J Korean Neurosurg Soc.
2017 Jan;60(1):8-14. 10.3340/jkns.2016.0707.004.
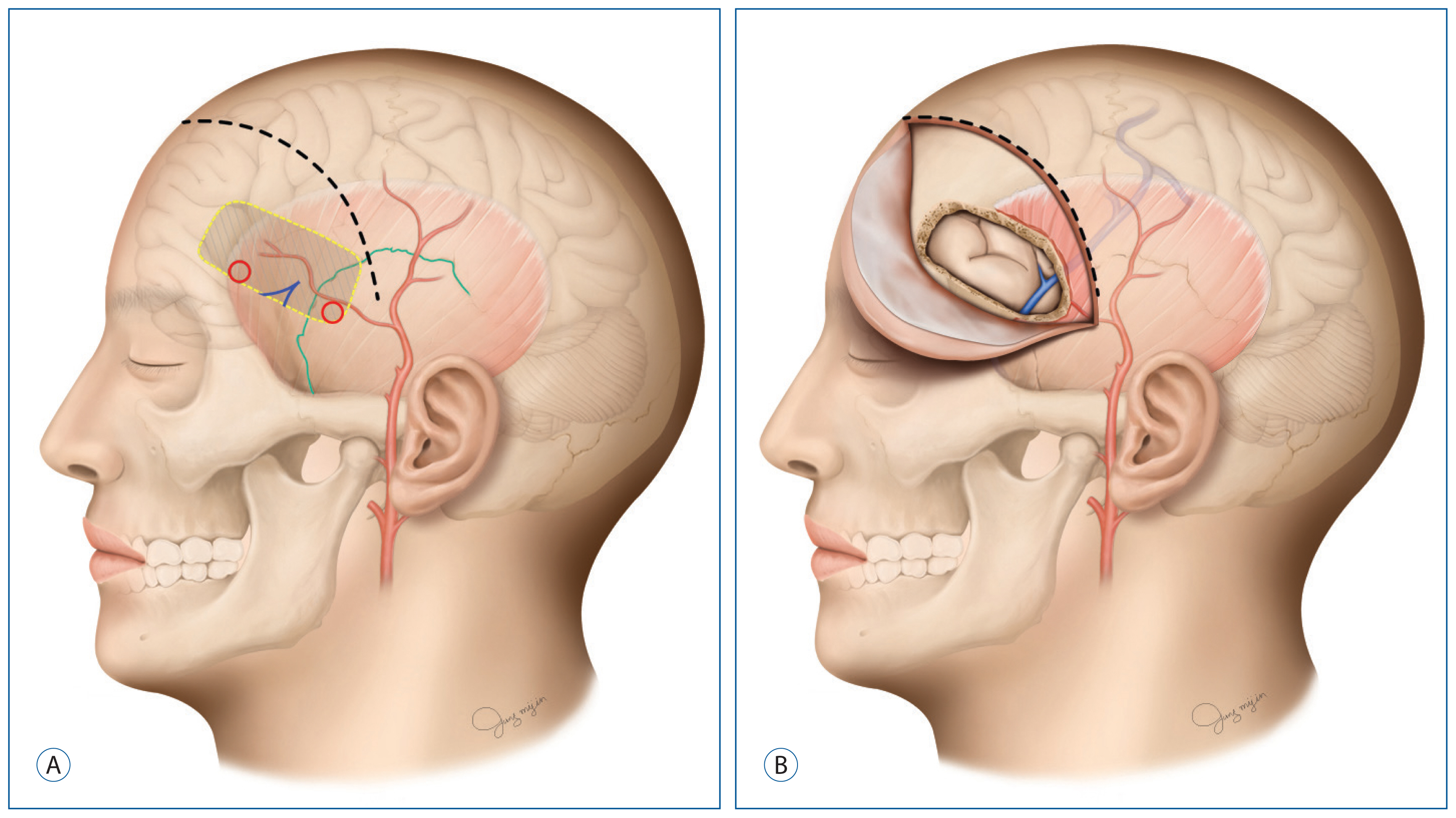
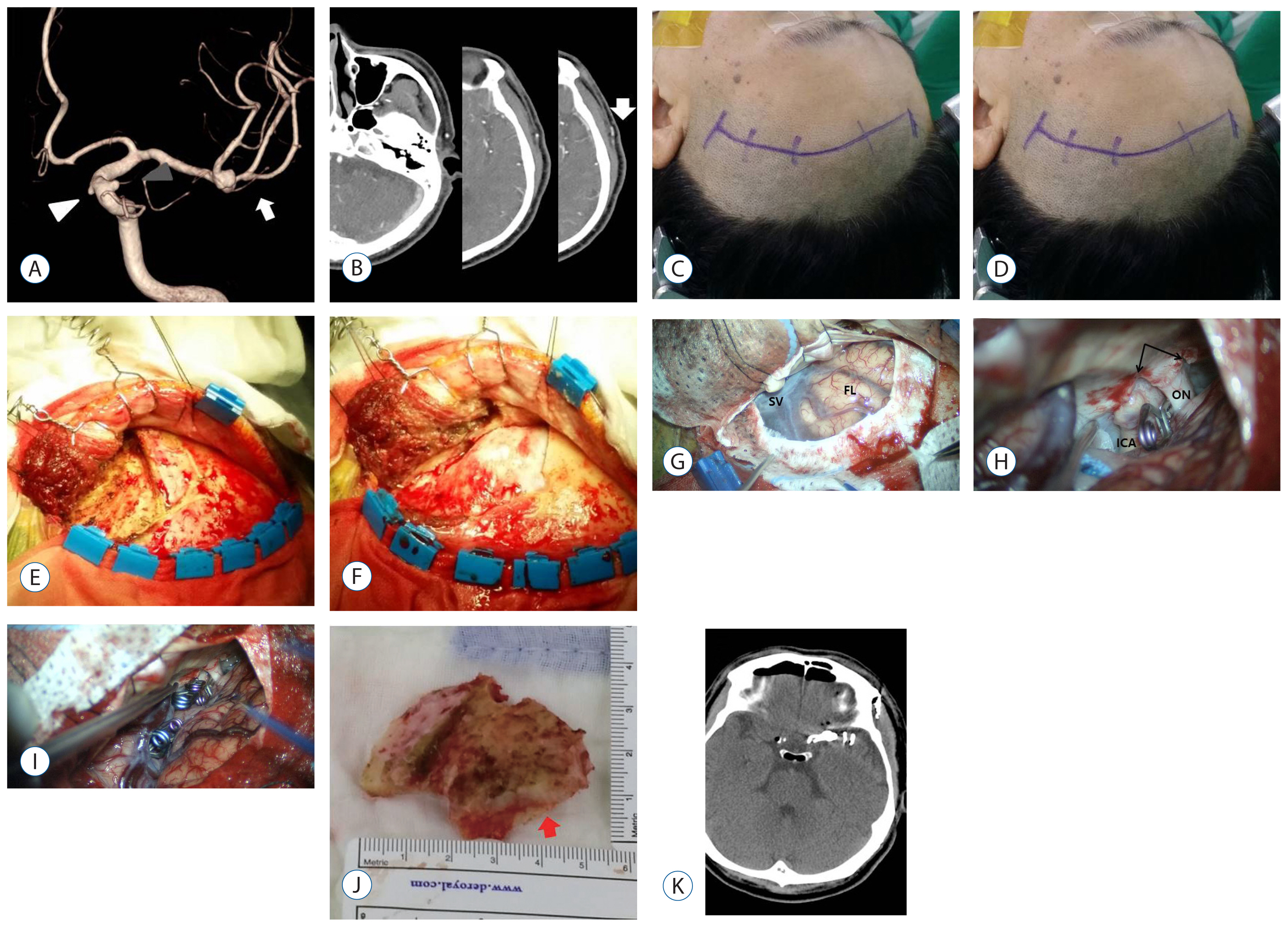
Superficial Temporal Artery-Sparing Mini-Pterional Approach for Cerebral Aneurysm Surgery
- Affiliations
-
- 1Department of Neurosurgery, Busan Paik Hospital, Inje University, College of Medicine, Busan, Korea. jyk91@inje.ac.kr
- KMID: 2365581
- DOI: http://doi.org/10.3340/jkns.2016.0707.004
Abstract
OBJECTIVE
The purposes of this study were to introduce a superficial temporal artery (STA)-sparing mini-pterional approach for the treatment of cerebral aneurysms and review the surgical results of this approach.
METHODS
Between June 2010 and December 2015, we performed the STA-sparing mini-pterional approach for 117 patients with 141 unruptured intracranial aneurysms. We analyzed demographic, radiologic, and clinical variables including age, sex, craniotomy size, aneurysm location, height of STA bifurcation, and postoperative complications.
RESULTS
The mean age of patients was 58.4 years. The height of STA bifurcation from the superior border of the zygomatic arch was 20.5 mm±10.0 (standard deviation [SD]). The craniotomy size was 1051.6 mm²±206.5 (SD). Aneurysm neck clipping was possible in all cases. Intradural anterior clinoidectomy was performed in four cases. Contralateral approaches to aneurysms were adopted for four cases. Surgery-related complications occurred in two cases. Permanent morbidity occurred in one case.
CONCLUSION
Our STA-sparing mini-pterional approach for surgical treatment of cerebral aneurysms is easy to learn and has the advantages of small incision, STA sparing, and a relatively wide surgical field. It may be a good alternative to the conventional pterional approach for treating cerebral aneurysms.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Microsurgical treatment for the recurrent cerebral aneurysm initially treated using coil embolization
Juwhan Lee, Sung-Tae Kim, Yong Woo Shim, Jin Wook Back, Jung Hae Ko, Won Hee Lee, Sung Hwa Paeng, Se Young Pyo, Young Jin Heo, Hae Woong Jeong, Young Gyun Jeong
J Cerebrovasc Endovasc Neurosurg. 2020;22(3):165-175. doi: 10.7461/jcen.2020.22.3.165.
