J Korean Soc Surg Hand.
2017 Mar;22(1):41-48. 10.12790/jkssh.2017.22.1.41.
Neurologic Deficits after Surgical Enucleation of Schwannoma in the Upper Extremity
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. ygchung@catholic.ac.kr
- KMID: 2375466
- DOI: http://doi.org/10.12790/jkssh.2017.22.1.41
Abstract
- PURPOSE
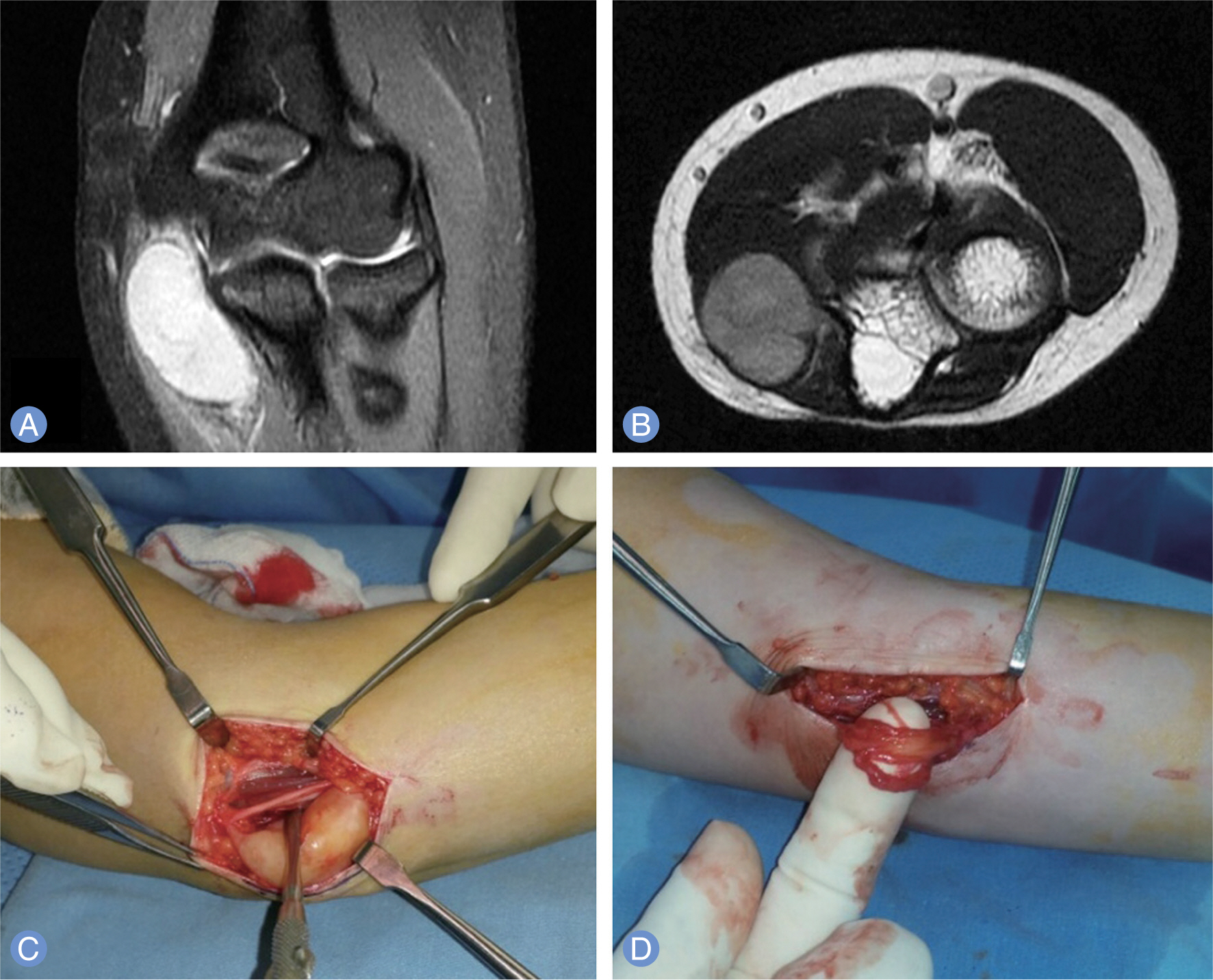
Neurologic deficits after enucleation of schwannoma are not rare. To evaluate the neurologic deficits after surgical enucleation of schwannoma in the upper extremity, we performed a retrospective review of patients with surgically treated schwannoma over a 14-year period at a single institution.
METHODS
Between March 2001 and September 2014, 103 patients underwent surgical enucleation for schwannomas; 36 patients of them had lesions in the upper extremity, and 2 out of 36 patients had multiple schwannomas. Each operation was performed by a single surgeon under loupe magnification. The postoperative neurological deficits were graded as major and minor in both immediate postoperatively and at last follow-up. The major deficit was defined as anesthesia or marked hypoesthesia, motor weakness of grade 3 or less and neuropathic pain. Minor deficit was defined as mild symptoms of mild hypoesthesia, paresthesia and motor weakness of grade 4 or more.
