Korean J Ophthalmol.
2016 Dec;30(6):443-450. 10.3341/kjo.2016.30.6.443.
Comparison of Long-term Clinical Outcomes between Descemet's Stripping Automated Endothelial Keratoplasty and Penetrating Keratoplasty in Patients with Bullous Keratopathy
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. ckjoo@catholic.ac.kr
- 2Catholic Institute for Visual Science, The Catholic University of Korea College of Medicine, Seoul, Korea.
- KMID: 2374002
- DOI: http://doi.org/10.3341/kjo.2016.30.6.443
Abstract
- PURPOSE
To compare 2-year clinical outcomes of Descemet's stripping automated endothelial keratoplasty (DSAEK) and penetrating keratoplasty (PK) in patients with bullous keratopathy.
METHODS
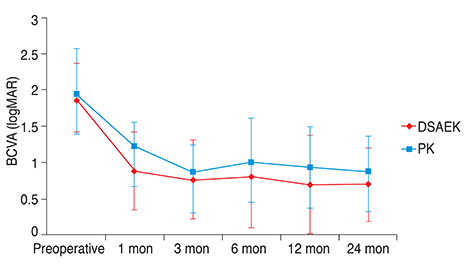
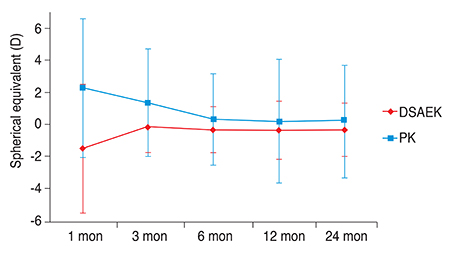
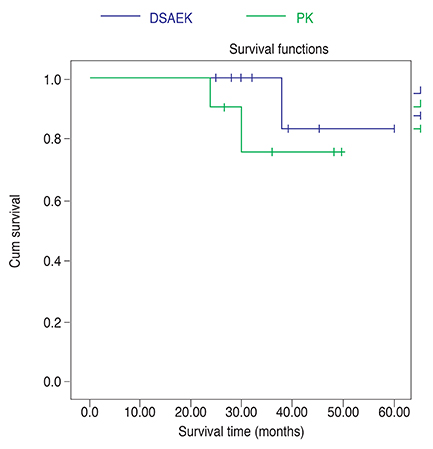
A retrospective chart review was performed to obtain 2 years of follow-up data of DSAEK or PK at a single center from March 2009 to September 2012. The study comprised 15 eyes of DSAEK and 11 eyes of PK. Outcome measures included best-corrected visual acuity (BCVA), spherical and keratometric changes, central corneal thickness, endothelial cell density, intraocular pressure, and postoperative complications. Graft survival rate was assessed by Kaplan-Meier survival analysis.
RESULTS
There were no differences in patient baseline characteristics between the two groups. At postoperative 2 years, better BCVA of 0.69 ± 0.51 logarithm of the minimum angle of resolution (logMAR) was found after DSAEK compared to 0.88 ± 0.48 logMAR after PK. Refractive cylinder in DSAEK and PK was −2.60 ± 1.53 and −6.00 ± 1.05 diopters (D), respectively, and keratometric cylinder was 3.27 ± 3.70 and 6.34 ± 3.51 D, respectively, at postoperative 2 years. The difference of mean spherical equivalents between postoperative 1 month and 2 years was 0.84 D after DSAEK and 2.05 D after PK. A hyperopic shift of 1.17 D was present after 2 years of DSAEK. The mean endothelial cell density at postoperative 2 years was 1,548 ± 456 cells/mm² for DSAEK and 1,052 ± 567 cells/mm² for PK, with a cell loss of 19.96% vs. 52.38%, respectively when compared to postoperative 1 month. No significant difference in central corneal thickness was found between DSAEK and PK (592 ± 75 vs. 563 ± 90 µm, respectively). Finally, the 2-year survival rate did not differ significantly between DSAEK and PK (93.3% vs. 81.8%, respectively, p = 0.344).
