Clin Orthop Surg.
2016 Sep;8(3):243-248. 10.4055/cios.2016.8.3.243.
Stoppa Approach for Anterior Plate Fixation in Unstable Pelvic Ring Injury
- Affiliations
-
- 1Department of Orthopedic Surgery, Inje University Ilsan Paik Hospital, Goyang, Korea. osd11@paik.ac.kr
- 2Department of Orthopedic Surgery, Asan Medical Center, Seoul, Korea.
- 3Department of Orthopedic Surgery, UC Davis Medical Center, Sacramento, CA, USA.
- KMID: 2374268
- DOI: http://doi.org/10.4055/cios.2016.8.3.243
Abstract
- BACKGROUND
The Stoppa (intrapelvic) approach has been introduced for the treatment of pelvic-acetabular fractures; it allows easy exposure of the pelvic brim, where the bone quality is optimal for screw fixation. The purpose of our study was to investigate the surgical outcomes of unstable pelvic ring injuries treated using the Stoppa approach for stable anterior ring fixation.
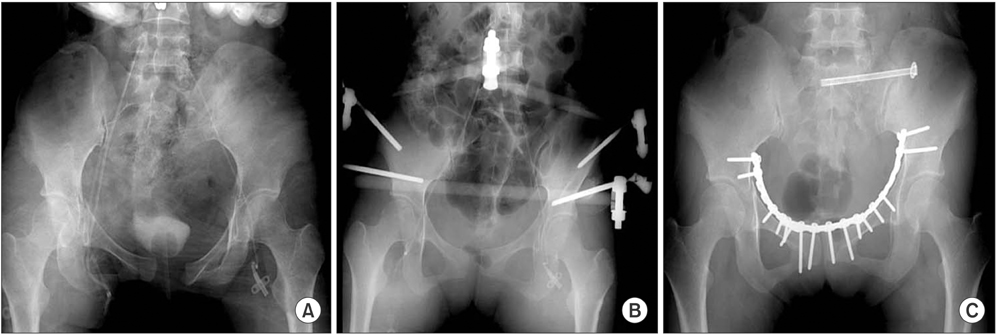
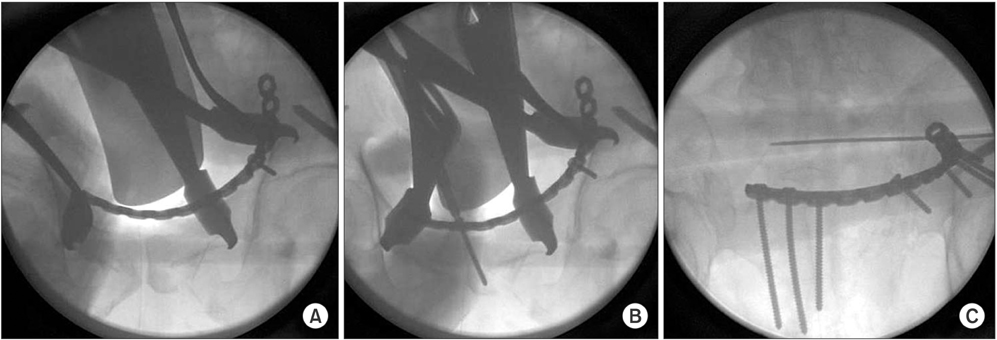
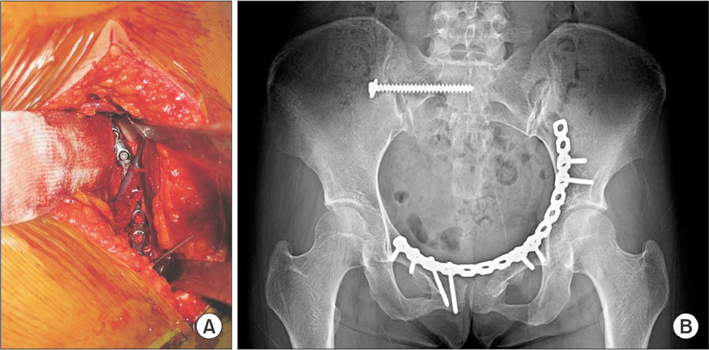
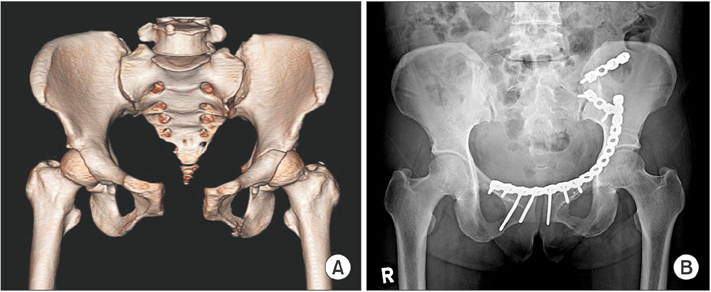
METHODS
We analyzed 22 cases of unstable pelvic ring injury treated with plate fixation of the anterior ring with the Stoppa approach. We excluded cases of nondisplaced rami fracture, simple symphyseal diastasis, and parasymphyseal fractures, which can be easily treated with other techniques. The average age of the study patients was 41 years (range, 23 to 61 years). There were 10 males and 12 females. According to the Young and Burgess classification, there were 12 lateral compression, 4 anteroposterior compression, and 6 vertical shear fracture patterns. The fracture location on the anterior ring was near the iliopectineal eminence in all cases and exposure of the pelvic brim was required for plate fixation. All patients were placed in the supine position. For anterior plate fixation, all screws were applied to the anterior ramus distally and directed above the hip joint proximally. Radiologic outcomes were assessed by union time and quality of reduction by Matta method. The Merle d'Aubigne-Postel score was used to evaluate the functional results.
