Korean J Gastroenterol.
2015 May;65(5):297-305. 10.4166/kjg.2015.65.5.297.
Does Endoscopic Sphincterotomy and/or Cholecystectomy Reduce Recurrence Rate of Acute Biliary Pancreatitis?
- Affiliations
-
- 1Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. ringer2003@gmail.com
- KMID: 2373226
- DOI: http://doi.org/10.4166/kjg.2015.65.5.297
Abstract
- BACKGROUND/AIMS
Practice guidelines from international societies have recommended cholecystectomy during the same hospitalization for acute biliary pancreatitis (ABP). The aim of this study is to investigate the question of whether endoscopic sphincterotomy (EST) and/or cholecystectomy during the same hospitalization can reduce the recurrence rate of ABP.
METHODS
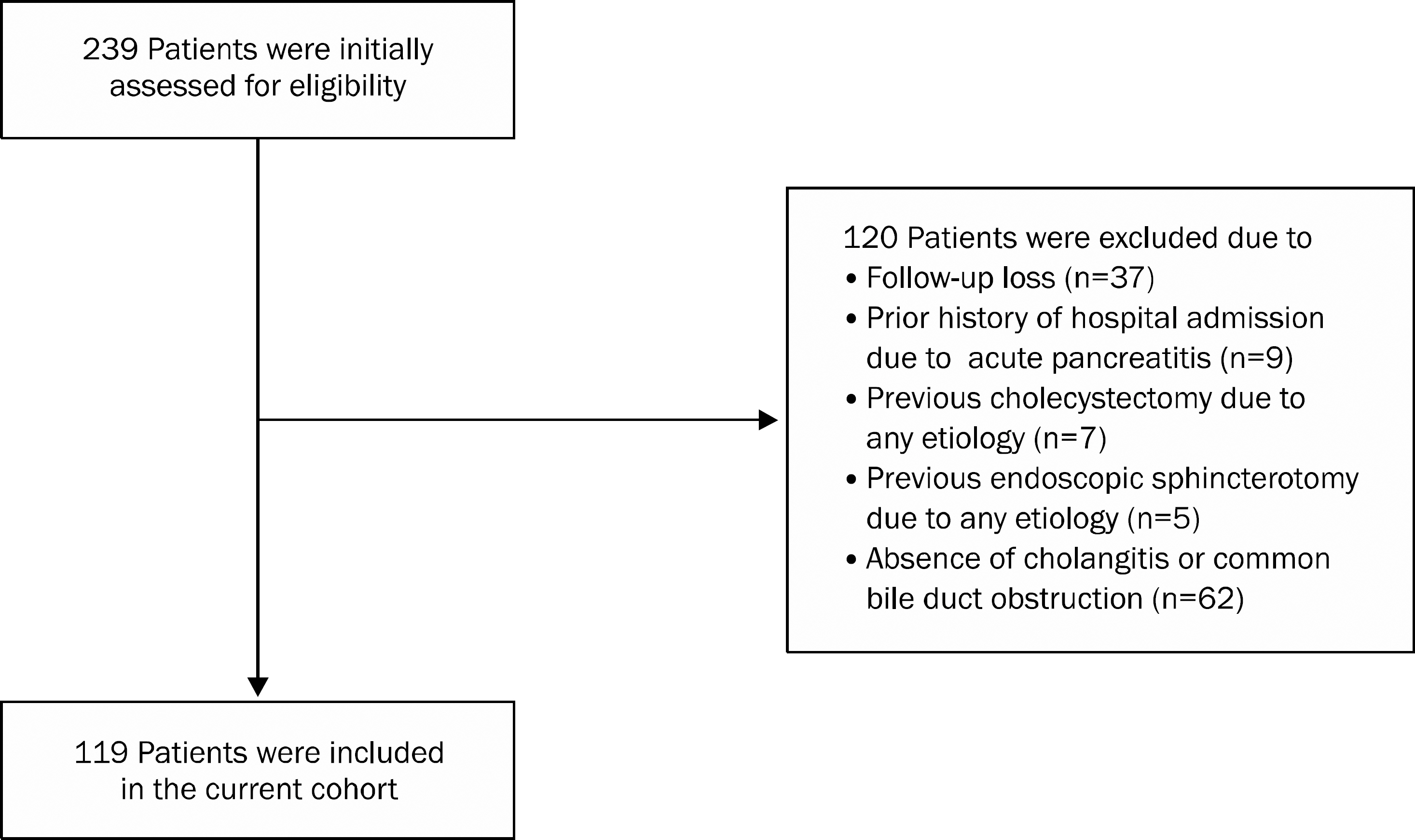
A total of 119 patients with ABP admitted to our institution between May 2005 and May 2010 who had complete follow-up data until May 2012 were enrolled.
