J Korean Med Sci.
2017 Mar;32(3):528-533. 10.3346/jkms.2017.32.3.528.
Who Dies after ICU Discharge? Retrospective Analysis of Prognostic Factors for In-Hospital Mortality of ICU Survivors
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. yeonjoolee1117@gmail.com
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2366652
- DOI: http://doi.org/10.3346/jkms.2017.32.3.528
Abstract
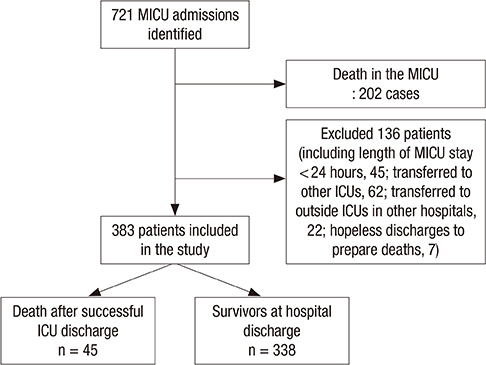
- We investigated the causes of inpatient death after intensive care unit (ICU) discharge and determined predictors of in-hospital mortality in Korea. Using medical ICU registry data of Seoul National University Hospital, we performed a retrospective cohort study involving patients who were discharged alive from their first ICU admission with at least 24 hours of ICU length of stay (LOS). From January 2011 to August 2013, 723 patients were admitted to ICU and 383 patients were included. The estimated in-hospital mortality rate was 11.7% (45/383). The most common cause of death was respiratory failure (n = 25, 56%) followed by sepsis and cancer progression; the causes of hospital death and ICU admission were the same in 64% of all deaths; sudden unexpected deaths comprised about one-fifth of all deaths. In order to predict in-hospital mortality among ICU survivors, multivariate analysis identified presence of solid tumor (odds ratio [OR], 4.06; 95% confidence interval [CI], 2.01-8.2; P < 0.001), hematologic disease (OR, 4.75; 95% CI, 1.51-14.96; P = 0.013), Sequential Organ Failure Assessment (SOFA) score upon ICU admission (OR, 1.08; 95% CI, 0.99-1.17; P = 0.075), and hemoglobin (Hb) level (OR, 0.67; 95% CI, 0.52-0.86; P = 0.001) and platelet count (Plt) (OR, 0.99; 95% CI, 0.99-1.00; P = 0.033) upon ICU discharge as significant factors. In conclusion, a significant proportion of in-hospital mortality is predictable and those who die in hospital after ICU discharge tend to be severely-ill, with comorbidities of hematologic disease and solid tumor, and anemic and thrombocytopenic upon ICU discharge.
MeSH Terms
Figure
Reference
-
1. Goldhill DR, Sumner A. Outcome of intensive care patients in a group of British intensive care units. Crit Care Med. 1998; 26:1337–1345.2. Rowan KM, Kerr JH, Major E, McPherson K, Short A, Vessey MP. Intensive Care Society’s APACHE II study in Britain and Ireland--II: outcome comparisons of intensive care units after adjustment for case mix by the American APACHE II method. BMJ. 1993; 307:977–981.3. Smith L, Orts CM, O’Neil I, Batchelor AM, Gascoigne AD, Baudouin SV. TISS and mortality after discharge from intensive care. Intensive Care Med. 1999; 25:1061–1065.4. Azoulay E, Adrie C, De Lassence A, Pochard F, Moreau D, Thiery G, Cheval C, Moine P, Garrouste-Orgeas M, Alberti C, et al. Determinants of postintensive care unit mortality: a prospective multicenter study. Crit Care Med. 2003; 31:428–432.5. Ranzani OT, Prada LF, Zampieri FG, Battaini LC, Pinaffi JV, Setogute YC, Salluh JI, Povoa P, Forte DN, Azevedo LC, et al. Failure to reduce C-reactive protein levels more than 25% in the last 24 hours before intensive care unit discharge predicts higher in-hospital mortality: a cohort study. J Crit Care. 2012; 27:525.e9–525.15.6. Daly K, Beale R, Chang RW. Reduction in mortality after inappropriate early discharge from intensive care unit: logistic regression triage model. BMJ. 2001; 322:1274–1276.7. Sprung CL, Danis M, Iapichino G, Artigas A, Kesecioglu J, Moreno R, Lippert A, Curtis JR, Meale P, Cohen SL, et al. Triage of intensive care patients: identifying agreement and controversy. Intensive Care Med. 2013; 39:1916–1924.8. Brown SE, Ratcliffe SJ, Halpern SD. Assessing the utility of ICU readmissions as a quality metric: an analysis of changes mediated by residency work-hour reforms. Chest. 