J Pathol Transl Med.
2017 Mar;51(2):180-184. 10.4132/jptm.2016.08.30.
Mucinous Cystadenoma of the Testis: A Case Report with Immunohistochemical Findings
- Affiliations
-
- 1Department of Pathology, Medical Research Center, Seoul National University College of Medicine, Seoul, Korea. blue7270@snu.ac.kr
- 2Kidney Research Institute, Medical Research Center, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2372969
- DOI: http://doi.org/10.4132/jptm.2016.08.30
Abstract
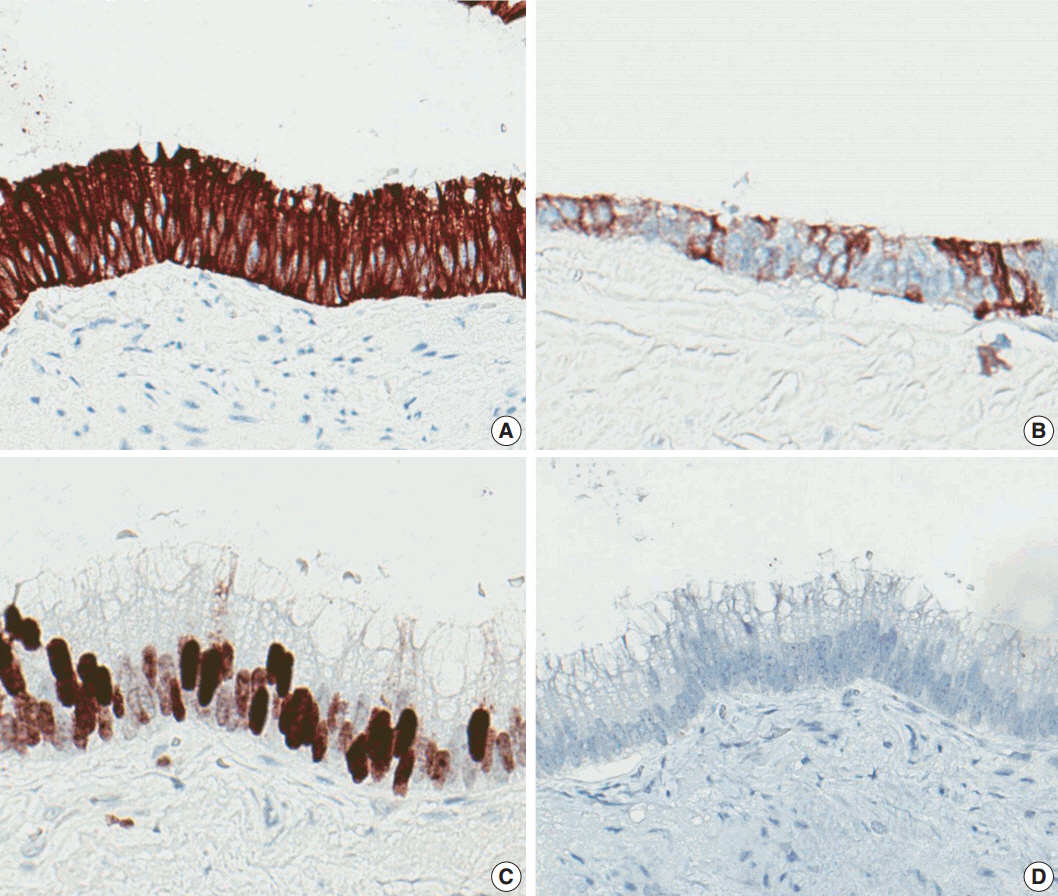
- Mucinous cystadenoma of the testis is a very rare tumor. Herein, we report a case of mucinous cystadenoma arising in the testis of a 61-year-old man, along with a literature review. Computed tomography showed a 2.5-cm-sized poorly enhancing cystic mass. Grossly, the tumor was a unilocular cystic mass filled with mucinous material and confined to the testicular parenchyma. Histologically, the cyst had a fibrotic wall lined by mucinous columnar epithelium without atypia. Immunohistochemical staining was positive for cytokeratin 20 and CDX2, as well as focally positive for cytokeratin 7. The pathologic diagnosis was mucinous cystadenoma.
