Anesth Pain Med.
2017 Jan;12(1):68-71. 10.17085/apm.2017.12.1.68.
Prediction of midline depth from skin to cervical epidural space by lateral cervical spine X-ray
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Soonchunhyang University Seoul Hospital, Seoul, Korea. sauronia@lycos.co.kr
- KMID: 2369670
- DOI: http://doi.org/10.17085/apm.2017.12.1.68
Abstract
- BACKGROUND
Previous studies have shown that measuring the distance from the skin to the ligamentum flavum by ultrasound preceding cervical epidural block can be beneficial in excluding false loss of resistance. However, the measurement value using ultrasound may vary depending on the degree of operator experience. Therefore, we aimed to determine the depth from skin to cervical epidural space by using lateral cervical spine X-ray, which is a more intuitive method.
METHODS
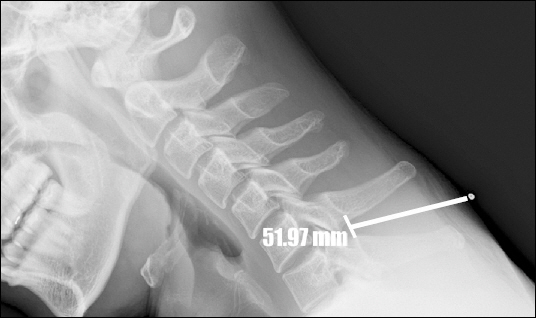
We enrolled 102 adult patients who were scheduled to undergo cervical epidural anesthesia for vascular bypass surgery of upper arm. After attaching a steel rod on the needle insertion site, lateral cervical spine X-ray was taken before the epidural procedure. We measured the distance from the steel rod to the midpoint of interlaminar space on the spinolaminar line. The X-ray depth was compared with needle depth.
RESULTS
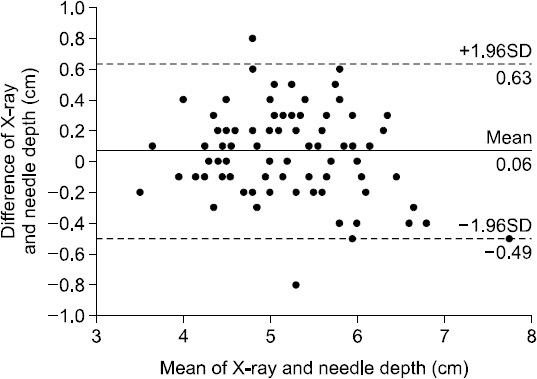
Of the 102 enrolled patients, 18 patients including 13 in whom we were unable to measure X-ray depth were excluded from the analysis. In total, 84 patients were included in the analysis. Concordance correlation coefficient between the X-ray-measured depth and needle depth was 0.925. Bland-Altman analysis indicated a mean difference of ± 1.96 SD with 0.06 ± 0.56 cm.
CONCLUSIONS
Lateral cervical spine X-ray can be useful for prediction of the midline depth from skin to epidural space, particularly for operators who are not skilled at spine ultrasound or the use the C-arm fluoroscopy.
Keyword
MeSH Terms
Figure
Reference
-
1. Zhao Q, Huang K, An J, Fang Q, Wen H, Qian X, et al. The distance from skin to cervical and high thoracic epidural space on chinese adults as read from MRI. Pain Physician. 2014; 17:163–8. PMID: 24658477.2. Lirk P, Kolbitsch C, Putz G, Colvin J, Colvin HP, Lorenz I, et al. Cervical and high thoracic ligamentum flavum frequently fails to fuse in the midline. Anesthesiology. 2003; 99:1387–90. DOI: 10.1097/00000542-200312000-00023. PMID: 14639154.3. Pak MH, Lee WH, Ko YK, So SY, Kim HJ. Ultrasonographic measurement of the ligamentum flavum depth;is it a reliable method to distinguish true and false loss of resistance? Korean J Pain. 2012; 25:99–104. DOI: 10.3344/kjp.2012.25.2.99. PMID: 22514777. PMCID: PMC3324748.4. Ok SY, Ryoo SH, Baek YH, Kim SH, Kim SI, Kim SC, et al. Drip infusion method as a useful indicator for identification of the epidural space. Korean J Anesthesiol. 2009; 57:181–4. DOI: 10.4097/kjae.2009.57.2.181.5. Baek YH, Ok SY, Kim SI, Kim SC, Lee MH. Effects of continuous epidural infusion after thoracic epidural anesthesia for mastectomy on postoperative pain, nausea and vomiting. Korean J Anesthesiol. 2007; 52:396–402. DOI: 10.4097/kjae.2007.52.4.396.6. Singh AP, Tewari M, Singh DK, Shukla HS. Cervical epidural anesthesia: a safe alternative to general anesthesia for patients undergoing cancer breast surgery. World J Surg. 2006; 30:2043–7. DOI: 10.1007/s00268-006-0117-2. PMID: 16927058.7. Cha SM, Jung YH, Kim DS, Park JS, Kang H, Baek CW, et al. Distance from the lumbar epidural space to the skin in Korean adults. Anesth Pain Med. 2011; 6:16–20.8. Kao MC, Tsai SK, Chang WK, Liu HT, Hsieh YC, Hu JS, et al. Prediction of the distance from skin to epidural space for low-thoracic epidural catheter insertion by computed tomography. Br J Anaesth. 2004; 92:271–3. DOI: 10.1093/bja/aeh053. PMID: 14722181.9. Lee SJ, Choi SH, Kim MS, Shin YS. Prediction of the distance from skin to mid-thoracic epidural space by computed tomography. Korean J Anesthesiol. 2005; 48:605–8. DOI: 10.4097/kjae.2005.48.6.605.10. Kim SH, Lee KH, Yoon KB, Park WY, Yoon DM. Sonographic estimation of needle depth for cervical epidural blocks. Anesth Analg. 2008; 106:1542–7. DOI: 10.1213/ane.0b013e318168b6a8. PMID: 18420873.11. Rasoulian A, Lohser J, Najafi M, Rafii-Tari H, Tran D, Kamani AA, et al. Utility of prepuncture ultrasound for localization of the thoracic epidural space. Can J Anaesth. 2011; 58:815–23. DOI: 10.1007/s12630-011-9548-9. PMID: 21698508.12. Grau T, Leipold RW, Delorme S, Martin E, Motsch J. Ultrasound imaging of the thoracic epidural space. Reg Anesth Pain Med. 2002; 27:200–6. DOI: 10.1053/rapm.2002.29239. PMID: 11915069.13. Avramescu S, Arzola C, Tharmaratnam U, Chin KJ, Balki M. Sonoanatomy of the thoracic spine in adult volunteers. Reg Anesth Pain Med. 2012; 37:349–53. DOI: 10.1097/AAP.0b013e3182464be2. PMID: 22354105.14. Aldrete JA, Mushin AU, Zapata JC, Ghaly R. Skin to cervical epidural space distances as read from magnetic resonance imaging films: consideration of the “hump pad.”. J Clin Anesth. 1998; 10:309–13. DOI: 10.1016/S0952-8180(98)00033-6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Distance from Skin to Cervical Epidural Space
- A Clinical Measure of the Skin to Cervical Epidural Space Depth in the Korean Adults
- Distance from the Skin to the Cervical Epidural Space in Korean Adults
- To Study About Distance from Skin to Cervical Epidural Space in Korean Adults
- Surface Anatomical Landmark and Optimal Insertion Angle in Cervical Epidural Block