stenosis. Neurology. 2006; 6. 66(12):1868–1872. PMID: 16801652.
Article5. Leung TW, Yu SC, Lam WW, Chan AY, Lau AY, Wong LK. Would self-expanding stent occlude middle cerebral artery perforators? Stroke. 2009; 5. 40(5):1910–1912. PMID: 19182082.
Article6. Levy EI, Chaturvedi S. Perforator stroke following intracranial stenting: a sacrifice for the greater good. Neurology. 2006; 6. 66(12):1803–1804. PMID: 16801640.
Article7. Lopes DK, Ringer AJ, Boulos AS, Qureshi AI, Lieber BB, Guterman LR, et al. Fate of branch arteries after intracranial stenting. Neurosurgery. 2003; 6. 52(6):1275–1278. discussion 1278-9. PMID: 12762872.
Article8. Masuo O, Terada T, Walker G, Tsuura M, Nakai K, Itakura T. Patency of perforating arteries after stent placement? A study using an in vivo experimental atherosclerosis-induced model. Am J Neuroradiol. 2005; 3. 26(3):543–548. PMID: 15760863.9. Nahab F, Cotsonis G, Lynn M, Feldmann E, Chaturvedi S, Hemphill JC, et al. Prevalence and prognosis of coexistent asymptomatic intracranial stenosis. Stroke. 2008; 3. 39(3):1039–1041. PMID: 18239161.
Article10. Nahab F, Lynn MJ, Kasner SE, Alexander MJ, Klucznik R, Zaidat OO, et al. Risk factors associated with major cerebrovascular complications after intracranial stenting. Neurology. 2009; 6. 72(23):2014–2019. PMID: 19299309.
Article11. Poerner TC, Kralev S, Voelker W, Sueselbeck T, Latsch A, Pfleger S, et al. Natural history of small and medium-sized side branches after coronary stent implantation. Am Heart J. 2002; 4. 143(4):627–635. PMID: 11923799.
Article12. Sacco RL, Kargman DE, Gu Q, Zamanillo MC. Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction. The Northern Manhattan Stroke Study. Stroke. 1995; 1. 26(1):14–20. PMID: 7839388.13. Schumacher HC, Khaw AV, Myers PM, Gupta R, Higashida RT. Intracranial angioplasty and stent placement for cerebral atherosclerosis. J Vasc Interv Radiol. 2004; 1. 15(1 Pt 2):S123–S132. PMID: 15101521.
Article14. Umont TM, Sonig A, Mokin M, Eller JL, Sorkin GC, Snyder KV, et al. Submaximal angioplasty for symptomatic intracranial atherosclerosis: a prospective Phase I study. J Neurosurg. 2016; 10. 125(4):964–971. PMID: 26745485.15. Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) Trial Investigators. Design, progress and challenges of a double-blind trial of warfarin versus aspirin for symptomatic intracranial arterial stenosis. Neuroepidemiology. 2003; Mar-Apr. 22(2):106–117. PMID: 12656117.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictors of side branch occlusions just after coronary stenting
- Consecutive Jailed- and Kissing-Corsair Technique: Side Branch Protection and Dilation during Stent Implantation
- Controlled Atrial Fibrillation after Pulmonary Vein Stenting
- Angioplasty at Coronary Bifurcation
- Angioplasty, Stenting and Other Potential Treatments of Atherosclerotic Stenosis of the Intracranial Arteries: Past, Present and Future