J Korean Soc Radiol.
2017 Feb;76(2):96-103. 10.3348/jksr.2017.76.2.96.
Detection of Breast Abnormalities on Enhanced Chest CT: Correlation with Breast Composition on Mammography
- Affiliations
-
- 1Department of Radiology, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea. soinvain@naver.com
- KMID: 2367856
- DOI: http://doi.org/10.3348/jksr.2017.76.2.96
Abstract
- PURPOSE
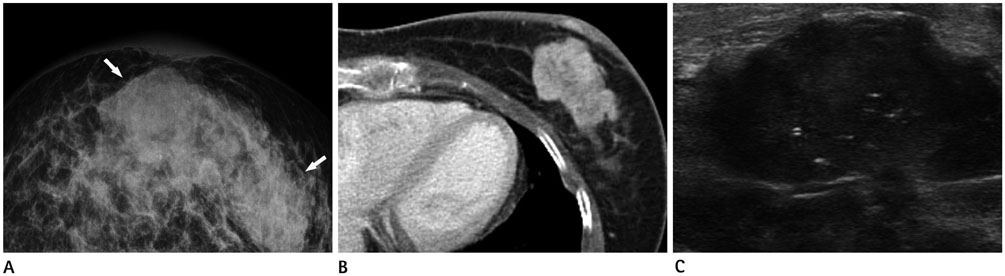
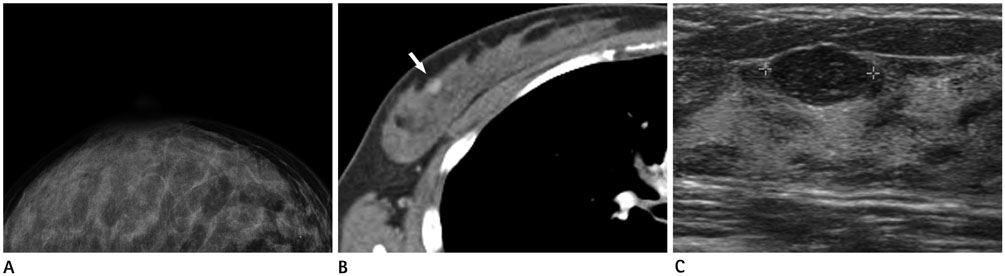
To investigate the capability of enhanced chest computed tomography (CT) for detecting breast abnormalities and to assess the influence of breast composition on this detectability.
MATERIALS AND METHODS
From 2000 to 2013, 75 patients who underwent mammography, breast sonography, and enhanced chest CT within one month and had abnormalities on sonography were included. Detection rate of breast abnormality on enhanced chest CT was compared among 4 types of breast composition by the Breast Imaging Reporting and Data System. Contribution of breast composition, size and enhancement of target lesions to detectability of enhanced chest CT was assessed using logistic regression and chi-square test.
RESULTS
Of the 75 target lesions, 34 (45.3%) were detected on enhanced chest CT, corresponding with those on breast sonography; there were no significantly different detection rates among the 4 types of breast composition (p = 0.078). Breast composition [odds ratio (OR) = 1.07, p = 0.206] and enhancement (OR = 21.49, p = 0.998) had no significant effect, but size (OR = 1.23, p = 0.004) was a significant contributing factor influencing the detectability of enhanced chest CT for breast lesions.
CONCLUSION
About half of the cases (45.3%) demonstrated breast lesions on chest CT corresponding with target lesions on sonography. Breast composition defined on mammography did not affect the detectability of enhanced chest CT for breast lesions.
MeSH Terms
Figure
Cited by 1 articles
-
Incidental Breast Lesions on Chest CT: Clinical Significance and Differential Features Requiring Referral
Yun Jung Choi, Tae Hoon Kim, Yoon Jin Cha, Eun Ju Son, Hye Mi Gweon, Chul Hwan Park
J Korean Soc Radiol. 2018;79(6):303-310. doi: 10.3348/jksr.2018.79.6.303.
