J Korean Fract Soc.
2017 Apr;30(2):75-82. 10.12671/jkfs.2017.30.2.75.
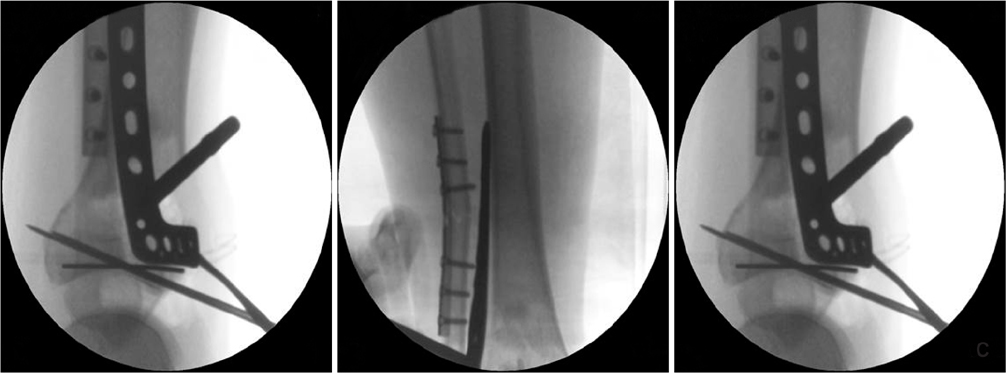
The Result of Using an Additional Mini-Locking Plate for Tibial Pilon Fractures
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chosun University Hospital, Chosun University School of Medicine, Gwangju, Korea. leejy88@chosun.ac.kr
- KMID: 2376613
- DOI: http://doi.org/10.12671/jkfs.2017.30.2.75
Abstract
- PURPOSE
We evaluated the usefulness of an additional, 2.7 mm mini-locking plate for tibial pilon fractures.
MATERIALS AND METHODS
We studied 21 patients (14 males and 7 females), who were treated with a 2.7 mm mini-locking plate via the anterolateral approach for tibial pilon fractures between September 2012 and April 2014. The mean age was 43.85 years, and the mean follow-up period was 16.6 months. The radiologic outcomes were graded by the Burwell and Charnley modified system and clinical outcomes were evaluated by the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hind foot score and visual analogue scale (VAS) score.
RESULTS
The mean union period was 14.3 weeks. At the final follow-up, radiologic results showed 16 excellent results, 4 fair results, and 1 poor result. The average VAS was 3.4 points; the average AOFAS score was 81.8 points. During the follow-up period, there were three cases of posttraumatic osteoarthritis and one case of superficial skin infection.
CONCLUSION
Additional anterolateral, 2.7 mm mini-locking plate may be a good treatment method to manage tibial pilon fractures.
Figure
Reference
-
1. Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 2001; 15:153–160.
Article2. Bone L, Stegemann P, McNamara K, Seibel R. External fixation of severely comminuted and open tibial pilon fractures. Clin Orthop Relat Res. 1993; (292):101–107.
Article3. Leung F, Kwok HY, Pun TS, Chow SP. Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury. 2004; 35:278–283.
Article4. Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma. 1999; 13:85–91.
Article5. Baumgaertel F, Buhl M, Rahn BA. Fracture healing in biological plate osteosynthesis. Injury. 1998; 29:Suppl 3. C3–C6.
Article6. Claes L, Heitemeyer U, Krischak G, Braun H, Hierholzer G. Fixation technique influences osteogenesis of comminuted fractures. Clin Orthop Relat Res. 1999; (365):221–229.
Article7. Gerber M, Richardson S, Cavallo F, et al. The role of diet history and biologic assays in the study of “diet and breast cancer”. Tumori. 1990; 76:321–330.
Article8. Jastifer JR. Topical review: locking plate technology in foot and ankle surgery. Foot Ankle Int. 2014; 35:512–518.9. Dujardin F, Abdulmutalib H, Tobenas AC. Total fractures of the tibial pilon. Orthop Traumatol Surg Res. 2014; 100:S65–S74.
Article10. Barei DP, Nork SE. Fractures of the tibial plafond. Foot Ankle Clin. 2008; 13:571–591.
Article11. Chen L, O'Shea K, Early JS. The use of medial and lateral surgical approaches for the treatment of tibial plafond fractures. J Orthop Trauma. 2007; 21:207–211.
Article12. Khazzam M, Della Rocca GJ, Wade AM, Murtha YM, Crist BD. Anterolateral approach to the distal tibia for fixation of pilon fractures: rate of wound complications in the early postoperative period. Curr Orthop Pract. 2012; 23:111–115.
Article13. Howard JL, Agel J, Barei DP, Benirschke SK, Nork SE. A prospective study evaluating incision placement and wound healing for tibial plafond fractures. J Orthop Trauma. 2008; 22:299–305. discussion 305-306.
Article14. Deivaraju C, Vlasak R, Sadasivan K. Staged treatment of pilon fractures. J Orthop. 2015; 12:S1–S6.
Article15. Lee KB. Distal tibia fracture: plate osteosynthesis. J Korean Fract Soc. 2009; 22:306–313.
Article16. Maffulli N, Toms AD, McMurtie A, Oliva F. Percutaneous plating of distal tibial fractures. Int Orthop. 2004; 28:159–162.
Article17. Ghera S, Santori FS, Calderaro M, Giorgini TL. Minimally invasive plate osteosynthesis in distal tibial fractures: pitfalls and surgical guidelines. Orthopedics. 2004; 27:903–905.
Article18. Lee HS, Kim JJ, Oh SK, Ahn HS. Treatment of distal tibial metaphyseal fracture using MIPPO technique. J Korean Foot Ankle Soc. 2004; 8:166–170.19. Vidyadhara S, Rao SK. Ilizarov treatment of complex tibial pilon fractures. Int Orthop. 2006; 30:113–117.
Article20. Bozkurt M, Ocguder DA, Ugurlu M, Kalkan T. Tibial pilon fracture repair using Ilizarov external fixation, capsuloligamentotaxis, and early rehabilitation of the ankle. J Foot Ankle Surg. 2008; 47:302–306.
Article21. Kim YJ, Jung HG, Lee JH, Byun WS, Lee ST. Comminuted pilon fractures: comparative outcome analysis according to surgical techniques. J Korean Fract Soc. 2007; 20:6–12.
Article22. Lomax A, Singh A, N Jane M, C Senthil K. Complications and early results after operative fixation of 68 pilon fractures of the distal tibia. Scott Med J. 2015; 60:79–84.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures: Technical Note
- Current Treatment of Tibial Pilon Fractures
- Lateral Locked Plating or Dual Plating: A Comparison of Two Methods in Simple Bicondylar Tibial Plateau Fractures
- A Clinical Study of tibial Pilon Fractures
- Treatment of The Pilon Fracture involving Tibial Shaft using Two Staged MIPO Technique