J Korean Med Sci.
2016 Jun;31(6):963-971. 10.3346/jkms.2016.31.6.963.
Cataract and Cataract Surgery: Nationwide Prevalence and Clinical Determinants
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. jiani4@snu.ac.kr
- 2Department of Preventive Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 3Medical Research Collaborating Center, Seoul National University Bundang Hospital, Seongnam, Korea.
- 4Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2373707
- DOI: http://doi.org/10.3346/jkms.2016.31.6.963
Abstract
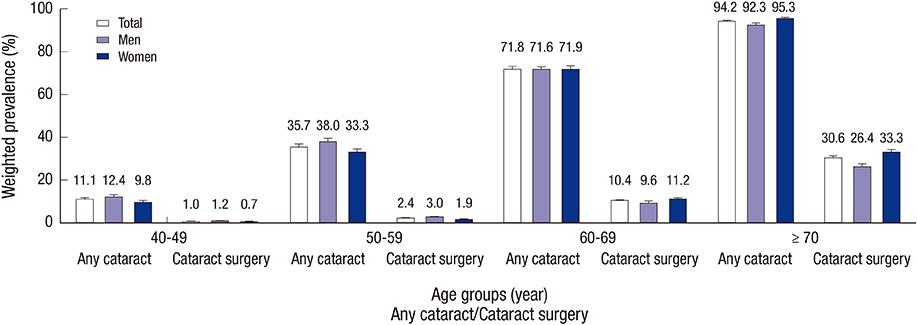
- This study aimed to investigate the prevalence and clinical determinants of cataract and cataract surgery in Korean population. The 2008-2012 Korean National Health and Nutrition Examination Survey was analyzed, which included 20,419 participants aged ≥ 40 years. The survey is a multistage, probability-cluster survey, which can produce nationally representative estimates. Prevalence of cataract and cataract surgery was estimated. Clinical determinants for those were investigated using logistic regression analyses (LRAs). The prevalence of cataract was 42.28% (95% confidence interval [CI], 40.67-43.89); 40.82% (95% CI, 38.97-42.66) for men and 43.62% (95% CI, 41.91-45.33) for women (P = 0.606). The prevalence of cataract surgery was 7.75% (95% CI, 7.30-8.20); 6.38% (95% CI, 5.80-6.96) for men and 9.01% (95% CI, 8.41-9.61) for women (P < 0.001). Cataract was associated with older age (P < 0.001), men (P = 0.032), lower household income (P = 0.031), lower education (P < 0.001), hypertension (P < 0.001), and diabetes mellitus (DM) (P < 0.001). Cataract surgery was consistently associated with older age, occupation, DM, asthma, and anemia in two LRAs, which compared participants with cataract surgery to those without cataract surgery and those having a cataract but without any cataract surgery, respectively. Hypertension, arthritis, and dyslipidemia were associated with cataract surgery at least in one of these LRAs. These results suggest that there are 9.4 million individuals with cataract and 1.7 million individuals with cataract surgery in Korea. Further studies are warranted to reveal the causality and its possible mechanism of developing/exacerbating cataract in novel determinants (i.e., anemia, asthma, and arthritic conditions) as well as well-known determinants.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Hyperglycemia and Hypo-HDL-cholesterolemia Are Primary Risk Factors for Age-related Cataract, and a Korean-style Balanced Diet has a Negative Association, based on the Korean Genome and Epidemiology Study
Donghyun Jee, Sunmin Park
J Korean Med Sci. 2021;36(23):e155. doi: 10.3346/jkms.2021.36.e155.
Reference
-
1. Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012; 96:614–618.2. Blindness C. Vision 2020: the cataract challenge. Community Eye Health. 2000; 13:17–19.3. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77.4. Park SJ, Lee JH, Woo SJ, Ahn J, Shin JP, Song SJ, Kang SW, Park KH; Epidemiologic Survey Committee of the Korean Ophthalmologic Society. Age-related macular degeneration: prevalence and risk factors from Korean National Health and Nutrition Examination Survey, 2008 through 2011. Ophthalmology. 2014; 121:1756–1765.5. Park SJ, Ahn S, Woo SJ, Park KH. Extent of exacerbation of chronic health conditions by visual impairment in terms of health-related quality of life. JAMA Ophthalmol. 2015; 133:1267–1275.6. Park SJ, Lee JH, Woo SJ, Kang SW, Park KH; Epidemiologic Survey Committee of Korean Ophthalmologic Society. Five heavy metallic elements and age-related macular degeneration: Korean National Health and Nutrition Examination Survey, 2008-2011. Ophthalmology. 2015; 122:129–137.7. Yoon KC, Mun GH, Kim SD, Kim SH, Kim CY, Park KH, Park YJ, Baek SH, Song SJ, Shin JP, et al. Prevalence of eye diseases in South Korea: data from the Korea National Health and Nutrition Examination Survey 2008-2009. Korean J Ophthalmol. 2011; 25:421–433.8. Chylack LT Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, Friend J, McCarthy D, Wu SY; The Longitudinal Study of Cataract Study Group. The Lens Opacities Classification System III. Arch Ophthalmol. 1993; 111:831–836.9. Seah SK, Wong TY, Foster PJ, Ng TP, Johnson GJ. Prevalence of lens opacity in Chinese residents of Singapore: the tanjong pagar survey. Ophthalmology. 2002; 109:2058–2064.10. Congdon N, Vingerling JR, Klein BE, West S, Friedman DS, Kempen J, O’Colmain B, Wu SY, Taylor HR; Eye Diseases Prevalence Research Group. Prevalence of cataract and pseudophakia/aphakia among adults in the United States. Arch Ophthalmol. 