Reference
-
1. Sickles EA, D'Orsi CJ, Bassett LW, Appleton CM, Berg WA, Burnside ES, et al. ACR BI-RADS-Mammography 2013. In : Reston VA, editor. ACR BI-RADS atlas breast imaging reporting and data system. 5th ed. American College of Radiology;2013. p. 123–126.2. Tamimi RM, Byrne C, Colditz GA, Hankinson SE. Endogenous hormone levels, mammographic density, and subsequent risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 2007; 99:1178–1187.3. Meller MT, Cox JE, Callanan KW. Incidental detection of breast lesions with computed tomography. Clin Breast Cancer. 2007; 7:634–637.4. Yi JG, Kim SJ, Marom EM, Park JH, Jung SI, Lee MW. Chest CT of incidental breast lesions. J Thorac Imaging. 2008; 23:148–155.5. Salvatore M, Margolies L, Kale M, Wisnivesky J, Kotkin S, Henschke CI, et al. Breast density: comparison of chest CT with mammography. Radiology. 2014; 270:67–73.6. Kolb TM, Lichy J, Newhouse JH. Comparison of the performance of screening mammography, physical examination, and breast US and evaluation of factors that influence them: an analysis of 27,825 patient evaluations. Radiology. 2002; 225:165–175.7. Kim JH, Chang YW, Hwang JH, Kim HH, Lee EH, Yang SB. Evaluation of the significance of incidental breast lesions detected by chest CT. J Korean Soc Radiol. 2013; 68:229–235.8. Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007; 356:227–236.9. Boyd NF, Martin LJ, Rommens JM, Paterson AD, Minkin S, Yaffe MJ, et al. Mammographic density: a heritable risk factor for breast cancer. Methods Mol Biol. 2009; 472:343–360.10. Cecchini RS, Costantino JP, Cauley JA, Cronin WM, Wickerham DL, Bandos H, et al. Baseline mammographic breast density and the risk of invasive breast cancer in postmenopausal women participating in the NSABP study of tamoxifen and raloxifene (STAR). Cancer Prev Res (Phila). 2012; 5:1321–1329.11. Hooley RJ, Greenberg KL, Stackhouse RM, Geisel JL, Butler RS, Philpotts LE. Screening US in patients with mammographically dense breasts: initial experience with Connecticut Public Act 09-41. Radiology. 2012; 265:59–69.12. Graf O, Helbich TH, Fuchsjaeger MH, Hopf G, Morgun M, Graf C, et al. Follow-up of palpable circumscribed noncalcified solid breast masses at mammography and US: can biopsy be averted? Radiology. 2004; 233:850–856.13. Mainiero MB, Goldkamp A, Lazarus E, Livingston L, Koelliker SL, Schepps B, et al. Characterization of breast masses with sonography: can biopsy of some solid masses be deferred? J Ultrasound Med. 2005; 24:161–167.14. Stavros AT, Thickman D, Rapp CL, Dennis MA, Parker SH, Sisney GA. Solid breast nodules: use of sonography to distinguish between benign and malignant lesions. Radiology. 1995; 196:123–134.15. Hong AS, Rosen EL, Soo MS, Baker JA. BI-RADS for sonography: positive and negative predictive values of sonographic features. AJR Am J Roentgenol. 2005; 184:1260–1265.16. Porter G, Steel J, Paisley K, Watkins R, Holgate C. Incidental breast masses detected by computed tomography: are any imaging features predictive of malignancy? Clin Radiol. 2009; 64:529–533.17. Moyle P, Sonoda L, Britton P, Sinnatamby R. Incidental breast lesions detected on CT: what is their significance. Br J Radiol. 2010; 83:233–240.18. Surov A, Fiedler E, Wienke A, Holzhausen HJ, Spielmann RP, Behrmann C. Intramammary incidental findings on staging computer tomography. Eur J Radiol. 2012; 81:2174–2178.19. Lin WC, Hsu HH, Li CS, Yu JC, Hsu GC, Yu CP, et al. Incidentally detected enhancing breast lesions on chest computed tomography. Korean J Radiol. 2011; 12:44–51.20. March DE, Wechsler RJ, Kurtz AB, Rosenberg AL, Needleman L. CT-pathologic correlation of axillary lymph nodes in breast carcinoma. J Comput Assist Tomogr. 1991; 15:440–444.21. Hata Y, Ogawa Y, Nishioka A, Inomata T, Yoshida S, Toki T. [Evaluation of thin section CT scanning in the prone position of metastatic axillary lymph nodes for breast cancer]. Nihon Igaku Hoshasen Gakkai Zasshi. 1996; 56:1027–1031.22. Prionas ND, Lindfors KK, Ray S, Huang SY, Beckett LA, Monsky WL, et al. Contrast-enhanced dedicated breast CT: initial clinical experience. Radiology. 2010; 256:714–723.