J Korean Neurosurg Soc.
2017 Jan;60(1):30-39. 10.3340/jkns.2015.0506.004.
Comparative Analysis between Total Disc Replacement and Posterior Foraminotomy for Posterolateral Soft Disc Herniation with Unilateral Radiculopathy : Clinical and Biomechanical Results of a Minimum 5 Years Follow-up
- Affiliations
-
- 1Department of Neurosurgery, Kyungpook National University Hospital, Daegu, Korea. nskimkt7@gmail.com
- 2Department of Neurosurgery, Chung-Ang University Hospital, Seoul, Korea.
- 3Department of Rehabilitation Medicine, Keimyung University Hospital, Daegu, Korea.
- KMID: 2365584
- DOI: http://doi.org/10.3340/jkns.2015.0506.004
Abstract
OBJECTIVE
To compare the clinical outcomes and biomechanical effects of total disc replacement (TDR) and posterior cervical foraminotomy (PCF) and to propose relative inclusion criteria.
METHODS
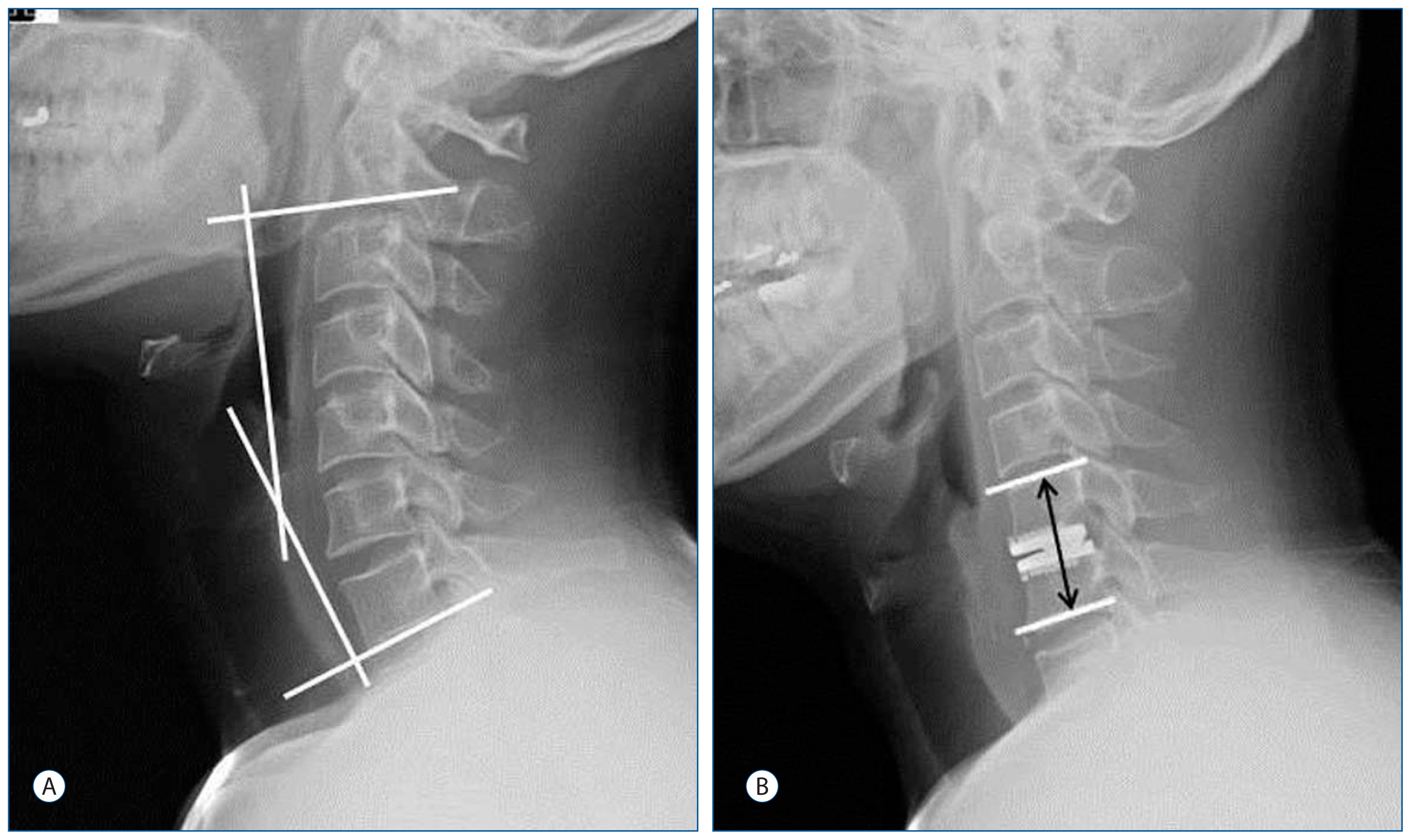
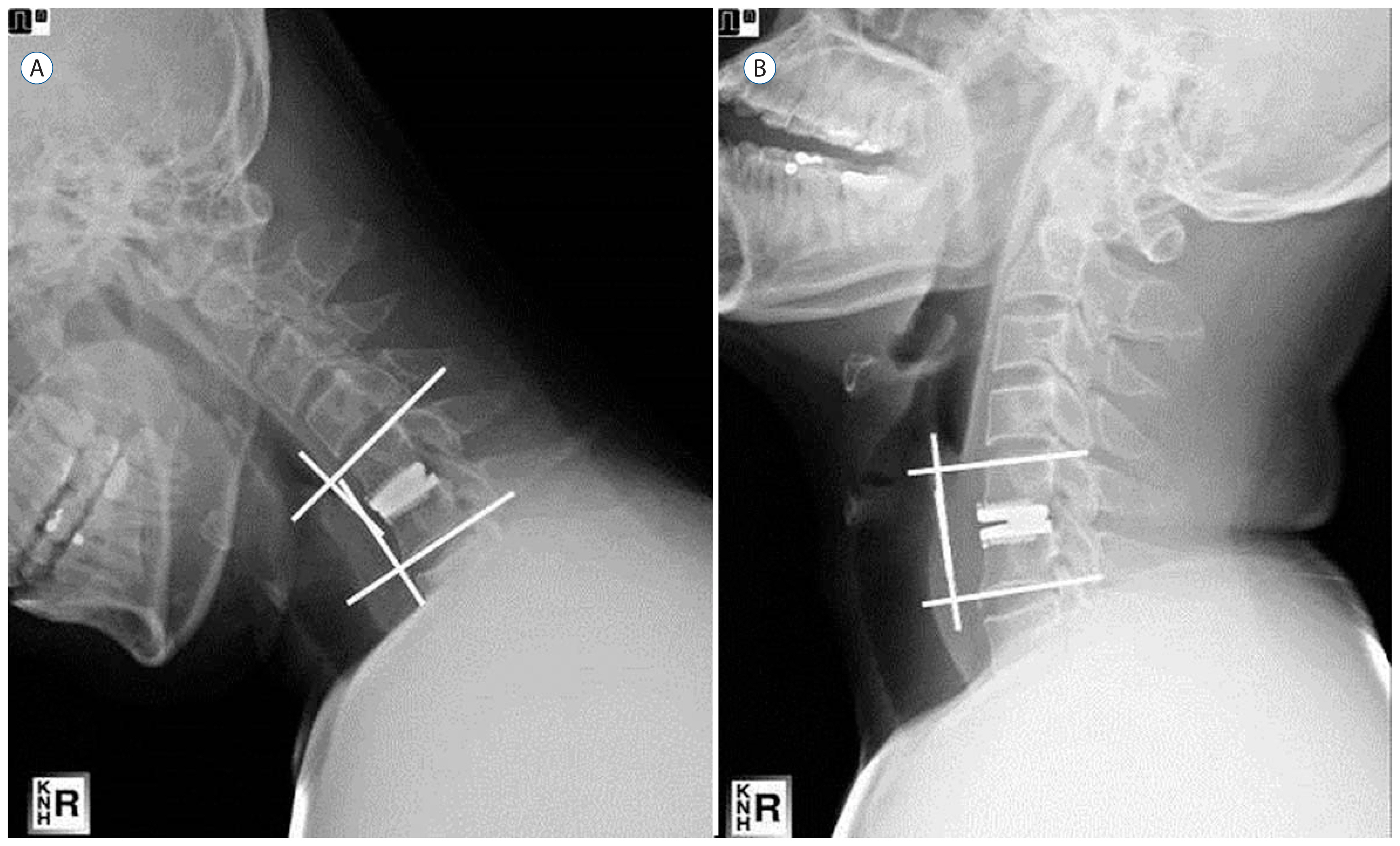
