World J Mens Health.
2017 Apr;35(1):28-33. 10.5534/wjmh.2017.35.1.28.
Clinicopathologic Characteristics and Treatment Outcomes of Penile Cancer
- Affiliations
-
- 1Department of Urology, Pusan National University Yangsan Hospital, Yangsan, Korea. toughkil76@naver.com
- 2Department of Urology, Gyeongsang National University Hospital, Jinju, Korea.
- 3Department of Urology, Dong-A University Hospital, Busan, Korea.
- 4Department of Urology, Kosin University Gospel Hospital, Busan, Korea.
- 5Department of Urology, Inje University Haeundae Paik Hospital, Busan, Korea.
- 6Department of Urology, Pusan National University Hospital, Busan, Korea.
- KMID: 2377209
- DOI: http://doi.org/10.5534/wjmh.2017.35.1.28
Abstract
- PURPOSE
The aim of this study was to assess the clinicopathologic characteristics of penile cancer, including patterns of therapy, oncologic results, and survival.
MATERIALS AND METHODS
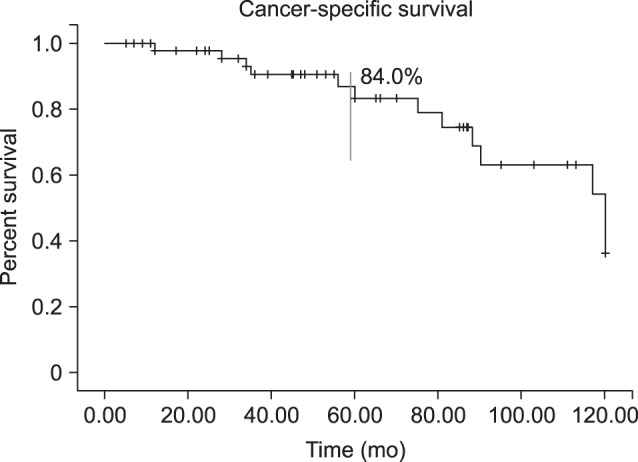
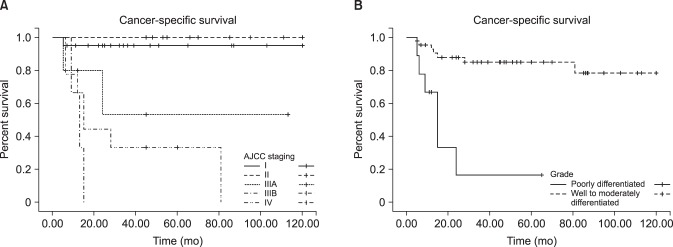
Between January 2005 and July 2015, 71 patients at 6 institutions who had undergone penectomy or penile biopsy were enrolled. Their medical records were reviewed to identify the mode of therapy, pathology reports, and cancer-specific survival (CSS) rate.
RESULTS
Clinicopathologic and outcome information was available for 52 male patients (mean age, 64.3 years; mean follow-up, 61.4 months). At presentation, 17 patients were node-positive, and 4 had metastatic disease. Management was partial penectomy in 34 patients, total penectomy in 12 patients, and chemotherapy or radiotherapy in 6 patients. The pathology reports were squamous cell carcinoma in 50 patients and other types of carcinoma in the remaining 2 patients. Kaplan-Meier survival analysis showed a 5-year CSS rate of 84.0%. In univariate and multivariate analyses, the American Joint Committee on Cancer (AJCC) stage and pathologic grade were associated with survival.
CONCLUSIONS
Partial penectomy was the most common treatment of penile lesions. The oncologic outcomes were good, with a 5-year CSS of 84.0%. The AJCC stage and pathologic grade were independent prognostic factors for survival.
Keyword
MeSH Terms
Figure
Reference
-
1. Chaux A, Netto GJ, Rodríguez IM, Barreto JE, Oertell J, Ocampos S, et al. Epidemiologic profile, sexual history, pathologic features, and human papillomavirus status of 103 patients with penile carcinoma. World J Urol. 2013; 31:861–867. PMID: 22116602.
Article2. Korean Ministry of Health and Welfare & Korean National Cancer Information Center 2015. Cancer in Korea [Internet]. Goyang: National Cancer Center;c2016. cited 2016 Jun 5. Available from: http://www.cancer.go.kr.3. Bleeker MC, Heideman DA, Snijders PJ, Horenblas S, Dillner J, Meijer CJ. Penile cancer: epidemiology, pathogenesis and prevention. World J Urol. 2009; 27:141–150. PMID: 18607597.
Article4. Skeppner E, Andersson SO, Johansson JE, Windahl T. Initial symptoms and delay in patients with penile carcinoma. Scand J Urol Nephrol. 2012; 46:319–325. PMID: 22989150.
Article5. American Joint Committee on Cancer (AJCC). Penis. In : Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 7th ed. New York: Springer;2010. p. 447–455.6. Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB. Cancer incidence in five continents vol. viii. IARC Scientific Publication. Lyon: International Agency for Research on Cancer;2002. p. 93–514.7. Morris BJ, Gray RH, Castellsague X, Bosch FX, Halperin DT, Waskett JH, et al. The strong protective effect of circumcision against cancer of the penis. Adv Urol. 2011; DOI: 10.1155/2011/812368.
