Korean J Gastroenterol.
2015 Sep;66(3):168-171. 10.4166/kjg.2015.66.3.168.
A Case of Splenic Tuberculosis Forming a Gastro-splenic Fistula
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. jawkim96@yonsei.ac.kr
- 2Department of Pathology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 2373334
- DOI: http://doi.org/10.4166/kjg.2015.66.3.168
Abstract
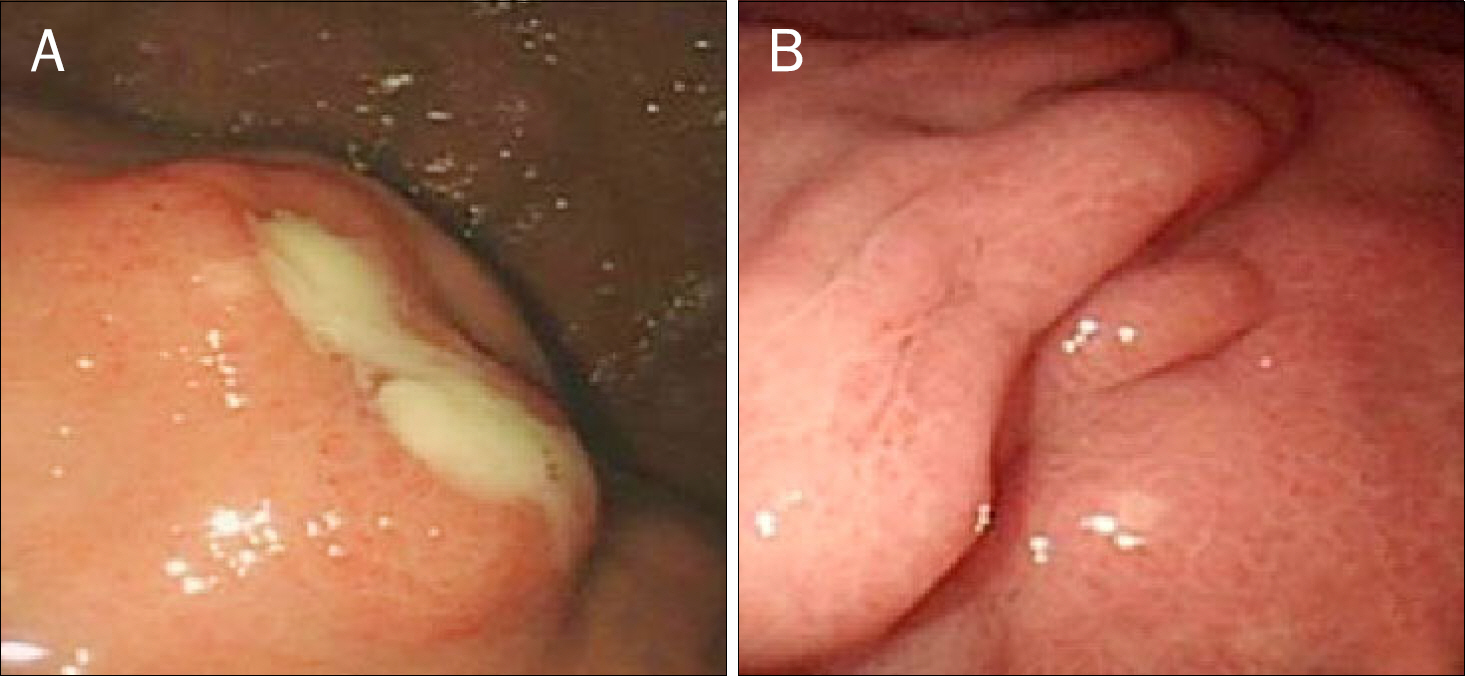
- We report a case of a 61-year-old man who presented with a cough and abdominal discomfort. CT scan of the chest showed two lesions across both lungs, and an abdominal CT scan revealed multiple hypodense lesions in the spleen with cystic lesions on the splenic hilum. Upper gastrointestinal tract endoscopy found creamy yellowish discharge through a fistula between the stomach and splenic hilum. Under fluoroscopic guidance, forceps was inserted into the fistula tract, and forcep biopsy was done. The pathology was consistent with tuberculosis, and a nine-month anti-tuberculosis medication regimen was started. Imaging performed three months after finishing medication indicated improvement of splenic lesions, and the gastro-splenic tract was sealed off. This case is a very rare clinical example of secondary splenic tuberculosis with a gastro-splenic fistula formation in an immunocompetent patient.