Keyword
Figure
Reference
-
1. Elliott JE, Klein JR, Drachenberg DE. Primary testicular mucinous neoplasms: case report and literature review. Can Urol Assoc J. 2010; 4:E112–5.
Article2. Shimbo M, Araki K, Kaibuchi T, Kuramochi H, Mori I. Mucinous cystadenoma of the testis. J Urol. 2004; 172:146–7.
Article3. Park KM, Cho NB, Song KY. A serous papillary cystadenoma of low malignant potential in paratesticular tissue. Korean J Pathol. 1996; 30:463–5.4. Kim JY, Lee YT, Kang HJ, Lee CH. Primary mucinous cystadenoma of the spermatic cord within the inguinal canal. Diagn Pathol. 2012; 7:139.
Article5. Park MI, Kim HS, Suh KS, Kang DY. Paratesticular papillary serous tumor of low malignant potential: a case report. Korean J Pathol. 2004; 38:427–9.6. Park HJ, Park SW, Chon WH, Jung SG, Park NC. A serous papillary cystadenoma of borderline malignancy in testis. Korean J Androl. 2007; 25:36–8.7. Weon HC, Kim IS, Jang CS, Hong SJ, Lee MS. Papillary mucinous cystadenoma, paratesticular: a case report. Korean J Urol. 1986; 27:359–60.8. Celdran JO, Rodriguez CS, Valverde FM, Compiano LO. Primary mucinous cystadenocarcinoma of the testis: an extremely rare ovarian-type surface epithelial carcinoma. J Cancer Res Ther. 2015; 11:647.9. Nokubi M, Kawai T, Mitsu S, Ishikawa S, Morinaga S. Mucinous cystadenoma of the testis. Pathol Int. 2002; 52:648–52.
Article10. Naito S, Yamazumi K, Yakata Y, et al. Immunohistochemical examination of mucinous cystadenoma of the testis. Pathol Int. 2004; 54:355–9.
Article11. Alasio TM, Borin J, Taylor K, Bar-Chama N, Unger PD. Intratesticular mucinous cystadenoma: immunohistochemical comparison with ovarian and colonic tissue. Arch Pathol Lab Med. 2005; 129:399–402.
Article12. Burger T, Schildhaus HU, Inniger R, et al. Ovarian-type epithelial tumours of the testis: immunohistochemical and molecular analysis of two serous borderline tumours of the testis. Diagn Pathol. 2015; 10:118.
Article13. Olla L, Di Naro N, Puliga G, Tolu GA. Intraparenchymal serous papillary cystadenoma of the testis: a case report. Pathologica. 2013; 105:15–7.14. Remmele W, Kaiserling E, Zerban U, et al. Serous papillary cystic tumor of borderline malignancy with focal carcinoma arising in testis: case report with immunohistochemical and ultrastructural observations. Hum Pathol. 1992; 23:75–9.
Article15. Ulbright TM, Young RH. Primary mucinous tumors of the testis and paratestis: a report of nine cases. Am J Surg Pathol. 2003; 27:1221–8.16. Amin MB. Selected other problematic testicular and paratesticular lesions: rete testis neoplasms and pseudotumors, mesothelial lesions and secondary tumors. Mod Pathol. 2005; 18 Suppl 2:S131–45.
Article17. Young RH, Scully RE. Testicular and paratesticular tumors and tumor-like lesions of ovarian common epithelial and mullerian types: a report of four cases and review of the literature. Am J Clin Pathol. 1986; 86:146–52.
Article18. Vang R, Gown AM, Wu LS, et al. Immunohistochemical expression of CDX2 in primary ovarian mucinous tumors and metastatic mucinous carcinomas involving the ovary: comparison with CK20 and correlation with coordinate expression of CK7. Mod Pathol. 2006; 19:1421–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Papillary Mucinous Cystadenoma, Paratesticular: A Case Report
- A Case of Mucinous Cystadenoma of the Pancreas
- A Serous Papillary Cystadenoma of Borderline Malignancy in Testis
- A Case of a Choledochal Cyst with a Mucinous Cystadenoma of the Pancreas
- A case of Huge Ovarian Mucinous Cystadenoma associated with 37 weeks' Gestation