2015; 147:626–636.9. Wagner J, Gabler NB, Ratcliffe SJ, Brown SE, Strom BL, Halpern SD. Outcomes among patients discharged from busy intensive care units. Ann Intern Med. 2013; 159:447–455.10. Moreno R, Agthé D. ICU discharge decision-making: are we able to decrease post-ICU mortality? Intensive Care Med. 1999; 25:1035–1036.11. Casaer MP, Ziegler TR. Nutritional support in critical illness and recovery. Lancet Diabetes Endocrinol. 2015; 3:734–745.12. Goldhill DR, Worthington L, Mulcahy A, Tarling M, Sumner A. The patient-at-risk team: identifying and managing seriously ill ward patients. Anaesthesia. 1999; 54:853–860.13. Santamaria JD, Duke GJ, Pilcher DV, Cooper DJ, Moran J, Bellomo R; Discharge and Readmission Evaluation (DARE) Study. The timing of discharge from the intensive care unit and subsequent mortality. A prospective, multicenter study. Am J Respir Crit Care Med. 2015; 191:1033–1039.14. Azoulay E, Alberti C, Legendre I, Buisson CB, Le Gall JR; European Sepsis Group. Post-ICU mortality in critically ill infected patients: an international study. Intensive Care Med. 2005; 31:56–63.15. Martin-Loeches I, Wunderink RG, Nanchal R, Lefrant JY, Kapadia F, Sakr Y, Vincent JL. ICON Investigators. Determinants of time to death in hospital in critically ill patients around the world. Intensive Care Med. 2016; 42:1454–1460.16. Bion J. Rationing intensive care. BMJ. 1995; 310:682–683.17. Jeong BH, Ko MG, Nam J, Yoo H, Chung CR, Suh GY, Jeon K. Differences in clinical outcomes according to weaning classifications in medical intensive care units. PLoS One. 2015; 10:e0122810.18. Parsons EC, Hough CL, Seymour CW, Cooke CR, Rubenfeld GD, Watkins TR; NHLBI ARDS Network. Red blood cell transfusion and outcomes in patients with acute lung injury, sepsis and shock. Crit Care. 2011; 15:R221.19. Lim SY, Jeon EJ, Kim HJ, Jeon K, Um SW, Koh WJ, Chung MP, Kim H, Kwon OJ, Suh GY. The incidence, causes, and prognostic significance of new-onset thrombocytopenia in intensive care units: a prospective cohort study in a Korean hospital. J Korean Med Sci. 2012; 27:1418–1423.20. Zhang Z, Xu X, Ni H, Deng H. Platelet indices are novel predictors of hospital mortality in intensive care unit patients. J Crit Care. 2014; 29:885.e1–885.e6.21. van Zyl N, Reade MC, Fraser JF. Experimental animal models of traumatic coagulopathy: a systematic review. Shock. 2015; 44:16–24.22. Johansson PI, Haase N, Perner A, Ostrowski SR. Association between sympathoadrenal activation, fibrinolysis, and endothelial damage in septic patients: a prospective study. J Crit Care. 2014; 29:327–333.23. Levi M, Schultz M. Coagulopathy and platelet disorders in critically ill patients. Minerva Anestesiol. 2010; 76:851–859.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk factors for hospital mortality in intensive care unit survivors: a retrospective cohort study
- Clinical Features and Risk Factors of Patients Readmitted to ICU
- The Effect of Discharge Decision-Making of the Intensivist on Readmission to the Intensive Care Unit
- A Study About the Factors Concerned with Death of ICU patients by the APACHE III tool
- Impact of Environmental Stressors on the Risk for Posttraumatic Stress Disorder and Quality of Life in Intensive Care Unit Survivors