RESULTS
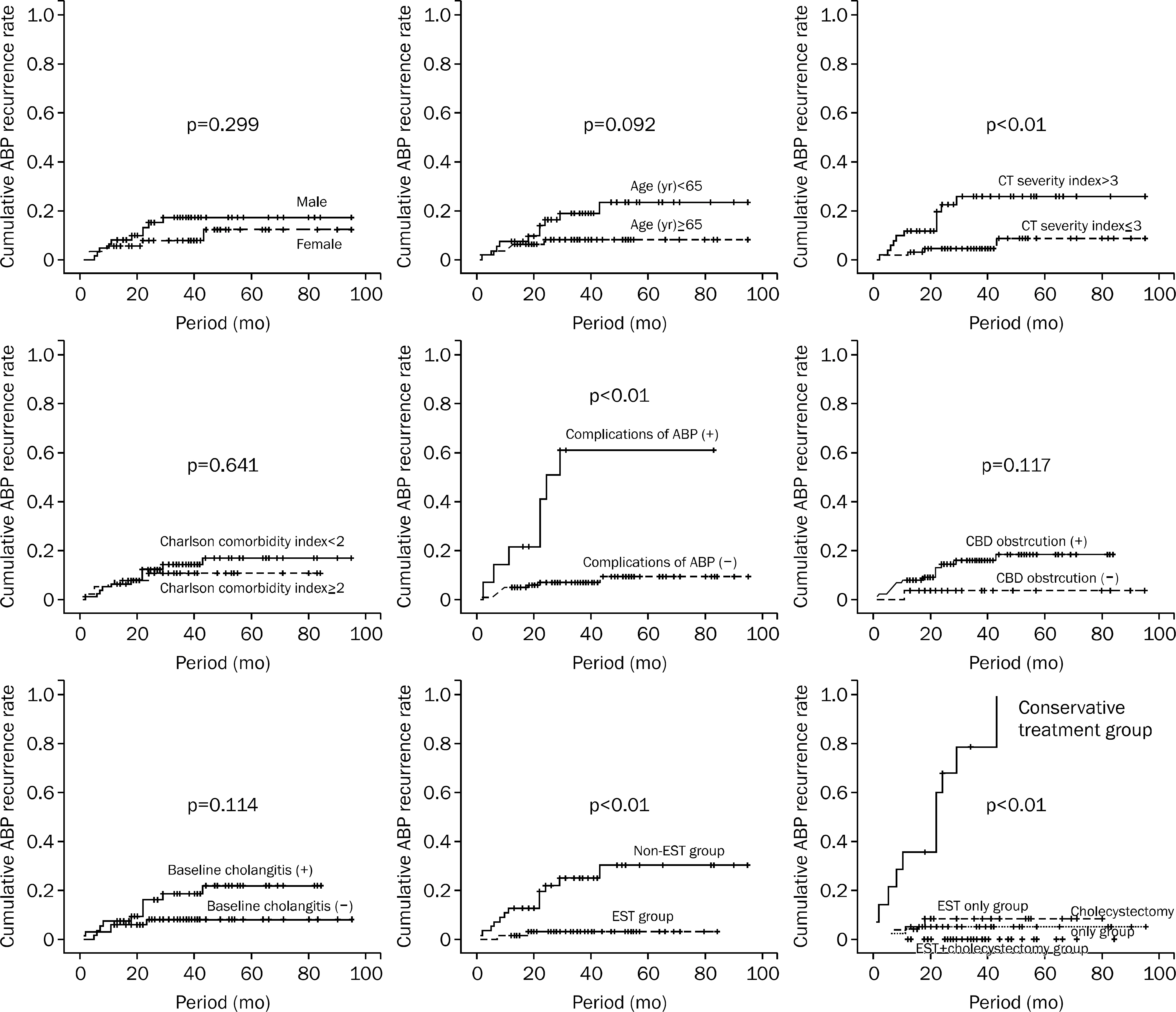
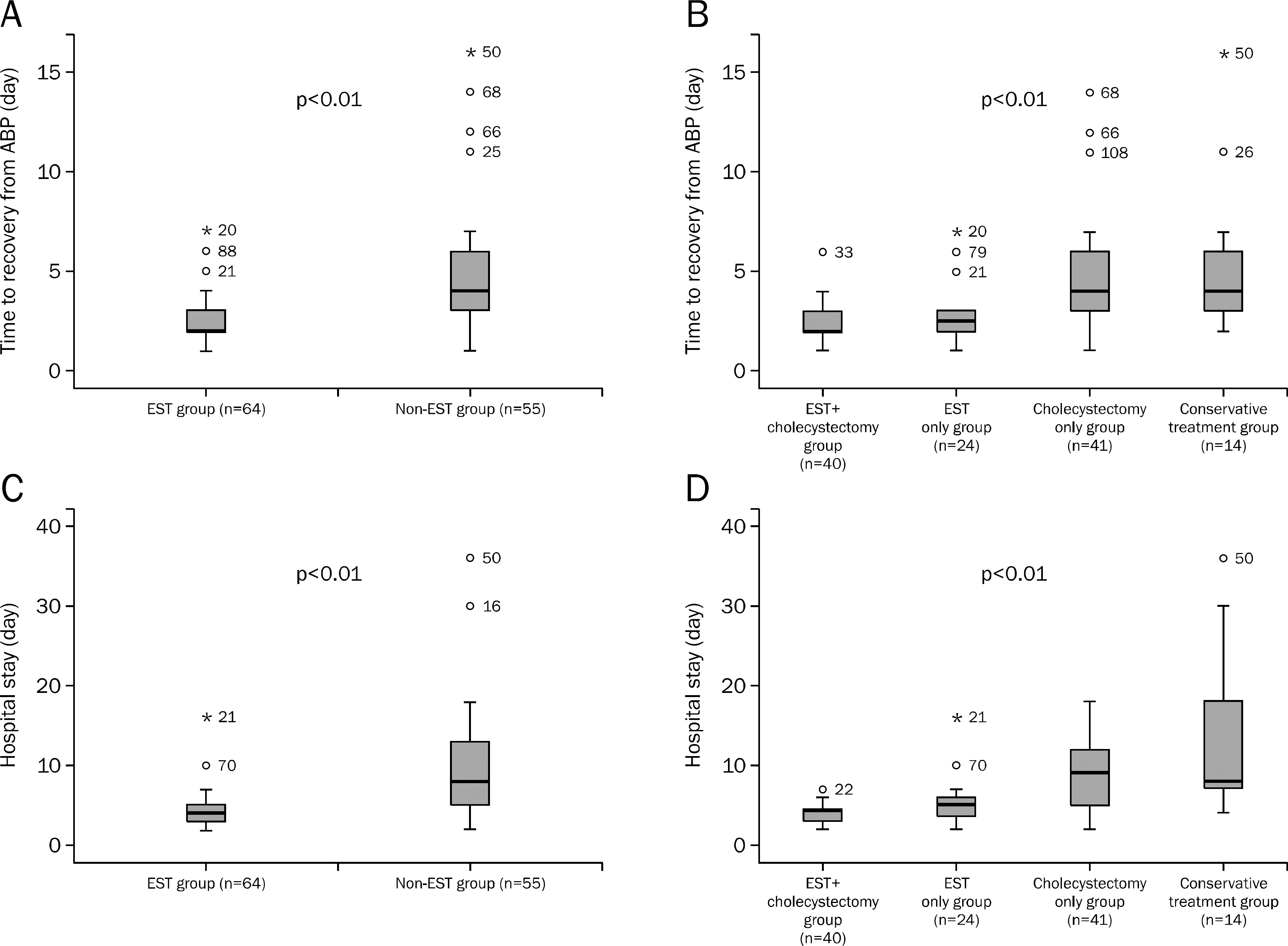
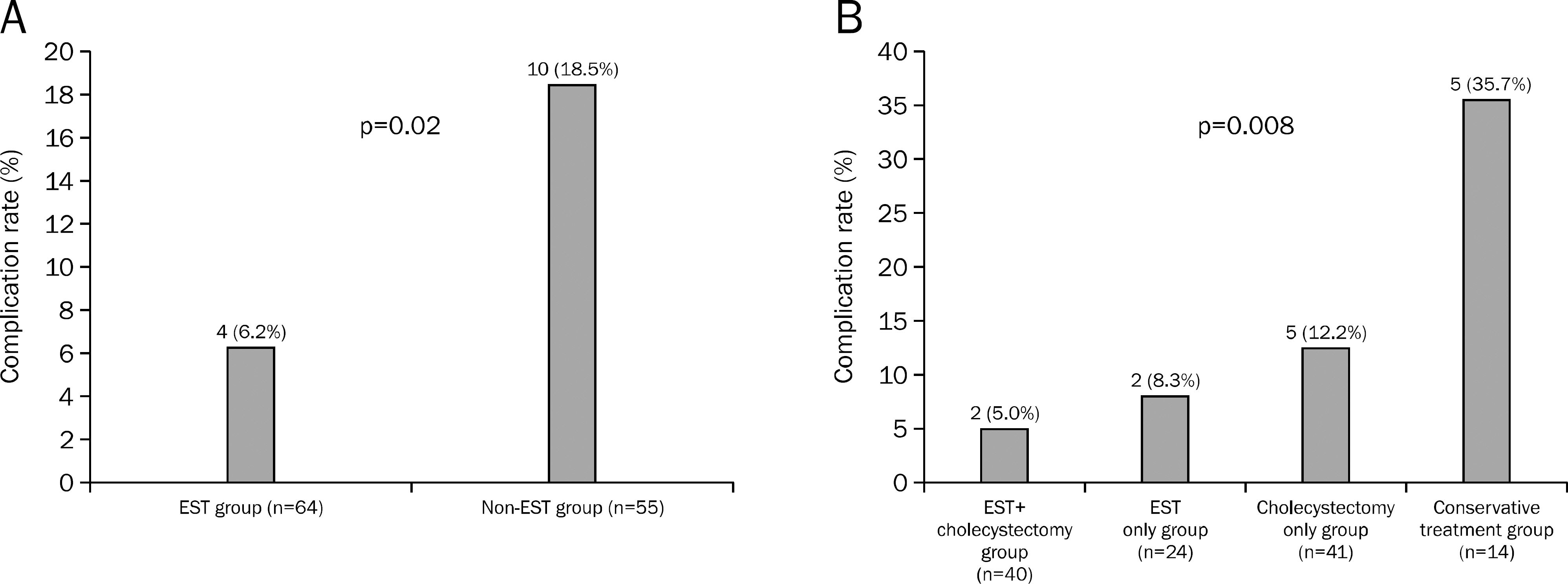
No significant differences in initial CT severity index and Charlson comorbidity index were observed between EST (n=64) and non-EST group (n=55) and among subgroups classified according to interventions performed. In Kaplan-Meier analyses, significantly higher recurrence rates of ABP were observed in the non-EST group compared to the EST group (p<0.01), and in the conservative treatment group compared to other intervention