Ann Hepatobiliary Pancreat Surg.
2017 Feb;21(1):39-47. 10.14701/ahbps.2017.21.1.39.
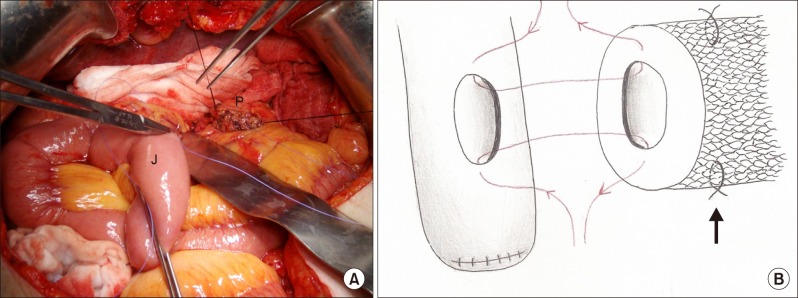
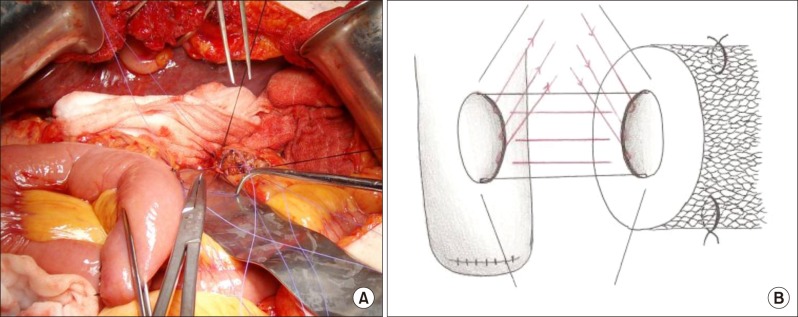
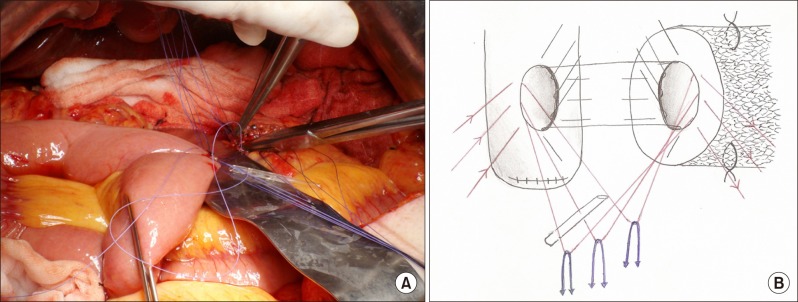
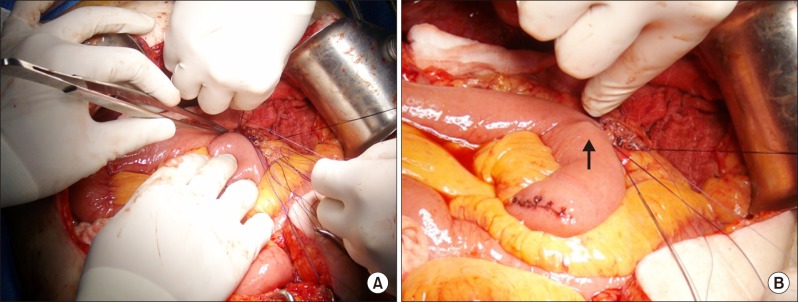
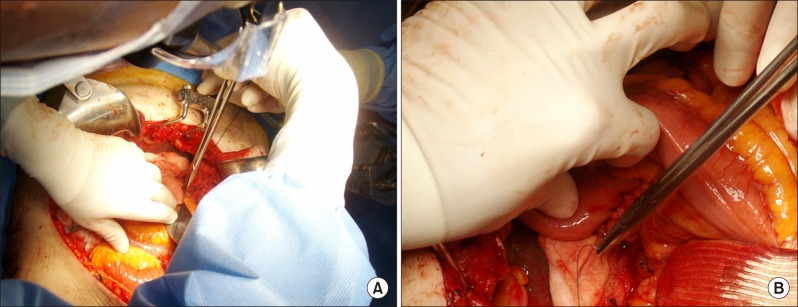
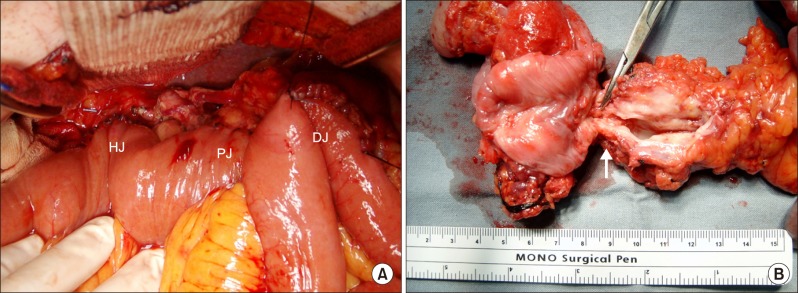
An intuitive method of duct-to-mucosa pancreaticojejunostomy after pancreaticoduodenectomy: use of one-step circumferential interrupted sutures
- Affiliations
-
- 1Department of Surgery, Inha University School of Medicine, Incheon, Korea. 196087@inha.ac.kr
- KMID: 2371566
- DOI: http://doi.org/10.14701/ahbps.2017.21.1.39
Abstract
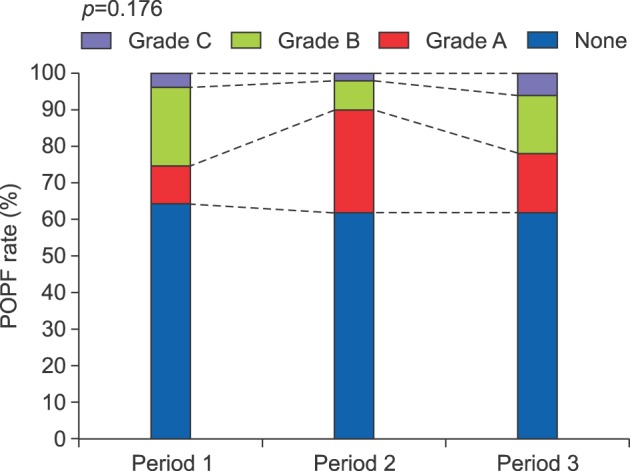
- Pancreaticoenteric anastomosis is the origin of postoperative pancreatic fistula (POPF). Although a variety of methods have been proposed to decrease the POPF rate, randomized controlled trials performed so far have failed to demonstrate superiority of any particular method to the others. Cattell-Warren duct-to-mucosa pancreaticojejunostomy (PJ) is a widely practiced procedure. Their method is challenging, especially when the pancreatic duct is small. We assumed that the difficulty resides in the pancreatic duct becoming difficult to access when the posterior row is tied before suturing the anterior row. We have modified the duct-to-mucosa PJ so that the entire circumference of the inner layer can be sutured and tied in one-step by anchoring and retracting the anterior row. The jejunal roux-limb and pancreatic stump are positioned spatially apart, allowing enough space for free needle work. During a 13-year period, 151 patients underwent pancreaticoduodenectomy with this method, and the cumulative POPF and mortality rates were 37.1% and 4.6%, respectively. These rates were stable throughout the study period, implicating a relative independence from surgeons' experience. We believe that our method is intuitive, easy to grasp, and can be readily adopted even by surgeons not accustomed to pancreaticoduodenectomy.
MeSH Terms
Figure
Reference
-
1. Barens SA, Lillemoe KD, Kaufman HS, Sauter PK, Yeo CJ, Talamini MA, et al. Pancreaticoduodenectomy for benign disease. Am J Surg. 1996; 171:131–134. PMID: 8554127.2. Diener MK, Knaebel HP, Heukaufer C, Antes G, Büchler MW, Seiler CM. A systematic review and meta-analysis of pylorus-preserving versus classical pancreaticoduodenectomy for surgical treatment of periampullary and pancreatic carcinoma. Ann Surg. 2007; 245:187–200. PMID: 17245171.
