Pediatr Gastroenterol Hepatol Nutr.
2017 Mar;20(1):27-33. 10.5223/pghn.2017.20.1.27.
Comparison of Percutaneous Endoscopic Gastrostomy and Surgical Gastrostomy in Severely Handicapped Children
- Affiliations
-
- 1Department of Pediatrics, Chonbuk National University Hospital, Chonbuk National University Medical School, Jeonju, Korea. kimsc@jbnu.ac.kr
- 2Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2375275
- DOI: http://doi.org/10.5223/pghn.2017.20.1.27
Abstract
- PURPOSE
Gastrostomy is commonly used procedures to provide enteral nutrition support for severely handicapped patients. This study aimed to identify and compare outcomes and complications associated with percutaneous endoscopic gastrostomy (PEG) and surgical gastrostomy (SG).
METHODS
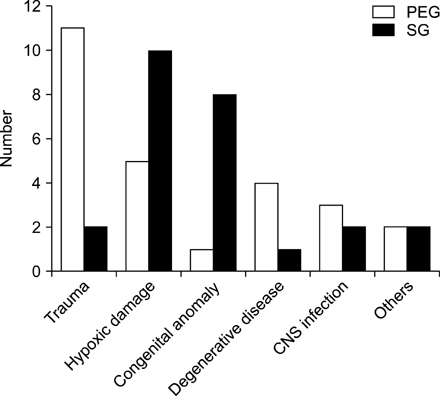
A retrospective chart review of 51 patients who received gastrostomy in a single tertiary hospital from January 2000 to May 2016 was performed. We analyzed the patients and the complications caused by the procedures.
RESULTS
Among the 51 patients, 26 had PEG and 25 had SG. Four cases in the SG group had fundoplication for gastroesophageal reflux disease. PEG and SG groups were followed up for an average of 29 months and 44 months. Major complications occurred in 19.2% of patients in the PEG group and 20.0% in the SG group, but significant differences between the groups were not observed. Minor complications occurred in 15.4% of patients in the PEG group and 52.0% in the SG group. Minor complications were significantly lower in the PEG group than in the SG group (p=0.006). The average use of antibiotics in the PEG and SG groups was 6.2 days and 15.7 days (p=0.002). Thirteen patients died of underlying disease but not related to gastrostomy, and only one patient died due to complications associated with general anesthesia.
CONCLUSION
The duration of antibiotics use and incidence of minor complications were significantly lower in the PEG group than those in the SG group. Early PEG could be recommended for nutritional supports.
Keyword
MeSH Terms
Figure
Reference
-
1. Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980; 15:872–875.
Article2. Grant JP. Comparison of percutaneous endoscopic gastrostomy with Stamm gastrostomy. Ann Surg. 1988; 207:598–603.
Article3. Stringel G, Geller ER, Lowenheim MS. Laparoscopic-assisted percutaneous endoscopic gastrostomy. J Pediatr Surg. 1995; 30:1209–1210.
Article4. Reiner DS, Leitman IM, Ward RJ. Laparoscopic stamm gastrostomy with gastropexy. Surg Laparosc Endosc. 1991; 1:189–192.5. Cook S, Hooper V, Nasser R, Larsen D. Effect of gastrostomy on growth in children with neurodevelopmental disabilities. Can J Diet Pract Res. 2005; 66:19–24.
Article6. Smith SW, Camfield C, Camfield P. Living with cerebral palsy and tube feeding: a population-based follow-up study. J Pediatr. 1999; 135:307–310.
Article7. Gang MH, Kim JY. Short-term complications of percutaneous endoscopic gastrostomy according to the type of technique. Pediatr Gastroenterol Hepatol Nutr. 2014; 17:214–222.
Article8. McSweeney ME, Smithers CJ. Advances in pediatric gastrostomy placement. Gastrointest Endosc Clin N Am. 2016; 26:169–185.
