Ann Surg Treat Res.
2017 Apr;92(4):221-224. 10.4174/astr.2017.92.4.221.
Acetic acid sclerotherapy for treatment of biliary leak from an isolated right posterior sectoral duct after cholecystectomy
- Affiliations
-
- 1Department of Surgery, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. jipark@paik.ac.kr
- 2Department of Surgery, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2374688
- DOI: http://doi.org/10.4174/astr.2017.92.4.221
Abstract
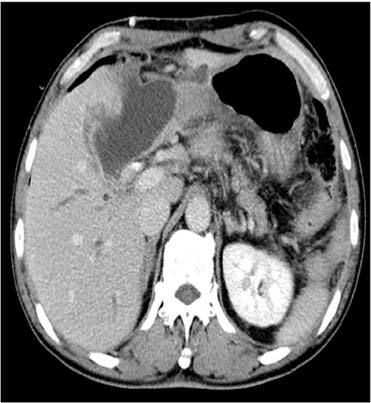
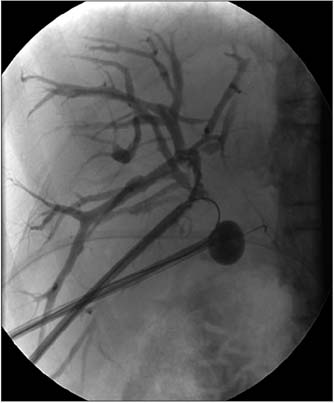
- Bile duct injury is one of the most serious complications of both laparoscopic and open cholecystectomy. Isolated bile duct injury can occur from the misidentification of aberrant right hepatic ducts, and it is troublesome because the early diagnosis is easy to miss and the definite treatment is controversial. We report a case of an isolated right posterior sectoral duct injury following cholecystectomy managed successfully with acetic acid sclerotherapy combined with coil embolization for a fistula tract.
Keyword
MeSH Terms
Figure
Reference
-
1. Perini RF, Uflacker R, Cunningham JT, Selby JB, Adams D. Isolated right segmental hepatic duct injury following laparoscopic cholecystectomy. Cardiovasc Intervent Radiol. 2005; 28:185–195.2. Hwang S, Lee SG, Lee YJ, Ha TY, Ko GY, Song GW. Delayed-onset isolated injury of the right posterior segment duct after laparoscopic cholecystectomy: a report of hepatic segmental atrophy induction. Surg Laparosc Endosc Percutan Tech. 2007; 17:203–205.3. Colovic RB. Isolated segmental, sectoral and right hepatic bile duct injuries. World J Gastroenterol. 2009; 15:1415–1419.4. Mazer LM, Tapper EB, Sarmiento JM. Nonoperative management of right posterior sectoral duct injury following laparoscopic cholecystectomy. J Gastrointest Surg. 2011; 15:1237–1242.5. Wojcicki M, Patkowski W, Chmurowicz T, Bialek A, Wiechowska-Kozlowska A, Stankiewicz R, et al. Isolated right posterior bile duct injury following cholecystectomy: report of two cases. World J Gastroenterol. 2013; 19:6118–6121.6. Choi G, Eun CK, Choi H. Acetic acid sclerotherapy for treatment of a bile leak from an isolated bile duct after laparoscopic cholecystectomy. Cardiovasc Intervent Radiol. 2011; 34:Suppl 2. S303–S306.7. Park JH, Oh JH, Yoon Y, Hong SH, Park SJ. Acetic acid sclerotherapy for treatment of a biliary leak from an isolated bile duct after hepatic surgery. J Vasc Interv Radiol. 2005; 16:885–888.8. Matsumoto T, Iwaki K, Hagino Y, Kawano K, Kitano S, Tomonari K, et al. Ethanol injection therapy of an isolated bile duct associated with a biliary-cutaneous fistula. J Gastroenterol Hepatol. 2002; 17:807–810.9. Kyokane T, Nagino M, Sano T, Nimura Y. Ethanol ablation for segmental bile duct leakage after hepatobiliary resection. Surgery. 2002; 131:111–113.10. Ohnishi K, Ohyama N, Ito S, Fujiwara K. Small hepatocellular carcinoma: treatment with US-guided intratumoral injection of acetic acid. Radiology. 1994; 193:747–752.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful non-surgical treatment for isolated right anterior section bile duct injury following laparoscopic cholecystectomy: Report of a case
- Therapeutic induction of hepatic atrophy for isolated injury of the right posterior sectoral duct following laparoscopic cholecystectomy
- Isolated aberrant right cysticohepatic duct injury during laparoscopic cholecystectomy: Evaluation and treatment challenges of a severe postoperative complication associated with an extremely rare anatomical variant
- Minimal invasive treatment of biliary leak after laparoscopic cholecystectomy
- A Case of Bile Leak from the Accessory Bile Duct after Laparoscopic Cholecystectomy