Article3. Machado NO. Pancreatic fistula after pancreatectomy: definitions, risk factors, preventive measures, and management-review. Int J Surg Oncol. 2012; 2012:602478. PMID: 22611494.4. Tewari M, Hazrah P, Kumar V, Shukla HS. Options of restorative pancreaticoenteric anastomosis following pancreaticoduodenectomy: a review. Surg Oncol. 2010; 19:17–26. PMID: 19231161.
Article5. Fernández-Cruz L, Belli A, Acosta M, Chavarria EJ, Adelsdorfer W, López-Boado MA, et al. Which is the best technique for pancreaticoenteric reconstruction after pancreaticoduodenectomy? A critical analysis. Surg Today. 2011; 41:761–766. PMID: 21626319.
Article6. Crippa S, Cirocchi R, Randolph J, Partelli S, Belfiori G, Piccioli A, et al. Pancreaticojejunostomy is comparable to pancreaticogastrostomy after pancreaticoduodenectomy: an updated meta-analysis of randomized controlled trials. Langenbecks Arch Surg. 2016; 401:427–437. PMID: 27102322.
Article7. Chen YJ, Lai EC, Lau WY, Chen XP. Enteric reconstruction of pancreatic stump following pancreaticoduodenectomy: a review of the literature. Int J Surg. 2014; 12:706–711. PMID: 24851718.
Article8. Hua J, He Z, Qian D, Meng H, Zhou B, Song Z. Duct-to-Mucosa versus invagination pancreaticojejunostomy following pancreaticoduodenectomy: a systematic review and meta-analysis. J Gastrointest Surg. 2015; 19:1900–1909. PMID: 26264363.
Article9. Zhang JL, Xiao ZY, Lai DM, Sun J, He CC, Zhang YF, et al. Comparison of duct-to-mucosa and end-to-side pancreaticojejunostomy reconstruction following pancreaticoduodenectomy. Hepatogastroenterology. 2013; 60:176–179. PMID: 22773303.
Article10. Osada S, Imai H, Sasaki Y, Tanaka Y, Nonaka K, Yoshida K. Reconstruction method after pancreaticoduodenectomy. Idea to prevent serious complications. JOP. 2012; 13:1–6. PMID: 22233940.11. Ball CG, Howard TJ. Does the type of pancreaticojejunostomy after Whipple alter the leak rate? Adv Surg. 2010; 44:131–148. PMID: 20919519.
Article12. Warren KW, Cattell RB. Basic techniques in pancreatic surgery. Surg Clin North Am. 1956; 36:707–724. PMID: 13324659.
Article13. Akamatsu N, Sugawara Y, Komagome M, Shin N, Cho N, Ishida T, et al. Risk factors for postoperative pancreatic fistula after pancreaticoduodenectomy: the significance of the ratio of the main pancreatic duct to the pancreas body as a predictor of leakage. J Hepatobiliary Pancreat Sci. 2010; 17:322–328. PMID: 20464562.
Article14. Kennedy EP, Yeo CJ. Dunking pancreaticojejunostomy versus duct-to-mucosa anastomosis. J Hepatobiliary Pancreat Sci. 2011; 18:769–774. PMID: 21845376.
Article15. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13. PMID: 16003309.
Article16. Bassi C, Falconi M, Molinari E, Mantovani W, Butturini G, Gumbs AA, et al. Duct-to-mucosa versus end-to-side pancreaticojejunostomy reconstruction after pancreaticoduodenectomy: results of a prospective randomized trial. Surgery. 2003; 134:766–771. PMID: 14639354.
Article17. Bai X, Zhang Q, Gao S, Lou J, Li G, Zhang Y, et al. Duct-to-Mucosa vs Invagination for Pancreaticojejunostomy after pancreaticoduodenectomy: a prospective, randomized controlled trial from a single surgeon. J Am Coll Surg. 2016; 222:10–18. PMID: 26577499.
Article18. Berger AC, Howard TJ, Kennedy EP, Sauter PK, Bower-Cherry M, Dutkevitch S, et al. Does type of pancreaticojejunostomy after pancreaticoduodenectomy decrease rate of pancreatic fistula? A randomized, prospective, dual-institution trial. J Am Coll Surg. 2009; 208:738–747. PMID: 19476827.