groups (p<0.01). The frequency of complications from ABP was significantly higher in the conservative treatment group (35.7%) and lowest in the EST plus cholecystectomy group (5.0%, p=0.008). In multivariate analysis, conservative treatment without EST and/or cholecystectomy, and non-EST group were independent risk factors for recurrence after the initial attack of ABP.
CONCLUSIONS
ERCP with EST and cholecystectomy during the index admission is associated with reduced recurrence rates of ABP.
MeSH Terms
-
Acute Disease
Adult
Aged
Cholangiopancreatography, Endoscopic Retrograde
Cholecystectomy, Laparoscopic
Cohort Studies
Female
Follow-Up Studies
Humans
Length of Stay
Male
Middle Aged
Multivariate Analysis
Odds Ratio
Pancreatitis/*pathology/surgery
Recurrence
Retrospective Studies
Severity of Illness Index
Sphincterotomy, Endoscopic
Tomography, X-Ray Computed
Treatment Outcome
Figure
Cited by 1 articles
-
The Protective Role of Endoscopic Sphincterotomy and/or Cholecystectomy for Recurrence of Acute Biliary Pancreatitis
Dong-Won Ahn
Korean J Gastroenterol. 2015;65(5):265-267. doi: 10.4166/kjg.2015.65.5.265.
