J Korean Med Sci.
2017 Mar;32(3):421-426. 10.3346/jkms.2017.32.3.421.
Risk Factors for Metachronous Recurrence after Endoscopic Submucosal Dissection of Early Gastric Cancer
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Gachon University, Gil Medical Center, Incheon, Korea. drgreen@gilhospital.com
- 2Division of Gastroenterology, Department of Internal Medicine, Catholic Kwandong University International St. Mary's Hospital, Incheon, Korea.
- KMID: 2366637
- DOI: http://doi.org/10.3346/jkms.2017.32.3.421
Abstract
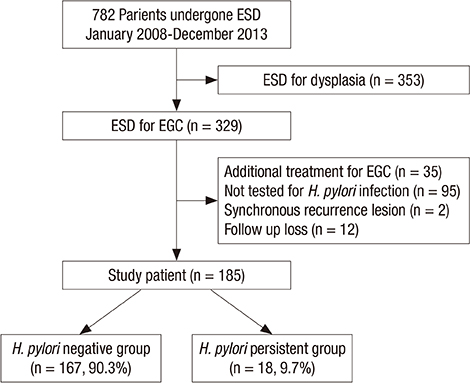
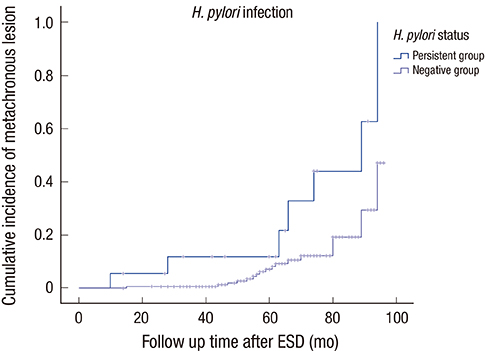
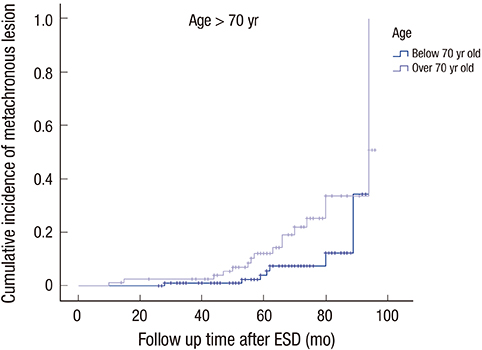
- Although endoscopic submucosal dissection (ESD) is widely accepted as a curative treatment method for early gastric cancer (EGC) worldwide, metachronous recurrence often occurs after ESD for EGC. However, there are insufficient data about the role of Helicobacter pylori (H. pylori) infection and other risk factors for recurrence. We aimed to compare the metachronous lesion in the H. pylori persistent group and the eradicated group, and to identify risk factors for metachronous lesion. We retrospectively analyzed 782 patients who underwent ESD between January 2008 and December 2013. We excluded patients with dysplasia or patients who were not tested for H. pylori infection. One hundred eighty-five patients were enrolled. We studied risk factors for recurrence, and used survival analysis to test. There were 24 patients with metachronous recurrence after ESD for EGC among the group. The incidence of metachronous gastric lesions after ESD for EGC developed more in the over 70-year-old group (P = 0.025) and more in the H. pylori persistent group (P = 0.008). In conclusion, H. pylori infection and old age are independent risk factors for metachronous gastric lesions after ESD in EGC.