RESULTS
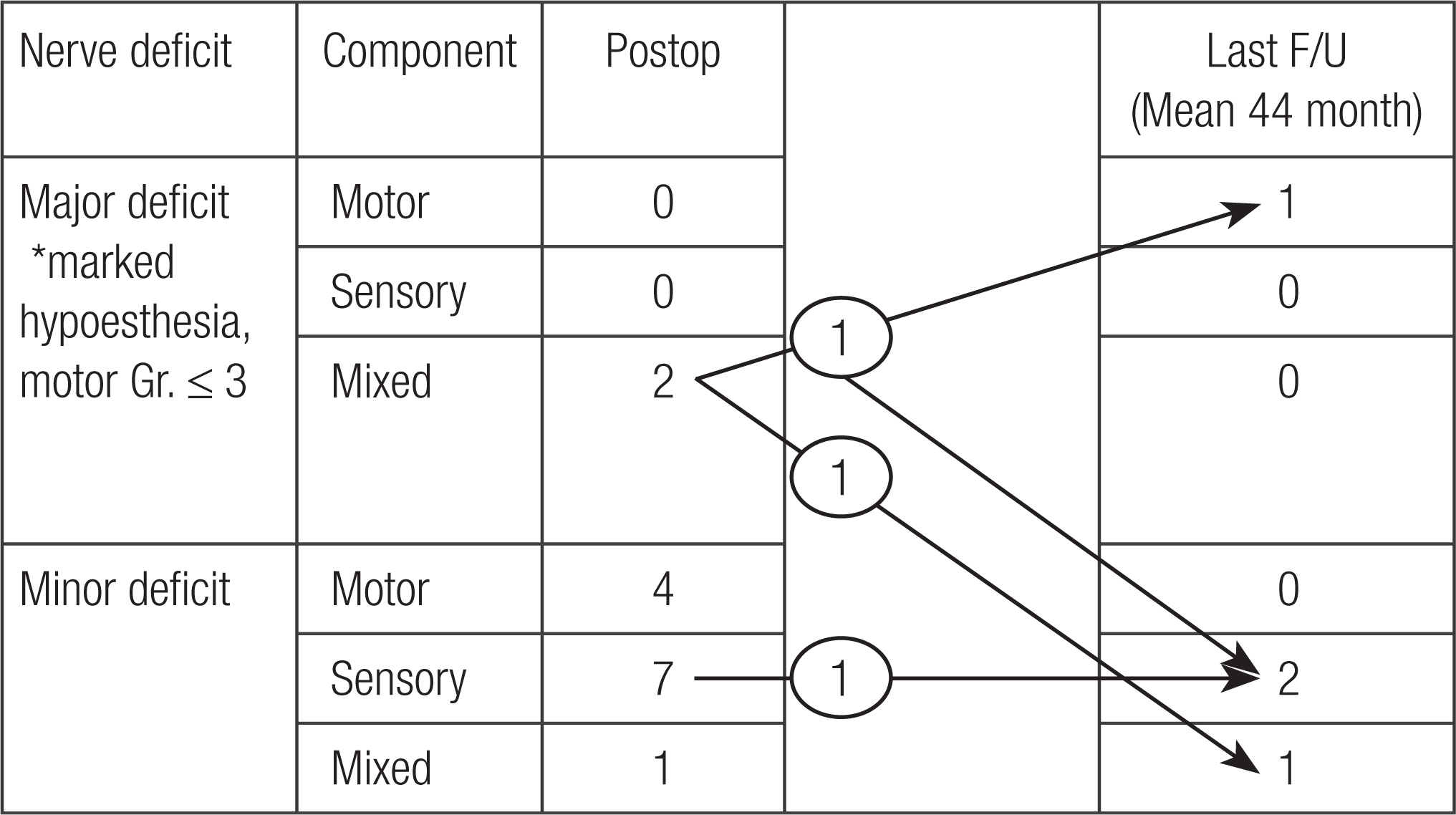
There were 2 major (2 mixed nerve) and 12 minor (4 motor, 7 sensory, 1 mixed nerve) neurologic deficits after surgery. At the last follow-up, one major mixed neurologic deficit remained as major motor and minor sensory, and other major ones changed to mixed minor. And all minor deficits except 1 sensory deficit were recovered spontaneously.