Reference
-
References
1. Cheng WY, Lee HT, Sun MH, Shen CC. A pterion keyhole approach for the treatment of anterior circulation aneurysms. Minim Invasive Neurosurg. 49:257–262. 2006.
Article2. Figueiredo EG, Deshmukh P, Nakaji P, Crusius MU, Crawford N, Spetzler RF, et al. The minipterional craniotomy: Technical description and anatomic assessment. Neurosurgery. 61(5 Suppl 2):256–64. discussion 264–265. 2007.
Article3. Figueiredo EG, Deshmukh P, Zabramski JM, Preul MC, Crawford NR, Spetzler RF. The pterional-transsylvian approach: An analytical study. Neurosurgery. 62(6 Suppl 3):1361–1367. 2008.4. Figueiredo EG, Deshmukh V, Nakaji P, Deshmukh P, Crusius MU, Crawford N, et al. An anatomical evaluation of the mini-supraorbital approach and comparison with standard craniotomies. Neurosurgery. 59(4 Suppl 2):ONS212–220. discussion ONS220. 2006.
Article5. Grand W. Microsurgical anatomy of the proximal middle cerebral artery and the internal carotid artery bifurcation. Neurosurgery. 7:215–218. 1980.
Article6. Harland SP, Hussein A, Gullan RW. Modification of the standard pterional approach for aneurysms of the anterior circle of willis. Br J Neurosurg. 10:149–153. discussion 153. 1996.
Article7. Hernesniemi J, Ishii K, Niemela M, Smrcka M, Kivipelto L, Fujiki M, et al. Lateral supraorbital approach as an alternative to the classical pterional approach. Acta Neurochir Suppl. 94:17–21. 2005.
Article8. Jeong HW, Seo JH, Kim ST, Jung CK, Suh SI. Clinical practice guideline for the management of intracranial aneurysms. Neurointervention. 9:63–71. 2014.
Article9. Kim BS, Jung YJ, Chang CH, Choi BY. The anatomy of the superficial temporal artery in adult koreans using 3-dimensional computed tomographic angiogram: Clinical research. J Cerebrovasc Endovasc Neurosurg. 15:145–151. 2013.
Article10. Miyazawa T. Less invasive reconstruction of the temporalis muscle for pterional craniotomy: Modified procedures. Surg Neurol. 50:347–351. discussion 351. 1998.
Article11. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised trial. Lancet. 360:1267–1274. 2002.
Article12. Molyneux AJ, Birks J, Clarke A, Sneade M, Kerr RS. The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the international subarachnoid aneurysm trial (ISAT). Lancet. 385:691–697. 2015.
Article13. Oikawa S, Mizuno M, Muraoka S, Kobayashi S. Retrograde dissection of the temporalis muscle preventing muscle atrophy for pterional craniotomy. technical note. J Neurosurg. 84:297–299. 1996.
Article14. Pritz MB, Chandler WF. The transsylvian approach to middle cerebral artery bifurcation/trifurcation aneurysms. Surg Neurol. 41:217–219. discussion 219–220. 1994.
Article15. Rahmah NN, Murata T, Yako T, Horiuchi T, Hongo K. Correlation between squamous suture and sylvian fissure: OSIRIX DICOM viewer study. PLoS One. 6:e18199. 2011.
Article16. Steiner T, Juvela S, Unterberg A, Jung C, Forsting M, Rinkel G, et al. European stroke organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis. 35:93–112. 2013.
Article17. van Lindert E, Perneczky A, Fries G, Pierangeli E. The supraorbital keyhole approach to supratentorial aneurysms: concept and technique. Surg Neurol. 49:481–489. discussion 489–490. 1998.
Article18. Yamahata H, Tokimura H, Tajitsu K, Tsuchiya M, Taniguchi A, Hirabaru M, et al. Efficacy and safety of the pterional keyhole approach for the treatment of anterior circulation aneurysms. Neurosurg Rev. 37:629–636. 2014.
Article19. Yasargil MG, Fox JL. The microsurgical approach to intracranial aneurysms. Surg Neurol. 3:7–14. 1975.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aneurysms of the superficial temporal artery
- Interhemispheric Approach for Intracranial Aneurysms
- The Optimal Surgical Direction Concerning the Pterional Approach to the Anterior Communicating Artery Aneurysms
- Bvaluation of the Eyebrow Approach for Cerebral Aneurysm Surgery
- Traumatic Cerebral Aneurysm: A Case of Traumatic False Aneurysm of the Superficial Temporal Artery