Obstet Gynecol Sci.
2017 Mar;60(2):139-144. 10.5468/ogs.2017.60.2.139.
No fault compensation in perinatal medicine in Japan-from results for 8 years
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Kyorin University School of Medicine, Tokyo, Japan. iwashita@ks.kyorin-u.ac.jp
- KMID: 2372797
- DOI: http://doi.org/10.5468/ogs.2017.60.2.139
Abstract
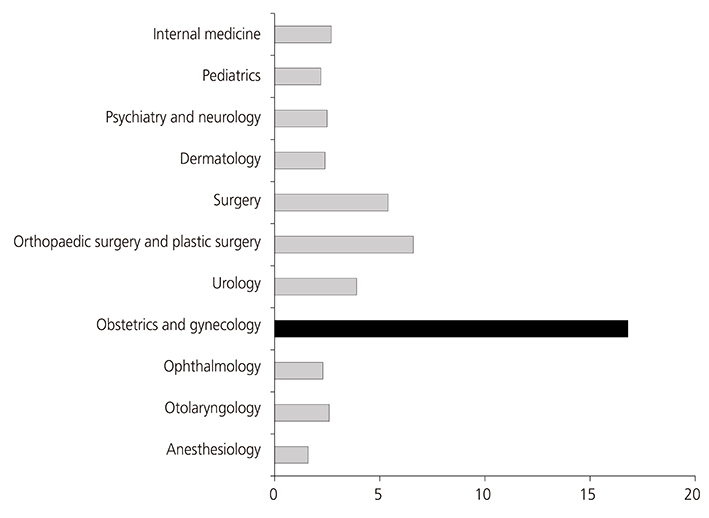
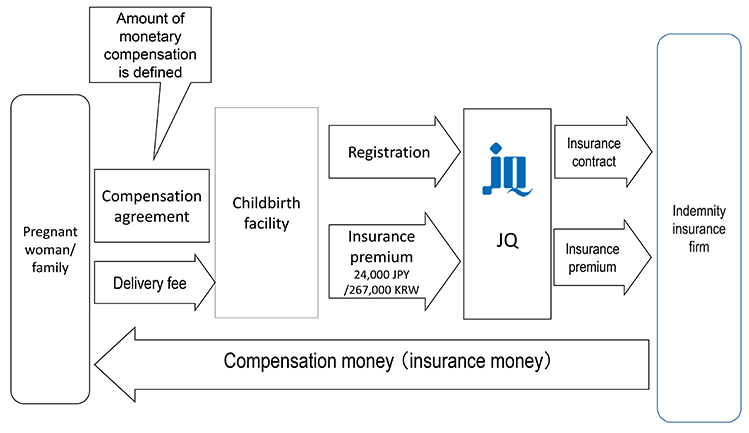
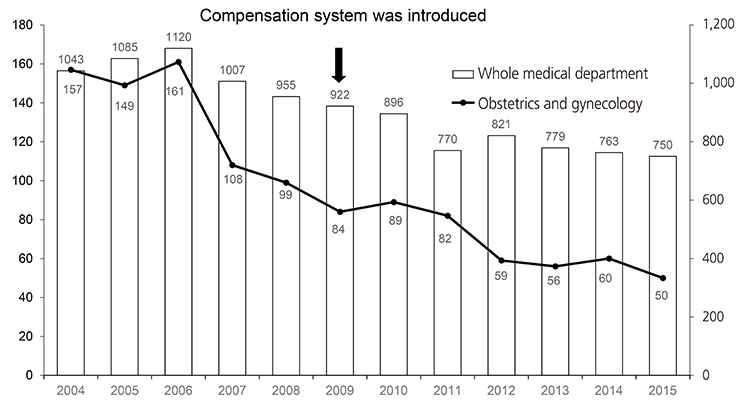
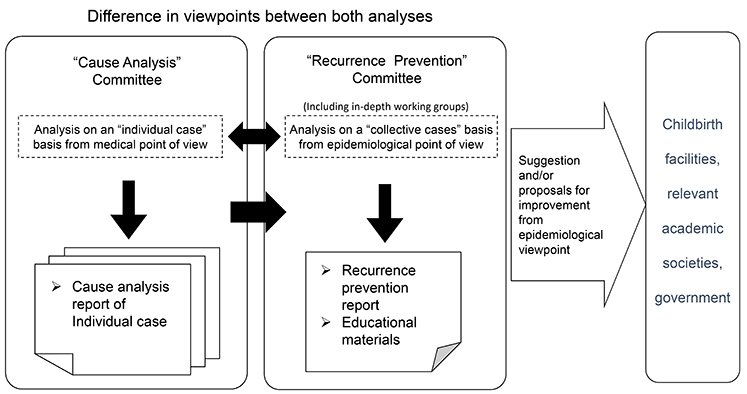
- No fault compensation in perinatal medicine has been established to provide aid to patients in the event of disability due to a medical accident during delivery and to strive to resolve disputes quickly that contributes to reduce medical malpractice suit in the field of perinatal medicine. Furthermore, this system is aimed to establish a mechanism that achieves higher quality of obstetric care by analyzing the causes of accidents. This system is operated by Japan Council for Quality Health Care and 99.9% of childbirth facilities in Japan registered with this compensation system. Compensation system has two major functions including compensation and cause analysis and recurrence prevention based on cases. Compensation eligibility is reviewed in the Review Committee at the organization in Japan Council for Quality Health Care and currently 1,717 cases are judged as eligible cases out of 2,250 since 2009. The cause of each eligible case is analyzed in the Cause Analysis Committee one by one. The Cause Analysis Committee has 7 independent subcommittee and each subcommittee members are consistent of obstetricians, neonatologists, pediatricians, midwives and lawyers. Original cause analysis report is sent to childbirth facility and patient's family. Questionnaire survey demonstrated that 73% of childbirth facilities and 65% of patient family were satisfied with the cause analysis report. The number of medical lawsuit in obstetrics and gynecology is significantly decreased compared to those in all medical departments since the compensation system was introduced suggesting that these cause analysis reports may contribute the decrease in medical lawsuits. The major purpose of the Recurrence Prevention Committee is striving to prevent future cases of cerebral palsy and to improve the quality of obstetric care. To accomplish the purpose, the committee routinely collect information from individual cases and analyze quantitatively and epidemiologically. Furthermore the committee choose subject from cases to discuss for future prevention and provide wide public disclosure of the information with recommendation. The committee issued 6 reports until now and these reports have been distributed to childbirth facilities, perinatal medicine-related scientific society and administrative agencies.
MeSH Terms
Figure
Cited by 1 articles
-
Management of disseminated intravascular coagulation associated with placental abruption and measures to improve outcomes
Jun Takeda, Satoru Takeda
Obstet Gynecol Sci. 2019;62(5):299-306. doi: 10.5468/ogs.2019.62.5.299.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Issues in Obstetric No Fault Compensation Act and Suggestions for the Improvement
- The influence of obstetric no-fault compensation act on future career of residents in obstetrics and gynecology
- Bench-marking of Japanese Perinatal Center System for Improving Maternal and Neonatal Outcome in Korea
- Analysis of the difference in the perinatal mortality rate between white-collar and blue-collar workers in Japan, 1995-2015
- Perinatal Care Center System for High Risk Pregnancy and Newborn in Japan