MeSH Terms
Figure
Reference
-
1. Tan VP, Wong BC. Gastric cancer chemoprevention: the current evidence. Gastroenterol Clin North Am. 2013; 42:299–316.2. Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011; 61:212–236.3. Marshall BJ, Warren JR. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984; 1:1311–1315.4. Marshall BJ, Armstrong JA, McGechie DB, Glancy RJ. Attempt to fulfil Koch’s postulates for pyloric Campylobacter. Med J Aust. 1985; 142:436–439.5. Schistosomes, liver flukes and Helicobacter pylori. IARC Working Group on the evaluation of carcinogenic risks to humans. Lyon, 7-14 June 1994. IARC Monogr Eval Carcinog Risks Hum. 1994; 61:1–241.6. Huang JQ, Sridhar S, Chen Y, Hunt RH. Meta-analysis of the relationship between Helicobacter pylori seropositivity and gastric cancer. Gastroenterology. 1998; 114:1169–1179.7. Choi MK, Kim GH, Park DY, Song GA, Kim DU, Ryu DY, Lee BE, Cheong JH, Cho M. Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: a single-center experience. Surg Endosc. 2013; 27:4250–4258.8. Kim SG. Endoscopic treatment for early gastric cancer. J Gastric Cancer. 2011; 11:146–154.9. Nakagawa S, Asaka M, Kato M, Nakamura T, Kato C, Fujioka T, Tatsuta M, Keida K, Terao S, Takahashi S, et al. Helicobacter pylori eradication and metachronous gastric cancer after endoscopic mucosal resection of early gastric cancer. Aliment Pharmacol Ther. 2006; 24:214–218.10. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123.11. Shin SH. Jung da H, Kim JH, Chung HS, Park JC, Shin SK, Lee SK, Lee YC. Helicobacter pylori eradication prevents metachronous gastric neoplasms after endoscopic resection of gastric dysplasia. PLoS One. 2015; 10:e0143257.12. Bae SE, Jung HY, Kang J, Park YS, Baek S, Jung JH, Choi JY, Kim MY, Ahn JY, Choi KS, et al. Effect of Helicobacter pylori eradication on metachronous recurrence after endoscopic resection of gastric neoplasm. Am J Gastroenterol. 2014; 109:60–67.13. Kim YI, Choi IJ, Kook MC, Cho SJ, Lee JY, Kim CG, Ryu KW, Kim YW. The association between Helicobacter pylori status and incidence of metachronous gastric cancer after endoscopic resection of early gastric cancer. Helicobacter. 2014; 19:194–201.14. Maehata Y, Nakamura S, Fujisawa K, Esaki M, Moriyama T, Asano K, Fuyuno Y, Yamaguchi K, Egashira I, Kim H, et al. Long-term effect of Helicobacter pylori eradication on the development of metachronous gastric cancer after endoscopic resection of early gastric cancer. Gastrointest Endosc. 2012; 75:39–46.15. Choi J, Kim SG, Yoon H, Im JP, Kim JS, Kim WH, Jung HC. Eradication of Helicobacter pylori after endoscopic resection of gastric tumors does not reduce incidence of metachronous gastric carcinoma. Clin Gastroenterol Hepatol. 2014; 12:793–800.e1.16. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112.17. Kim SG, Jung HK, Lee HL, Jang JY, Lee H, Kim CG, Shin WG, Shin ES, Lee YC;. Guidelines for the diagnosis and treatment of Helicobacter pylori infection in Korea, 2013 revised edition. Korean J Gastroenterol. 2013; 62:3–26.18. Chung JW, Jung HY, Choi KD, Song HJ, Lee GH, Jang SJ, Park YS, Yook JH, Oh ST, Kim BS, et al. Extended indication of endoscopic resection for mucosal early gastric cancer: analysis of a single center experience. J Gastroenterol Hepatol. 2011; 26:884–887.19. Kosaka T, Endo M, Toya Y, Abiko Y, Kudara N, Inomata M, Chiba T, Takikawa Y, Suzuki K, Sugai T. Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: a single-center retrospective study. Dig Endosc. 2014; 26:183–191.20. Tanabe S, Ishido K, Higuchi K, Sasaki T, Katada C, Azuma M, Naruke A, Kim M, Koizumi W. Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: a retrospective comparison with conventional endoscopic resection in a single center. Gastric Cancer. 2014; 17:130–136.21. Oda I, Oyama T, Abe S, Ohnita K, Kosaka T, Hirasawa K, Ishido K, Nakagawa M, Takahashi S. Preliminary results of multicenter questionnaire study on long-term outcomes of curative endoscopic submucosal dissection for early gastric cancer. Dig Endosc. 