Article8. Van Howe RS, Hodges FM. The carcinogenicity of smegma: debunking a myth. J Eur Acad Dermatol Venereol. 2006; 20:1046–1054. PMID: 16987256.
Article9. Daling JR, Madeleine MM, Johnson LG, Schwartz SM, Shera KA, Wurscher MA, et al. Penile cancer: importance of circumcision, human papillomavirus and smoking in in situ and invasive disease. Int J Cancer. 2005; 116:606–616. PMID: 15825185.10. Archier E, Devaux S, Castela E, Gallini A, Aubin F, Le Maître M, et al. Carcinogenic risks of psoralen UV-A therapy and narrowband UV-B therapy in chronic plaque psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012; 26(Suppl 3):22–31. PMID: 22512677.
Article11. Lau WD, Ong CH, Lim TP, Teo C. Penile cancer: a local case series and literature review. Singapore Med J. 2015; 56:637–640. PMID: 26668410.12. Cubilla AL. The role of pathologic prognostic factors in squamous cell carcinoma of the penis. World J Urol. 2009; 27:169–177. PMID: 18766352.
Article13. Lopes A, Hidalgo GS, Kowalski LP, Torloni H, Rossi BM, Fonseca FP. Prognostic factors in carcinoma of the penis: multivariate analysis of 145 patients treated with amputation and lymphadenectomy. J Urol. 1996; 156:1637–1642. PMID: 8863559.
Article14. Ornellas AA, Kinchin EW, Nóbrega BL, Wisnescky A, Koifman N, Quirino R. Surgical treatment of invasive squamous cell carcinoma of the penis: Brazilian National Cancer Institute long-term experience. J Surg Oncol. 2008; 97:487–495. PMID: 18425779.
Article15. Diorio GJ, Leone AR, Spiess PE. Management of penile cancer. Urology. 2016; 96:15–21. PMID: 26802797.
Article16. Ravi R. Correlation between the extent of nodal involvement and survival following groin dissection for carcinoma of the penis. Br J Urol. 1993; 72:817–819. PMID: 8281416.
Article17. Graafland NM, Lam W, Leijte JA, Yap T, Gallee MP, Corbishley C, et al. Prognostic factors for occult inguinal lymph node involvement in penile carcinoma and assessment of the high-risk EAU subgroup: a two-institution analysis of 342 clinically node-negative patients. Eur Urol. 2010; 58:742–747. PMID: 20800339.
Article18. Coblentz TR, Theodorescu D. Morbidity of modified prophylactic inguinal lymphadenectomy for squamous cell carcinoma of the penis. J Urol. 2002; 168:1386–1389. PMID: 12352399.
Article19. Bouchot O, Rigaud J, Maillet F, Hetet JF, Karam G. Morbidity of inguinal lymphadenectomy for invasive penile carcinoma. Eur Urol. 2004; 45:761–765. PMID: 15149749.
Article20. Kroon BK, Horenblas S, Lont AP, Tanis PJ, Gallee MP, Nieweg OE. Patients with penile carcinoma benefit from immediate resection of clinically occult lymph node metastases. J Urol. 2005; 173:816–819. PMID: 15711276.
Article21. Mikhail GR. Cancers, precancers, and pseudocancers on the male genitalia. A review of clinical appearances, histopathology, and management. J Dermatol Surg Oncol. 1980; 6:1027–1035. PMID: 6259230.
Article22. Austoni E, Fenice O, Kartalas Goumas Y, Colombo F, Mantovani F, Pisani E. New trends in the surgical treatment of penile carcinoma. Arch Ital Urol Androl. 1996; 68:163–168.23. Gulino G, Sasso F, Falabella R, Bassi PF. Distal urethral reconstruction of the glans for penile carcinoma: results of a novel technique at 1-year of followup. J Urol. 2007; 178:941–944. PMID: 17632177.
Article24. O'Kane HF, Pahuja A, Ho KJ, Thwaini A, Nambirajan T, Keane P. Outcome of glansectomy and skin grafting in the management of penile cancer. Adv Urol. 2011; DOI: 10.1155/2011/240824.25. Morelli G, Pagni R, Mariani C, Campo G, Menchini-Fabris F, Minervini R, et al. Glansectomy with split-thickness skin graft for the treatment of penile carcinoma. Int J Impot Res. 2009; 21:311–314. PMID: 19458620.
Article26. Palminteri E, Berdondini E, Lazzeri M, Mirri F, Barbagli G. Resurfacing and reconstruction of the glans penis. Eur Urol. 2007; 52:893–898. PMID: 17275169.
Article27. Smith Y, Hadway P, Biedrzycki O, Perry MJ, Corbishley C, Watkin NA. Reconstructive surgery for invasive squamous carcinoma of the glans penis. Eur Urol. 2007; 52:1179–1185. PMID: 17349734.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Metastatic Penile Cancer Originated from Pancreas
- Third-generation Cryosurgery for Prostate Cancer Patient with a Penile Prosthesis
- Penile necrosis after penile prosthesis implantation
- One Staged Urethroplasty Using Bilateral Penile Pedicled Rotation Skin-flaps in the Proximal Penile Shaft Hypospadias with Insufficient Penile Skin
- Secondary penile carcinoma originated from pancreas