Korean J Phys Anthropol.
2017 Mar;30(1):21-27. 10.11637/kjpa.2017.30.1.21.
The Application and Effectiveness for Medical Procedural Skills through the Use of the Cadaver Model
- Affiliations
-
- 1Department of Anatomy, Keimyung University School of Medicine, Korea. neuroana@dsmc.or.kr
- 2Department of Preventive Medicine, Keimyung University School of Medicine, Korea.
- KMID: 2374773
- DOI: http://doi.org/10.11637/kjpa.2017.30.1.21
Abstract
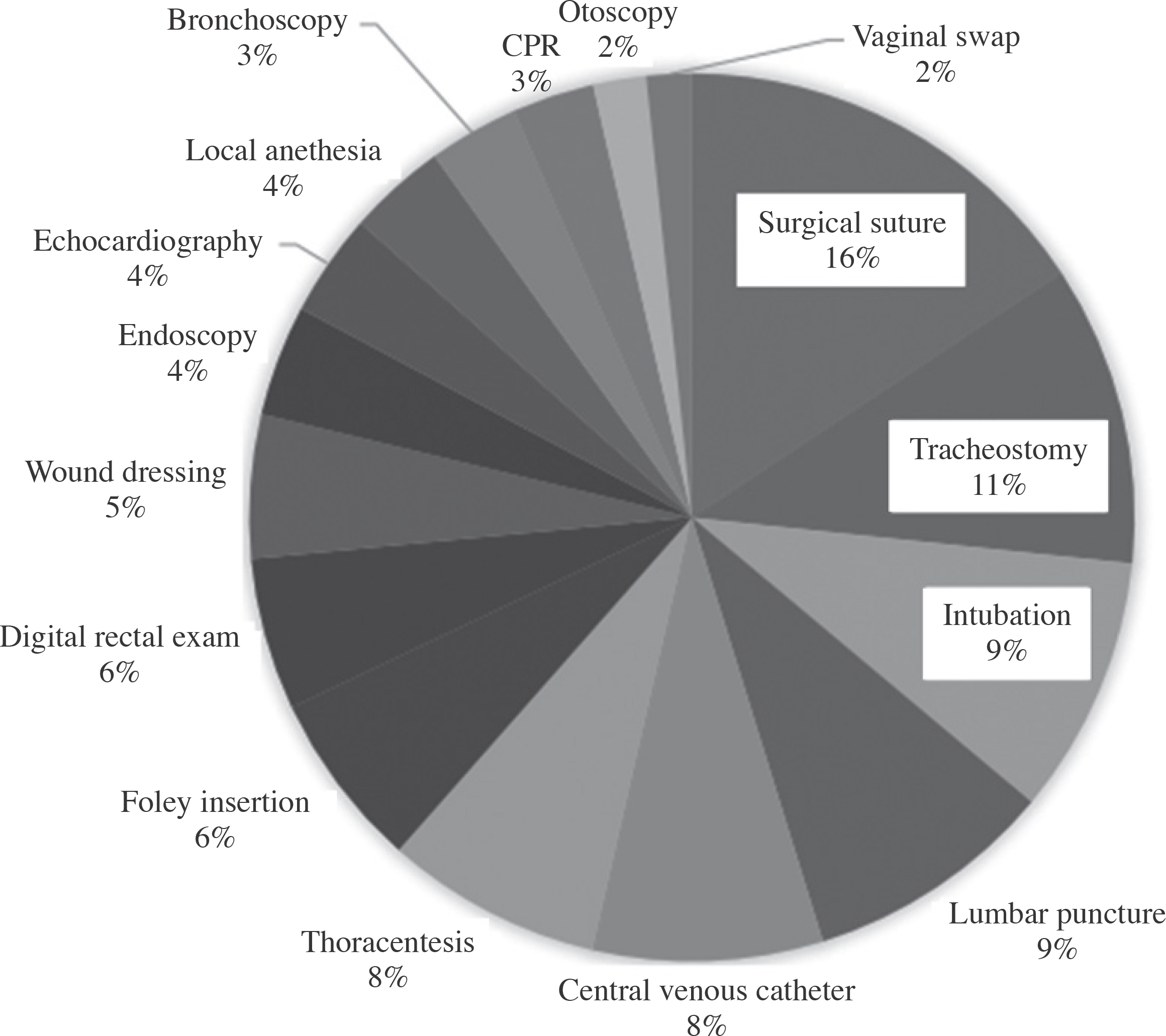
- For this study, medical students, intern physicians, and resident physicians, were surveyed about the application and effectiveness for medical procedure training using cadaver. In this survey, with a target population of 170 individuals, 105 individuals (61.7%) showed positive responses to learning medical procedural using cadaver. Resident physicians group (80.8%) showed relatively positive responses compared to 4(th) year medical students (58.1%) and intern physicians (47.6%); however, this did not account for any significant statistical difference. Regarding the application of cadaver to medical procedural practices, 95 individuals (62.1%) showed positive responses. Resident physicians (74.5%) had the highest percentage of positive responses compared to intern physicians (56.7%) and 4(th) year medical students (56.6%), and there was a significant statistical difference. Suture (15.7%) was ranked first as the most suitable medical procedural to be practiced on cadaver; tracheotomy and intubation came second and third respectively. This research confirmed the application and the effectiveness of cadaver for medical procedural training and the improvement of general medical procedural ability are expected if the cadaver is applied not only to medical schools but also to intern and resident physician training.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Coulehan JL, Williams PC, Landis D, Naser C. The first patient: reflections and stories about the anatomy cadaver. Teach Learn Med. 1995; 7:61–6.