2004; 122:487–494.11. Athanasiov PA, Casson RJ, Sullivan T, Newland HS, Shein WK, Muecke JS, Selva D, Aung T. Cataract in rural Myanmar: prevalence and risk factors from the Meiktila Eye Study. Br J Ophthalmol. 2008; 92:1169–1174.12. Duan XR, Liang YB, Wang NL, Wong TY, Sun LP, Yang XH, Tao QS, Yuan RZ, Friedman DS. Prevalence and associations of cataract in a rural Chinese adult population: the Handan Eye Study. Graefes Arch Clin Exp Ophthalmol. 2013; 251:203–212.13. Mahdi AM, Rabiu M, Gilbert C, Sivasubramaniam S, Murthy GV, Ezelum C, Entekume G; Nigeria National Blindness and Visual Impairment Study Group. Prevalence and risk factors for lens opacities in Nigeria: results of the national blindness and low vision survey. Invest Ophthalmol Vis Sci. 2014; 55:2642–2651.14. Foster PJ, Wong TY, Machin D, Johnson GJ, Seah SK. Risk factors for nuclear, cortical and posterior subcapsular cataracts in the Chinese population of Singapore: the Tanjong Pagar Survey. Br J Ophthalmol. 2003; 87:1112–1120.15. Chang JR, Koo E, Agrón E, Hallak J, Clemons T, Azar D, Sperduto RD, Ferris FL 3rd, Chew EY; Age-Related Eye Disease Study Group. Risk factors associated with incident cataracts and cataract surgery in the Age-related Eye Disease Study (AREDS): AREDS report number 32. Ophthalmology. 2011; 118:2113–2119.16. Klein R, Klein BE, Jensen SC, Moss SE, Cruickshanks KJ. The relation of socioeconomic factors to age-related cataract, maculopathy, and impaired vision. The Beaver Dam Eye Study. Ophthalmology. 1994; 101:1969–1979.17. Klein BE, Klein R, Lee KE. Diabetes, cardiovascular disease, selected cardiovascular disease risk factors, and the 5-year incidence of age-related cataract and progression of lens opacities: the Beaver Dam Eye Study. Am J Ophthalmol. 1998; 126:782–790.18. Leske MC, Wu SY, Hennis A, Connell AM, Hyman L, Schachat A. Diabetes, hypertension, and central obesity as cataract risk factors in a black population. The Barbados Eye Study. Ophthalmology. 1999; 106:35–41.19. Christen WG, Glynn RJ, Manson JE, MacFadyen J, Bubes V, Schvartz M, Buring JE, Sesso HD, Gaziano JM. Effects of multivitamin supplement on cataract and age-related macular degeneration in a randomized trial of male physicians. Ophthalmology. 2014; 121:525–534.20. Tan JS, Wang JJ, Mitchell P. Influence of diabetes and cardiovascular disease on the long-term incidence of cataract: the Blue Mountains eye study. Ophthalmic Epidemiol. 2008; 15:317–327.21. Anderson GF. Universal health care coverage in Korea. Health Aff (Millwood). 1989; 8:24–34.22. Erie JC, Baratz KH, Hodge DO, Schleck CD, Burke JP. Incidence of cataract surgery from 1980 through 2004: 25-year population-based study. J Cataract Refract Surg. 2007; 33:1273–1277.23. Lansingh VC, Resnikoff S, Tingley-Kelley K, Nano ME, Martens M, Silva JC, Duerksen R, Carter MJ. Cataract surgery rates in latin america: a four-year longitudinal study of 19 countries. Ophthalmic Epidemiol. 2010; 17:75–81.24. International Federation of Health Plans (GB). 2012 Comparative price report. accessed on 3 March 2014. Available at http://www.ifhp.com.25. Roy CN. Anemia of inflammation. Hematology Am Soc Hematol Educ Program. 2010; 2010:276–280.26. Guralnik JM, Eisenstaedt RS, Ferrucci L, Klein HG, Woodman RC. Prevalence of anemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anemia. Blood. 2004; 104:2263–2268.27. Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med. 2005; 352:1011–1023.28. Girdhar A, Kumar V, Singh A, Menon B, Vijayan VK. Systemic inflammation and its response to treatment in patients with asthma. Respir Care. 2011; 56:800–805.29. Wood LG, Baines KJ, Fu J, Scott HA, Gibson PG. The neutrophilic inflammatory phenotype is associated with systemic inflammation in asthma. Chest. 2012; 142:86–93.30. National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): guidelines for the diagnosis and management of asthma-summary report 2007. J Allergy Clin Immunol. 2007; 120:S94–138.31. Weatherall M, Clay J, James K, Perrin K, Shirtcliffe P, Beasley R. Dose-response relationship of inhaled corticosteroids and cataracts: a systematic review and meta-analysis. Respirology. 2009; 14:983–990.32. Christen WG, Manson JE, Glynn RJ, Ajani UA, Schaumberg DA, Sperduto RD, Buring JE, Hennekens CH. Low-dose aspirin and risk of cataract and subtypes in a randomized trial of U.S. physicians. Ophthalmic Epidemiol. 1998; 5:133–142.33. Cumming RG, Mitchell P. Medications and cataract. The Blue Mountains Eye Study. Ophthalmology. 1998; 105:1751–1758.34. Rim TH, Kim MH, Kim WC, Kim TI, Kim EK. Cataract subtype risk factors identified from the Korea National Health and Nutrition Examination survey 2008-2010. BMC Ophthalmol. 2014; 14:4.