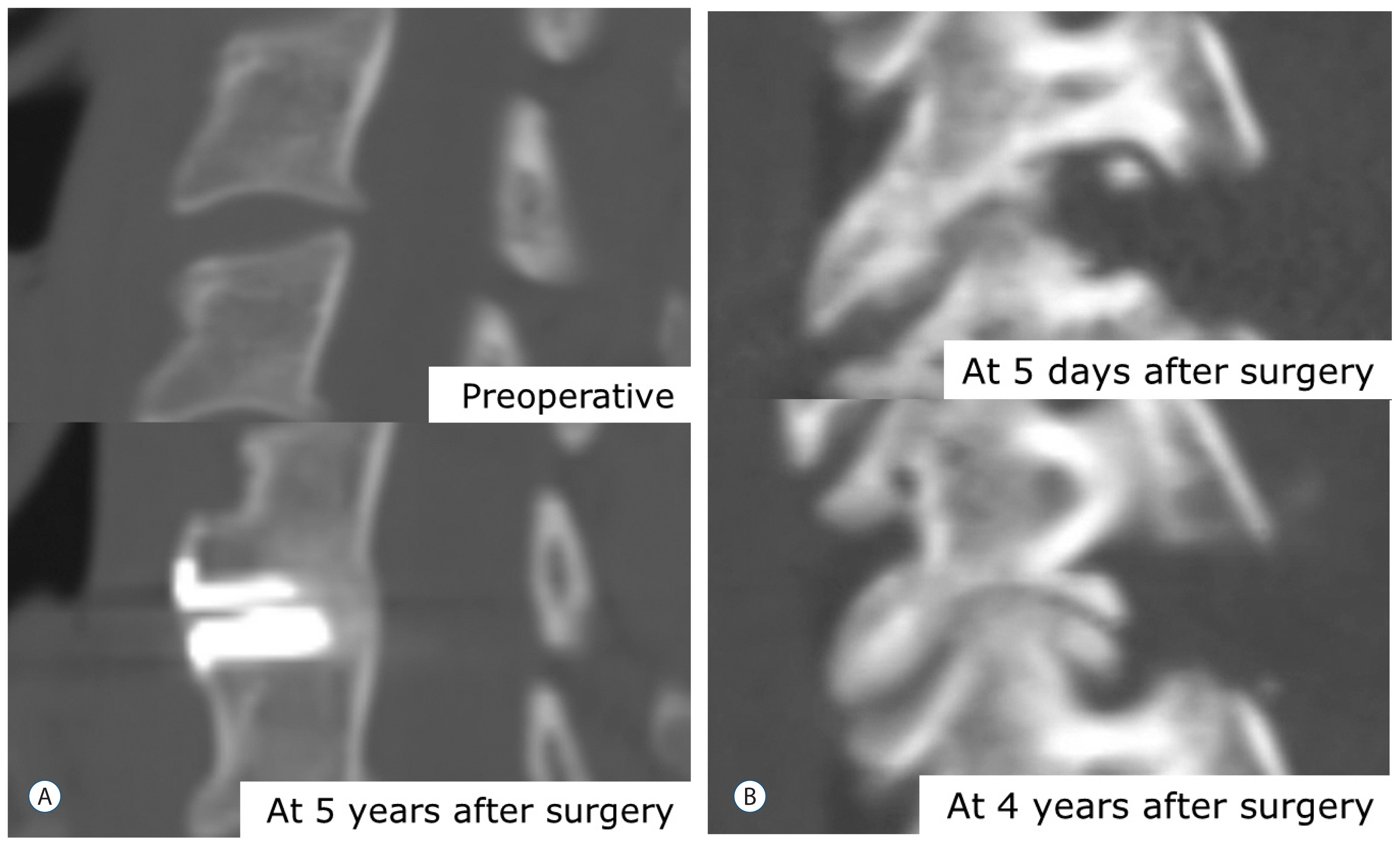
Thirty-five patients who underwent surgery between 2006 and 2008 were included. All patients had single-level disease and only radiculopathy. The overall sagittal balance and angle and height of a functional segmental unit (FSU; upper and lower vertebral body of the operative lesion) were assessed by preoperative and follow-up radiographs. C2-7 range of motion (ROM), FSU, and the adjacent segment were also checked.