RESULTS
The average radiologic follow-up period was 16 months (range, 10 to 51 months). All fractures united at an average of 3.5 months (range, 3 to 5 months). According to the Matta method, the quality of reduction was classified as follows: 16 anatomical (73%) and 6 nearly anatomical (27%) reductions. There were no cases of screw or implant loosening before bone healing. The functional results were classified as 7 excellent (32%), 12 good (55%), and 3 fair (13%) by the Merle d'Aubigne-Postel score. There were no wound complications, neurovascular injuries, or other complications related to the surgical approach.
CONCLUSIONS
Stable anterior ring fixation placed via the Stoppa approach can result in excellent reduction and stable screw fixation with a low complication rate.
Keyword
MeSH Terms
Figure
Reference
-
1. Matta JM, Tornetta P 3rd. Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res. 1996; (329):129–140.
Article2. Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993; (292):62–76.
Article3. Bible JE, Choxi AA, Kadakia RJ, Evans JM, Mir HR. Quantification of bony pelvic exposure through the modified Stoppa approach. J Orthop Trauma. 2014; 28(6):320–323.
Article4. Isaacson MJ, Taylor BC, French BG, Poka A. Treatment of acetabulum fractures through the modified Stoppa approach: strategies and outcomes. Clin Orthop Relat Res. 2014; 472(11):3345–3352.
Article5. Hirvensalo E, Lindahl J, Bostman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993; (297):28–32.
Article6. Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach: description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994; (305):112–123.7. D'Aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954; 36(3):451–475.8. Stoppa RE, Rives JL, Warlaumont CR, Palot JP, Verhaeghe PJ, Delattre JF. The use of Dacron in the repair of hernias of the groin. Surg Clin North Am. 1984; 64(2):269–285.9. Ponsen KJ, Joosse P, Schigt A, Goslings JC, Luitse JS. Internal fracture fixation using the Stoppa approach in pelvic ring and acetabular fractures: technical aspects and operative results. J Trauma. 2006; 61(3):662–667.10. Tile M. Acute pelvic fractures: I. Causation and classification. J Am Acad Orthop Surg. 1996; 4(3):143–151.11. Mears DC, Capito CP, Deleeuw H. Posterior pelvic disruptions managed by the use of the Double Cobra Plate. Instr Course Lect. 1988; 37:143–150.12. Routt ML Jr, Meier MC, Kregor PJ, Mayo KA. Percutaneous iliosacral screws with the patient supine technique. Oper Tech Orthop. 1993; 3(1):35–45.
Article13. Routt ML Jr, Kregor PJ, Simonian PT, Mayo KA. Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma. 1995; 9(3):207–214.
Article14. Ragnarsson B, Olerud C, Olerud S. Anterior square-plate fixation of sacroiliac disruption: 2-8 years follow-up of 23 consecutive cases. Acta Orthop Scand. 1993; 64(2):138–142.
Article15. Simonian PT, Routt ML Jr, Harrington RM, Tencer AF. Internal fixation of the unstable anterior pelvic ring: a biomechanical comparison of standard plating techniques and the retrograde medullary superior pubic ramus screw. J Orthop Trauma. 1994; 8(6):476–482.
Article16. Vikmanis A, Jumtins A. Internal fracture fixation using the anterior retroperitoneal lower laparotomy approach in pelvic ring and acetabular fractures: the first experience and outcomes. Acta Chir Latv. 2011; 10(2):48–52.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Operative Treatment of Unstable Pelvic Ring Injury
- Surgical Fixation of Sacroiliac Joint Complex in Unstable Pelvic Ring Injuries
- Percutaneous Iliosacral Screw Fixation for Pelvic Ring Injury
- Fixation Options of Unstable Posterior Pelvic Ring Disruption: Ilio-Sacral Screw Fixation, S2AI Fixation, Posterior Tension Band Plate Fixation, and Spino-Pelvic Fixation
- Percutaneous screw fixation and external stabilization as definitive surgical intervention for a pelvic ring injury combined with an acetabular fracture in the acute phase of polytrauma in Korea: a case report