MeSH Terms
-
Antitubercular Agents/therapeutic use
Fluoroscopy
Gastric Fistula/pathology
Gastroscopy
Humans
Male
Middle Aged
Spleen/diagnostic imaging/pathology
Splenic Diseases/*diagnosis/diagnostic imaging/pathology
Tomography, X-Ray Computed
Tuberculosis, Splenic/*diagnosis/drug therapy/microbiology
Ultrasonography
Antitubercular Agents
Figure
Reference
-
References
1. Pramesh CS, Tamhankar AP, Rege SA, Shah SR. Splenic tuberculosis and HIV-1 infection. Lancet. 2002; 359:353.
Article2. Ho PL, Chim CS, Yuen KY. Isolated splenic tuberculosis presenting with pyrexia of unknown origin. Scand J Infect Dis. 2000; 32:700–701.3. Kim HH, Park SJ, Park MI, Moon W. Primary tuberculous abscess of the spleen in an immununocompetent patient diagnosed by biochemical markers and radiologic findings. J Clin Med Res. 2012; 4:149–151.
Article4. Raul SK, Tiwari S, Raina V, Sharma R, Joseph M. Tubercular splenic abscess in immunocompetent patients: a rare entity. Indian J Surg. 2009; 71:213–215.
Article5. Tung CC, Chen FC, Lo CJ. Splenic abscess: an easily overlooked disease? Am Surg. 2006; 72:322–325.
Article6. Gill RS, Gill SS, Mangat H, Logsetty S. Gastric perforation associated with tuberculosis: a case report. Case Rep Med. 2011; 2011:392769.
Article7. Nagi B, Lal A, Kochhar R, Bhasin DK, Thapa BR, Singh K. Perforations and fistulae in gastrointestinal tuberculosis. Acta Radiol. 2002; 43:501–506.
Article8. Sharma D, Gupta A, Jain BK, et al. Tuberculous gastric perforation: report of a case. Surg Today. 2004; 34:537–541.
Article9. Llenas-García J, Fernández-Ruiz M, Caurcel L, Enguita-Valls A, Vila-Santos J, Guerra-Vales JM. Splenic abscess: a review of 22 cases in a single institution. Eur J Intern Med. 2009; 20:537–539.
Article10. Sharma SK, Smith-Rohrberg D, Tahir M, Mohan A, Seith A. Radiological manifestations of splenic tuberculosis: a 23-patient case series from India. Indian J Med Res. 2007; 125:669–678.11. Ray S, Kundu S, Goswami M, Sarkar D, Saha M. Isolated tubercular splenic abscess: can we defer splenectomy? Our single experience with anti-tuberculous therapy alone. Indian J Med Microbiol. 2012; 30:101–103.
Article12. Kundu PR, Mathur SK, Singh S, Duhan A, Aggarwal G, Sen R. Isolated tuberculous splenic abscess in an immunocompetent individual. Asian Pac J Trop Med. 2011; 4:81–82.
Article13. Hamizah R, Rohana AG, Anwar SA, Ong TZ, Hamzaini AH, Zulkarnaen AN. Splenic tuberculosis presenting as pyrexia of unknown origin. Med J Malaysia. 2007; 62:70–71.14. Dede F, Doğ an E, Demir M, et al. Unusual presentation of tuberculosis as a splenic mass. Tohoku J Exp Med. 2006; 210:79–82.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Splenic Rupture as a Paradoxical Reaction during Treatment for Splenic Tuberculosis
- Suspected Case of Secondary Splenic Tuberculosis Difficult to Differentiate from Pyogenic Splenic Abscess
- A Case of Mass-Forming Splenic Tuberculosis: MRI Findings with Emphasis of Diffusion-Weighted Imaging Characteristics
- Recurrent Upper Gastrointestinal Bleeding from Gastro-Cystic Fistula and Pancreatic Pseudocyst Bleeding
- A Case of Tuberculous Splenic Abscess