RESULTS
The clinical outcome of TDR (group A) was tended to be superior to that of PCF (group B) without statistical significance. In the group A, preoperative and postoperative upper adjacent segment level motion values were 8.6±2.3 and 8.4±2.0, and lower level motion values were 8.4±2.2 and 8.3±1.9. Preoperative and postoperative FSU heights were 37.0±2.1 and 37.1±1.8. In the group B, upper level adjacent segment motion values were 8.1±2.6 and 8.2±2.8, and lower level motion values were 6.5±3.3 and 6.3±3.1. FSU heights were 37.1±2.0 and 36.2±1.8. The postoperative FSU motion and height changes were significant (p<0.05). The patient's satisfaction rates for surgery were 88.2% in group A and 88.8% in group B.
CONCLUSION
TDR and PCF have favorable outcomes in patients with unilateral soft disc herniation. However, patients have different biomechanical backgrounds, so the patient's biomechanical characteristics and economic status should be understood and treated using the optimal procedure.
MeSH Terms
Figure
Cited by 1 articles
-
Feasibility of Posterior Cervical Foraminotomy for Adjacent Segmental Disease after Anterior Cervical Fusion
Hyun Jun Kim, Min Soo Kang, Sang Ho Lee, Chan Hong Park, Seok Won Chung, Yong Hwan Shin, Shin Young Lee, Eun Soo Park
J Korean Neurosurg Soc. 2020;63(6):767-776. doi: 10.3340/jkns.2020.0033.
Reference
-
References
1. Aldrich F. Posterolateral microdisectomy for cervical monoradiculopathy caused by posterolateral soft cervical disc sequestration. J Neurosurg. 72:370–377. 1990.
Article2. Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine (Phila Pa 1976). 27:2453–2458. 2002.3. Beaurain J, Bernard P, Dufour T, Fuentes JM, Hovorka I, Huppert J, et al. Intermediate clinical and radiological results of cervical TDR (Mobi-C) with up to 2 years of follow-up. Eur Spine J. 18:841–850. 2009.
Article4. Cağlar YS, Bozkurt M, Kahilogullari G, Tuna H, Bakir A, Torun F, et al. Keyhole approach for posterior cervical discectomy: experience on 84 patients. Minim Invasive Neurosurg. 50:7–11. 2007.
Article5. Cho HJ, Shin MH, Huh JW, Ryu KS, Park CK. Heterotopic ossification following cervical total disc replacement: iatrogenic or constitutional? Korean J Spine. 9:209–214. 2012.
Article6. Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 15:602–617. 1958.
Article7. Ducker TB, Zeidman SM. The posterior operative approach for cervical radiculopathy. Neurosurg Clin N Am. 4:61–74. 1993.
Article8. Duggal N, Pickett GE, Mitsis DK, Keller JL. Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus. 17:E9. 2004.
Article9. Fehlings MG, Gray RJ. Posterior cervical foraminotomy for the treatment of cervical radiculopathy. J Neurosurg Spine. 10:343–344. 2009.
Article10. Gala VC, O’Toole JE, Voyadzis JM, Fessler RG. Posterior minimally invasive approaches for the cervical spine. Orthop Clin North Am. 38:339–349. 2007.
Article11. Henderson CM, Hennessy RG, Henry M Jr, Shackelford GE. Posterior-lateral foraminotomy as an exclusive operative technique for cervical radiculopathy: a review of 846 consecutively operated cases. Neurosurgery. 13:504–512. 1983.
Article12. Hilton DL Jr. Minimally invasive tubular access for posterior cervical foraminotomy with three-dimensional microscopic visualization and localization with anterior/posterior imaging. Spine J. 7:154–158. 2007.
Article13. Hrabálek L, Vaverka M, Houdek M. Cervical disc arthroplasty (Prodisc-C): analysis of 3 to 4- year follow up results. Rozhl Chir. 88:634–641. 2009.14. Jagannathan J, Sherman JH, Szabo T, Shaffrey CI, Jane JA. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease: a single-surgeon experience with a minimum of 5 years’ clinical and radiographic follow-up. J Neurosurg Spine. 10:347–356. 2009.
Article15. Jin YJ, Park SB, Kim MJ, Kim KJ, Kim HJ. An analysis of heterotopic ossification in cervical disc arthroplasty: a novel morphologic classification of an ossified mass. Spine J. 13:408–420. 2013.
Article16. Jödicke A, Daentzer D, Kästner S, Asamoto S, Böker DK. Risk factors for outcome and complications of dorsal foraminotomy in cervical disc herniation. Surg Neurol. 60:124–129. discussion 129–130. 2003.