CONCLUSION
Even though high incidence rate of neurologic deficit after enucleation of schwannoma in the upper extremity (38.9%), about three fourths of them were recovered spontaneously. There were 3 permanent neurologic deficits, and one of them was major one. In some cases, surgeon cannot avoid to encounter a neurological deficit. So we recommend more delicate microscopic surgical procedure and preoperative planning and counseling. And surgery is indicated for only symptomatic lesions.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Donner TR, Voorhies RM, Kline DG. Neural sheath tumors of major nerves. J Neurosurg. 1994; 81:362–73.
Article2. Colon F, Upton J. Pediatric hand tumors: a review of 349 cases. Hand Clin. 1995; 11:223–43.3. Strickland JW, Steichen JB. Nerve tumors of the hand and forearm. J Hand Surg Am. 1977; 2:285–91.
Article4. Kehoe NJ, Reid RP, Semple JC. Solitary benign peripheral-nerve tumours: review of 32 years’ experience. J Bone Joint Surg Br. 1995; 77:497–500.
Article5. Holdsworth BJ. Nerve tumours in the upper limb: a clinical review. J Hand Surg Br. 1985; 10:236–8.
Article6. Molina AR, Chatterton BD, Kalson NS, Fallowfield ME, Khandwala AR. Multiple schwannomas of the upper limb related exclusively to the ulnar nerve in a patient with segmental schwannomatosis. J Plast Reconstr Aesthet Surg. 2013; 66:e376–9.
Article7. Hasham S, Matteucci P, Stanley PR. Schwannomatosis: multiple schwannomas of the upper limb. J Hand Surg Br. 2006; 31:182–4.
Article8. Phalen GS. Neurilemmomas of the forearm and hand. Clin Orthop Relat Res. 1976; (114):219–22.
Article9. Park MJ, Seo KN, Kang HJ. Neurological deficit after surgical enucleation of schwannomas of the upper limb. J Bone Joint Surg Br. 2009; 91:1482–6.
Article10. Mizushima H. Neurological deficits before and after surgical resection of schwannomas in the upper extremities. J Reconstr Microsurg. 2016; 32:371–7.
Article11. Adani R, Tarallo L, Mugnai R, Colopi S. Schwannomas of the upper extremity: analysis of 34 cases. Acta Neurochir (Wien). 2014; 156:2325–30.
Article12. Tang CY, Fung B, Fok M, Zhu J. Schwannoma in the upper limbs. Biomed Res Int. 2013; 2013:167196.13. Kim SM, Seo SW, Lee JY, Sung KS. Surgical outcome of schwannomas arising from major peripheral nerves in the lower limb. Int Orthop. 2012; 36:1721–5.
Article14. James MA. Use of the Medical Research Council muscle strength grading system in the upper extremity. J Hand Surg Am. 2007; 32:154–6.
Article15. Kang HJ, Shin SJ, Kang ES. Schwannomas of the upper extremity. J Hand Surg Br. 2000; 25:604–7.
Article16. Ujigo S, Shimose S, Kubo T, Fujimori J, Ochi M. Therapeutic effect and risk factors for complications of excision in 76 patients with schwannoma. J Orthop Sci. 2014; 19:150–5.
Article17. Levi AD, Ross AL, Cuartas E, Qadir R, Temple HT. The surgical management of symptomatic peripheral nerve sheath tumors. Neurosurgery. 2010; 66:833–40.
Article18. Forthman CL, Blazar PE. Nerve tumors of the hand and upper extremity. Hand Clin. 2004; 20:233–42.
Article19. Sawada T, Sano M, Ogihara H, Omura T, Miura K, Nagano A. The relationship between pre-operative symptoms, operative findings and postoperative complications in schwannomas. J Hand Surg Br. 2006; 31:629–34.
Article20. Artico M, Cervoni L, Wierzbicki V, D’Andrea V, Nucci F. Benign neural sheath tumours of major nerves: characteristics in 119 surgical cases. Acta Neurochir (Wien). 1997; 139:1108–16.
Article21. Oberle J, Kahamba J, Richter HP. Peripheral nerve schwannomas: an analysis of 16 patients. Acta Neurochir (Wien). 1997; 139:949–53.22. Knight DM, Birch R, Pringle J. Benign solitary schwannomas: a review of 234 cases. J Bone Joint Surg Br. 2007; 89:382–7.23. Takase K, Yamamoto K, Imakiire A. Clinical pathology and therapeutic results of neurilemmoma in the upper extremity. J Orthop Surg (Hong Kong). 2004; 12:222–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Outcomes of Schwannoma Occurring at Major Peripheral Nerves of Extremity: A Single Institution Analysis
- A Schwannoma Originating from Median Nerve at Proximal Forearm Caused Ulnar Nerve Symptom by Compression
- Outcome of Schwannoma Resection at Upper Extremity with Preservation of Nerve Fascicle
- A Case of Multiple Cutaneous Plexiform Schwannomas Accompanying Neurologic Deficits
- Asymtomatic Giant Benign Schwannoma Involving Cervical Vertebral Body: A Case Report-