Reference
-
References
1. Kimura Y, Arata S, Takada T, et al. Gallstone-induced acute pancreatitis. J Hepatobiliary Pancreat Sci. 2010; 17:60–69.
Article2. Toouli J, Brooke-Smith M, Bassi C, et al. Working Party of the Program Commitee of the Bangkok World Congress of Gastroenterology 2002. Guidelines for the management of acute pancreatitis. J Gastroenterol Hepatol. 2002; 17(Suppl):S15–S39.
Article3. Nguyen GC, Rosenberg M, Chong RY, Chong CA. Early cholecystectomy and ERCP are associated with reduced read-missions for acute biliary pancreatitis: a nationwide, pop-ulation-based study. Gastrointest Endosc. 2012; 75:47–55.
Article4. Uhl W, Warshaw A, Imrie C, et al. International Association of Pancreatology. IAP guidelines for the surgical management of acute pancreatitis. Pancreatology. 2002; 2:565–573.
Article5. van Geenen EJ, van der Peet DL, Bhagirath P, Mulder CJ, Bruno MJ. Etiology and diagnosis of acute biliary pancreatitis. Nat Rev Gastroenterol Hepatol. 2010; 7:495–502.
Article6. Oría A, Cimmino D, Ocampo C, et al. Early endoscopic intervention versus early conservative management in patients with acute gallstone pancreatitis and biliopancreatic obstruction: a randomized clinical trial. Ann Surg. 2007; 245:10–17.7. Tse F, Yuan Y. Early routine endoscopic retrograde cholangiopancreatography strategy versus early conservative management strategy in acute gallstone pancreatitis. Cochrane Database Syst Rev. 2012; 5:CD009779.
Article8. Uy MC, Daez ML, Sy PP, Banez VP, Espinosa WZ, Talingdan-Te MC. Early ERCP in acute gallstone pancreatitis without cholangitis: a meta-analysis. JOP. 2009; 10:299–305.9. van Geenen EJ, van der Peet DL, Mulder CJ, Cuesta MA, Bruno MJ. Recurrent acute biliary pancreatitis: the protective role of cholecystectomy and endoscopic sphincterotomy. Surg Endosc. 2009; 23:950–956.
Article10. Lee JK, Ryu JK, Park JK, et al. Roles of endoscopic sphincterotomy and cholecystectomy in acute biliary pancreatitis. Hepatogastroenterology. 2008; 55:1981–1985.11. Banks PA, Freeman ML. Practice Parameters Committee of the American College of Gastroenterology. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006; 101:2379–2400.
Article12. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383.
Article13. Balthazar EJ, Robinson DL, Megibow AJ, Ranson JH. Acute pancreatitis: value of CT in establishing prognosis. Radiology. 1990; 174:331–336.
Article14. Sandzén B, Haapamäki MM, Nilsson E, Stenlund HC, Oman M. Cholecystectomy and sphincterotomy in patients with mild acute biliary pancreatitis in Sweden 1988–2003: a nationwide register study. BMC Gastroenterol. 2009; 9:80.
Article15. Ayub K, Slavin J, Imada R. WITHDRAWN. Endoscopic retrograde cholangiopancreatography in gallstone-associated acute pancreatitis. Cochrane Database Syst Rev. 2010; 1:CD003630.16. Boerma D, Rauws EA, Keulemans YC, et al. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. Lancet. 2002; 360:761–765.
Article17. McAlister VC, Davenport E, Renouf E. Cholecystectomy deferral in patients with endoscopic sphincterotomy. Cochrane Database Syst Rev. 2007; 4:CD006233.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Indications and Timing of ERCP and Cholecystectomy for Biliary Pancreatitis
- The Roles of Endoscopic Sphincterotomy and Cholecystectomy in Acute Biliary Pancreatitis
- Management of Biliary Pancreatitis in the Laparoscopic Era
- Evaluation and Treatment of Recurrent Acute Pancreatitis
- Endoscopic Sphincterotomy, Balloon Stone Extraction, and Basket Stone Extraction