Article17. Kang SH, Kim DK, Seo KM, Kim KT, Kim YB. Multi-level spinal fusion and postoperative prevertebral thickness increase the risk of dysphagia after anterior cervical spine surgery. J Clin Neurosci. 18:1369–1373. 2011.
Article18. Kim KT, Kim YB. Comparison between open procedure and tubular retractor assisted procedure for cervical radiculopathy: results of a randomized controlled study. J Korean Med Sci. 24:649–653. 2009.
Article19. Korinth MC, Krüger A, Oertel MF, Gilsbach JM. Posterior foraminotomy or anterior discectomy with polymethyl methacrylate interbody stabilization for cervical soft disc disease: results in 292 patients with monoradiculopathy. Spine (Phila Pa 1976). 31:1207–1214. 2006.
Article20. Leung C, Casey AT, Goffin J, Kehr P, Liebig K, Lind B, et al. Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery. 57:759–763. 2005.
Article21. Lidar Z, Salame K. Minimally invasive posterior cervical discectomy for cervical radiculopathy: technique and clinical results. J Spinal Disord Tech. 24:521–524. 2011.
Article22. McAfee PC, Cunningham BW, Devine J, Williams E, Yu-Yahiro J. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech. 16:384–389. 2003.
Article23. Morpeth JF, Williams MF. Vocal fold paresis after anterior cervical discectomy and fusion. Laryngoscope. 110:43–46. 2000.24. Park CK, Ryu KS, Lee KY, Lee HJ. Clinical outcome of lumbar total disc replacement using ProDisc-L in degenerative disc disease: minimum 5-year follow-up results at a single institute. Spine (Phila Pa 1976). 37:672–677. 2012.
Article25. Peng CW, Yue WM, Basit A, Guo CM, Tow BP, Chen JL, et al. Intermediate results of the prestige LP cervical disc replacement: clinical and radiological analysis with minimum two-year follow-up. Spine (Phila Pa 1976). 36:E105–111. 2011.26. Quan GM, Vital JM, Hansen S, Pointillart V. Eight-year clinical and radiological follow-up of the Bryan cervical disc arthroplasty. Spine (Phila Pa 1976). 36:639–646. 2011.
Article27. Rodrigues MA, Hanel RA, Prevedello DM, Antoniuk A, Araújo JC. Posterior approach for soft cervical disc herniation: a neglected technique? Surg Neurol. 55:17–22. discussion 22. 2001.
Article28. Roh SW, Kim DH, Cardoso AC, Fessler RG. Endoscopic foraminotomy using MED system in cadaveric specimens. Spine (Phila Pa 1976). 25:260–264. 2000.
Article29. Russell SM, Benjamin V. Posterior surgical approach to the cervical neural foramen for intervertebral disc disease. Neurosurgery. 54:662–665. 2004.
Article30. Ryu KS, Park CK, Jun SC, Huh HY. Radiological changes of the operated and adjacent segments following cervical arthroplasty after a minimum 24-month follow-up: comparison between the Bryan and Prodisc-C devices. J Neurosurg Spine. 13:299–307. 2010.
Article31. Stewart M, Johnston RA, Stewart I, Wilson JA. Swallowing performance following anterior cervical spine surgery. Br J Neurosurg. 9:605–609. 1995.
Article32. Yang CW, Fuh JL. C5 palsy after cervical spine decompression surgery. J Chin Med Assoc. 76:363–364. 2013.
Article33. Yi S, Lim JH, Choi KS, Sheen YC, Park HK, Jang IT. Comparison of anterior cervical foraminotomy vs arthroplasty for unilateral cervical radiculopathy. Surg Neurol. 71:677–680. discussion 680. 2009.
Article34. Yi S, Shin DA, Kim KN, Choi G, Shin HC, Kim KS, et al. The predisposing factors for the heterotopic ossification after cervical artificial disc replacement. Spine J. 13:1048–1054. 2013.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Result of Posterior Microforaminotomy for Posterolateral Herniation of Cervical Discs
- Management of a Rare Case of C2–3 Cervical Foraminal Disc Herniation by Unilateral Biportal Endoscopic Foraminotomy
- Endoscope Assisted Anterior Cervical Foraminotomy
- Relative Risk of Operation between Lumbar Far Lateral Disc Herniation and Posterolateral Disc Herniation: A Retrospective Cohort Study
- Brown Sequard Syndrome Resulting from Cervical Disc Herniation Treated by Anterior Foraminotomy