CONCLUSIONS
Compared to PK, DSAEK provided more stable refractive errors with better visual outcome, lower endothelial cell loss, and a lower rate of graft rejection at postoperative 2 years in patients with bullous keratopathy.
Keyword
MeSH Terms
Figure
Reference
-
1. Koenig SB, Covert DJ, Dupps WJ Jr, Meisler DM. Visual acuity, refractive error, and endothelial cell density six months after Descemet stripping and automated endothelial keratoplasty (DSAEK). Cornea. 2007; 26:670–674.2. Ratanasit A, Gorovoy MS. Long-term results of Descemet stripping automated endothelial keratoplasty. Cornea. 2011; 30:1414–1418.3. Chen ES, Terry MA, Shamie N, et al. Descemet-stripping automated endothelial keratoplasty: six-month results in a prospective study of 100 eyes. Cornea. 2008; 27:514–520.4. Terry MA, Shamie N, Chen ES, et al. Precut tissue for Descemet's stripping automated endothelial keratoplasty: vision, astigmatism, and endothelial survival. Ophthalmology. 2009; 116:248–256.5. Anshu A, Price MO, Tan DT, Price FW Jr. Endothelial keratoplasty: a revolution in evolution. Surv Ophthalmol. 2012; 57:236–252.6. Nanavaty MA, Wang X, Shortt AJ. Endothelial keratoplasty versus penetrating keratoplasty for Fuchs endothelial dystrophy. Cochrane Database Syst Rev. 2014; (2):CD008420.7. Jun B, Kuo AN, Afshari NA, et al. Refractive change after Descemet stripping automated endothelial keratoplasty surgery and its correlation with graft thickness and diameter. Cornea. 2009; 28:19–23.8. Wacker K, Baratz KH, Maguire LJ, et al. Descemet stripping endothelial keratoplasty for Fuchs' endothelial corneal dystrophy: five-year results of a prospective study. Ophthalmology. 2016; 123:154–160.9. Price MO, Gorovoy M, Price FW Jr, et al. Descemet's stripping automated endothelial keratoplasty: three-year graft and endothelial cell survival compared with penetrating keratoplasty. Ophthalmology. 2013; 120:246–251.10. Ang M, Mehta JS, Lim F, et al. Endothelial cell loss and graft survival after Descemet's stripping automated endothelial keratoplasty and penetrating keratoplasty. Ophthalmology. 2012; 119:2239–2244.11. Terry MA, Chen ES, Shamie N, et al. Endothelial cell loss after Descemet's stripping endothelial keratoplasty in a large prospective series. Ophthalmology. 2008; 115:488–496.e3.12. Price MO, Price FW Jr. Endothelial cell loss after Descemet stripping with endothelial keratoplasty influencing factors and 2-year trend. Ophthalmology. 2008; 115:857–865.13. Busin M, Bhatt PR, Scorcia V. A modified technique for Descemet membrane stripping automated endothelial keratoplasty to minimize endothelial cell loss. Arch Ophthalmol. 2008; 126:1133–1137.14. Price MO, Gorovoy M, Benetz BA, et al. Descemet's stripping automated endothelial keratoplasty outcomes compared with penetrating keratoplasty from the Cornea Donor Study. Ophthalmology. 2010; 117:438–444.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Result of Femtosecond Laser Assisted Descemet's Membrane Stripping Endothelial Keratoplasty
- Eight Cases of Descemet's Stripping Automated Endothelial Keratoplasty in Eyes With Bullous Keratopathy
- Descemet Membrane Endothelial Keratoplasty to Treat Graft Failure after Descemet Stripping Endothelial Keratoplasty
- Long-Term Results of Descemet's Stripping Automated Endothelial Keratoplasty in Korea
- Factors Influencing Corneal Endothelial Cell Density after Descemet Stripping Automated Endothelial Keratoplasty