2014; 26:214–219.22. Kim JH, Lee JH, Chung JW, An J, Won IS, Lee JW, Ha M, Kim JS, Ahn HD, Park JC, et al. Risk factors for local recurrence of early gastric cancer after endoscopic submucosal dissection. Korean J Med. 2013; 85:285–293.23. Abe S, Oda I, Suzuki H, Nonaka S, Yoshinaga S, Nakajima T, Sekiguchi M, Mori G, Taniguchi H, Sekine S, et al. Long-term surveillance and treatment outcomes of metachronous gastric cancer occurring after curative endoscopic submucosal dissection. Endoscopy. 2015; 47:1113–1118.24. Hosokawa O, Kaizaki Y, Watanabe K, Hattori M, Douden K, Hayashi H, Maeda S. Endoscopic surveillance for gastric remnant cancer after early cancer surgery. Endoscopy. 2002; 34:469–473.25. Choi KS, Jung HY, Choi KD, Lee GH, Song HJ, Kim DH, Lee JH, Kim MY, Kim BS, Oh ST, et al. EMR versus gastrectomy for intramucosal gastric cancer: comparison of long-term outcomes. Gastrointest Endosc. 2011; 73:942–948.26. Etoh T, Katai H, Fukagawa T, Sano T, Oda I, Gotoda T, Yoshimura K, Sasako M. Treatment of early gastric cancer in the elderly patient: results of EMR and gastrectomy at a national referral center in Japan. Gastrointest Endosc. 2005; 62:868–871.27. Hansson LE, Nyrén O, Hsing AW, Bergström R, Josefsson S, Chow WH, Fraumeni JF Jr, Adami HO. The risk of stomach cancer in patients with gastric or duodenal ulcer disease. N Engl J Med. 1996; 335:242–249.28. Uemura N, Okamoto S, Yamamoto S, Matsumura N, Yamaguchi S, Yamakido M, Taniyama K, Sasaki N, Schlemper RJ. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2001; 345:784–789.29. Hojo M, Miwa H, Ohkusa T, Ohkura R, Kurosawa A, Sato N. Alteration of histological gastritis after cure of Helicobacter pylori infection. Aliment Pharmacol Ther. 2002; 16:1923–1932.30. Ley C, Mohar A, Guarner J, Herrera-Goepfert R, Figueroa LS, Halperin D, Johnstone I, Parsonnet J. Helicobacter pylori eradication and gastric preneoplastic conditions: a randomized, double-blind, placebo-controlled trial. Cancer Epidemiol Biomarkers Prev. 2004; 13:4–10.31. Wong BC, Lam SK, Wong WM, Chen JS, Zheng TT, Feng RE, Lai KC, Hu WH, Yuen ST, Leung SY, et al. Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trial. JAMA. 2004; 291:187–194.32. Chung JW, Hahm KB. Rejuvenation of atrophic gastritis in the elderly. J Gastroenterol Hepatol. 2010; 25:434–435.33. Wu CY, Kuo KN, Wu MS, Chen YJ, Wang CB, Lin JT. Early Helicobacter pylori eradication decreases risk of gastric cancer in patients with peptic ulcer disease. Gastroenterology. 2009; 137:1641–1648.e1-2.34. Lee YC, Chiang TH, Chou CK, Tu YK, Liao WC, Wu MS, Graham DY. Association between Helicobacter pylori eradication and gastric cancer incidence: a systematic review and meta-analysis. Gastroenterology. 2016; 150:1113–1124.e5.35. Asaka M, Kato M, Graham DY. Prevention of gastric cancer by Helicobacter pylori eradication. Intern Med. 2010; 49:633–636.36. Kushi LH, Byers T, Doyle C, Bandera EV, McCullough M, McTiernan A, Gansler T, Andrews KS, Thun MJ; American Cancer Society 2006 Nutrition and Physical Activity Guidelines Advisory Committee. American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2006; 56:254–281.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors for Metachronous Recurrence after Endoscopic Submucosal Dissection of a Gastric Neoplasm
- A Case of Metachronous Gastric Cancer and Follicular Lymphoma after Endoscopic Submucosal Dissection for Early Gastric Cancer
- The pattern of metachronous recurrence after endoscopic submucosal dissection for gastric adenocarcinoma and dysplasias
- Endoscopic Submucosal Dissection Followed by Concurrent Chemoradiotherapy in Patients with Early Esophageal Cancer with a High Risk of Lymph Node Metastasis
- Endoscopic resection for early gastric cancer: The current controversies