Article19. Batignani G, Fratini G, Zuckermann M, Bianchini E, Tonelli F. Comparison of Wirsung-jejunal duct-to-mucosa and dunking technique for pancreatojejunostomy after pancreatoduodenectomy. Hepatobiliary Pancreat Dis Int. 2005; 4:450–455. PMID: 16109535.20. Xu J, Zhang B, Shi S, Qin Y, Ji S, Xu W, et al. Papillary-like main pancreatic duct invaginated pancreaticojejunostomy versus duct-to-mucosa pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Surgery. 2015; 158:1211–1218. PMID: 26036878.21. El Nakeeb A, El Hemaly M, Askr W, Abd Ellatif M, Hamed H, Elghawalby A, et al. Comparative study between duct to mucosa and invagination pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized study. Int J Surg. 2015; 16:1–6. PMID: 25682724.
Article22. Ohwada S, Ogawa T, Kawate S, Tanahashi Y, Iwazaki S, Tomizawa N, et al. Results of duct-to-mucosa pancreaticojejunostomy for pancreaticoduodenectomy Billroth I type reconstruction in 100 consecutive patients. J Am Coll Surg. 2001; 193:29–35. PMID: 11442251.
Article23. Maharaj R, Naraynsingh V, Shukla PJ. Concept of a duct-to-mucosa pancreaticojejunostomy. J Am Coll Surg. 2010; 211:143. PMID: 20610265.
Article24. Liu C, Long J, Liu L, Xu J, Zhang B, Yu X, et al. Pancreatic stump-closed pancreaticojejunostomy can be performed safely in normal soft pancreas cases. J Surg Res. 2012; 172:e11–e17. PMID: 22079848.
Article25. Imaizumi T, Harada N, Hatori T, Fukuda A, Takasaki K. Stenting is unnecessary in duct-to-mucosa pancreaticojejunostomy even in the normal pancreas. Pancreatology. 2002; 2:116–121. PMID: 12123091.
Article26. Smyrniotis V, Arkadopoulos N, Kyriazi MA, Derpapas M, Theodosopoulos T, Gennatas C, et al. Does internal stenting of the pancreaticojejunostomy improve outcomes after pancreatoduodenectomy? A prospective study. Langenbecks Arch Surg. 2010; 395:195–200. PMID: 20082094.
Article27. Ohwada S, Tanahashi Y, Ogawa T, Kawate S, Hamada K, Tago KI, et al. In situ vs ex situ pancreatic duct stents of duct-to-mucosa pancreaticojejunostomy after pancreaticoduodenectomy with billroth I-type reconstruction. Arch Surg. 2002; 137:1289–1293. PMID: 12413321.
Article28. Zhou Y, Zhou Q, Li Z, Lin Q, Gong Y, Chen R. The impact of internal or external transanastomotic pancreatic duct stents following pancreaticojejunostomy. Which one is better? A meta-analysis. J Gastrointest Surg. 2012; 16:2322–2335. PMID: 23011201.
Article29. Tani M, Kawai M, Hirono S, Ina S, Miyazawa M, Shimizu A, et al. A prospective randomized controlled trial of internal versus external drainage with pancreaticojejunostomy for pancreaticoduodenectomy. Am J Surg. 2010; 199:759–764. PMID: 20074698.
Article30. Keck T, Wellner UF, Bahra M, Klein F, Sick O, Niedergethmann M, et al. Pancreatogastrostomy versus pancreatojejunostomy for RECOnstruction after PANCreatoduodenectomy (RECOPANC, DRKS 00000767): perioperative and long-term results of a multicenter randomized controlled trial. Ann Surg. 2016; 263:440–449. PMID: 26135690.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Duct to mucosa method for a pancreaticojejun-ostomy:continuous stitches modification
- Efficacy of Stented Pancreaticojejunostomy and Jejunojejunostomy after Pancreaticoduodenectomy
- The Complication Rate according to the Method of Pancreaticojejunostomy after Pancreaticoduodenectomy
- Anterior pancreatic duct split prior to duct-to-mucosa pancreatico-jejunal anastomosis in pancreaticoduodenectomy
- Pancreatic Fistula after Pancreaticoduodenectomy: A Comparison between the Two Pancreaticojejunostomy Methods for Approximating the Pancreatic Parenchyma to the Jejunal Seromuscular Layer: Interrupted Vs. Continuous Stitches