Article2. Dinsmore CE, Daugherty S, Zeitz HJ. Student responses to the gross anatomy laboratory in a medical curriculum. Clin Anat. 2001; 14:231–6.
Article3. Park H. Clinical application of objective structured clinical examination (OSCE). Korean J Med Educ. 2004; 16:13–23.
Article4. Lee YM, Hwang K, Baik SH, Hong MH, Choi YS, Kim SH. An experience of OSCE for introducing clinical performance assessment to Korean medical licensure examination. Korean J Med Educ. 2001; 13:47–57.
Article5. Choi SH, Koh SB. Introduction of Objective Structured Clinical Examination (OSCE) to Residency Examination. Korean J Med Educ. 2008; 20:343–9.
Article6. Kim SW, Lim SY, Mun GH, Shin JS. Introduction of OSCE (objective structured clinical examination) to board licensure examination of plastic surgeons. Korean J Med Educ. 2006; 18:153–60.
Article7. Sternbach GL, Rosen P. Use of laboratory animals in the teaching of emergency procedures. J Am Coll Emerg Phys. 1977; 6:543–5.
Article8. Lenhard A, Moallem M, Marrie RA, Becker J, Garland A. An intervention to improve procedure education for internal medicine residents. J Gen Intern Med. 2008; 23:288–93.
Article9. Olshaker JS, Brown CK, Arthur DC, Tek D. Animal procedure laboratory surveys: use of the animal laboratory to improve physician confidence and ability. J Emerg Med. 1989; 7:593–7.
Article10. Do HS, Min JH, Hong SW, Han SK, Kim IS, Ryu S, et al. Evaluation of the educational efficacy of a cadaver-based model for teaching a simple suture technique to medical students. J Korean Soc Traumatol. 2006; 19:121–5.11. Gilbody J, Prasthofer A, Ho K, Costa ML. The use and effectiveness of cadaveric workshops in higher surgical training: a systematic review. Ann R Coll Surg Engl. 2011; 93:347–52.
Article12. Weaver M, Kyrouac J, Frank S, Rabinovich S. A cadaver workshop to teach medical procedures. Med Educ. 1986; 20:407–9.
Article13. Lewis CE, Peacock WJ, Tillou A, Hines OJ, Hiatt JR. A novel cadaver-based educational program in general sur-gery training. J Surg Educ. 2012; 69:693–8.
Article14. Oxentenko AS, Ebbert JO, Ward LE, Pankratz VS, Wood KE. A multidimensional workshop using human cadavers to teach bedside procedures. Teach Learn Med. 2003; 15:127–30.
Article15. Varga S, Smith J, Minneti M, Carey J, Zakaluzny S, Noguchi T, et al. Central venous catheterization using a perfused human cadaveric model: application to surgical education. J Surg Educ. 2015; 72:28–32.
Article16. Park H. Clinical skills assessment in Korean medical licensing examination. Korean J Med Educ. 2008; 20:309–12.
Article17. English DC. Using animals for the training of physicians and surgeons. Theor Med. 1989; 10:43–52.
Article18. Cheong J. The use of animals in medical education: a question of necessity vs. desirability. Theor Med. 1989; 10:53–7.
Article19. Scott WC, Coble YD, Eisenbrey AB, Estes EH, Karlan MS, Kennedy WR, et al. Use of animals in medical education. JAMA. 1991; 266:836–7.
Article20. van der Vlugt TM, Harter PM. Teaching procedural skills to medical students: one institution's experience with an emergency procedures course. Ann Emerg Med. 2002; 40:41–9.
Article21. Swindle M. Swine as replacements for dogs in the surgical teaching and research laboratory. Lab Anim Sci. 1984; 34:383.22. Proano L, Jagminas L, Homan CS, Reinert S. Evaluation of a teaching laboratory using a cadaver model for tube tho-racostomy. J Emerg Med. 2002; 23:89–95.
Article23. Tabas JA, Rosenson J, Price DD, Rohde D, Baird CH, Dhillon N. A comprehensive, unembalmed cadaver-based course in advanced emergency procedures for medical students. Acad Emerg Med. 2005; 12:782–5.
Article24. Watson RA, Deshon GE, Agee RE. Surgical experience with large animals: important adjunct to residency training in urology. Urology. 1982; 20:154–6.25. Woods Jr JR, Ansbacher R, Castro RJ, Marshall W, Trabal JF. Animal surgery: an adjunct to training in obstetrics and gynecology. Obstet Gynecol. 1980; 56:373–4.26. Berkenstadt H, Ziv A, Gafni N, Sidi A. Incorporating sim-ulation-based objective structured clinical examination into the Israeli National Board Examination in Anesthesiology. Anesth Analg. 2006; 102:853–8.
Article27. Gerrow JD, Murphy HJ, Boyd MA, Scott DA. Concurrent validity of written and OSCE components of the Canadian dental certification examinations. J Dent Educ. 2003; 67:896–901.
Article28. Sloan DA, Donnelly MB, Schwartz RW, Strodel WE. The Objective Structured Clinical Examination. The new gold standard for evaluating postgraduate clinical performance. Ann Surg. 1995; 222:735.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the Educational Efficacy of a Cadaver-based Model for Teaching a Simple Suture Technique to Medical Students
- Effect of Practice based Program for Procedural Skills
- Teaching and Learning Communication Skills in Medical Education
- Implications of Changes in Legal Standards Related to Cadaver Research and Future Tasks
- The Effectiveness of Standardized Patient Managed Instruction in Teaching Foley Catheterization Skills, Communication Skills and Learning Motivation