Article9. Lucendo AJ, Friginal-Ruiz AB. Percutaneous endoscopic gastrostomy: an update on its indications, management, complications, and care. Rev Esp Enferm Dig. 2014; 106:529–539.10. Chang SH, Kim DY, Kim SC, Kim IK, Kim KM. Complications of percutaneous endoscopic gastrostomy (PEG) in children. Korean J Pediatr Gastroenterol Nutr. 2004; 7:8–15.
Article11. Liu R, Jiwane A, Varjavandi A, Kennedy A, Henry G, Dilley A, et al. Comparison of percutaneous endoscopic, laparoscopic and open gastrostomy insertion in children. Pediatr Surg Int. 2013; 29:613–621.
Article12. Fox VL, Abel SD, Malas S, Duggan C, Leichtner AM. Complications following percutaneous endoscopic gastrostomy and subsequent catheter replacement in children and young adults. Gastrointest Endosc. 1997; 45:64–71.
Article13. ASGE Standards of Practice Committee. Lightdale JR, Acosta R, Shergill AK, Chandrasekhara V, Chathadi K, et al. Modifications in endoscopic practice for pediatric patients. Gastrointest Endosc. 2014; 79:699–710.
Article14. Fredette ME, Lightdale JR. Endoscopic sedation in pediatric practice. Gastrointest Endosc Clin N Am. 2008; 18:739–751,ix.
Article15. van Beek EJ, Leroy PL. Safe and effective procedural sedation for gastrointestinal endoscopy in children. J Pediatr Gastroenterol Nutr. 2012; 54:171–185.
Article16. Miller RE, Kummer BA, Tiszenkel HI, Kotler DP. Percutaneous endoscopic gastrostomy: procedure of choice. Ann Surg. 1986; 204:543–545.17. Wasiljew BK, Ujiki GT, Beal JM. Feeding gastrostomy: complications and mortality. Am J Surg. 1982; 143:194–195.
Article18. El-Matary W. Percutaneous endoscopic gastrostomy in children. Can J Gastroenterol. 2008; 22:993–998.
Article19. McSweeney ME, Jiang H, Deutsch AJ, Atmadja M, Lightdale JR. Long-term outcomes of infants and children undergoing percutaneous endoscopy gastrostomy tube placement. J Pediatr Gastroenterol Nutr. 2013; 57:663–667.
Article20. Rudra A, Chatterjee S, Sengupta S, Iqbal A, Pal S, Wankhede R. The child with cerebral palsy and anaesthesia. Indian J Anaesth. 2008; 52:397–403.21. Maranhão MV. Anesthesia and cerebral palsy. Rev Bras Anestesiol. 2005; 55:680–702.22. Wass CT, Warner ME, Worrell GA, Castagno JA, Howe M, Kerber KA, et al. Effect of general anesthesia in patients with cerebral palsy at the turn of the new millennium: a population-based study evaluating perioperative outcome and brief overview of anesthetic implications of this coexisting disease. J Child Neurol. 2012; 27:859–866.
Article23. Tucker AT, Gourin CG, Ghegan MD, Porubsky ES, Martindale RG, Terris DJ. ‘Push’ versus ‘pull’ percutaneous endoscopic gastrostomy tube placement in patients with advanced head and neck cancer. Laryngoscope. 2003; 113:1898–1902.
Article24. Gauderer MW. Percutaneous endoscopic gastrostomy: a 10-year experience with 220 children. J Pediatr Surg. 1991; 26:288–292.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Endoscopic Gastrostomy Through the Sinus Tract of a Surgical Gastrostomy
- Long Term Efficacy of Percutaneous Endoscopic Gastrostomy
- Updates on Percutaneous Radiologic Gastrostomy/Gastrojejunostomy and Jejunostomy
- A Case of Buried Bumper Syndrome; A case report
- A Case of Percutaneous Endoscopic Gastrostomy in a Patient with Liver Cirrhosis Accompanied by Both Esophageal and Gastric Varices