Korean J Pain.
2016 Apr;29(2):123-128. 10.3344/kjp.2016.29.2.123.
Spinal Cauda Equina Stimulation for Alternative Location of Spinal Cord Stimulation in Intractable Phantom Limb Pain Syndrome: A Case Report
- Affiliations
-
- 1Department of Anaesthesiology and Pain Medicine, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. painfree@kuh.ac.kr
- KMID: 2365355
- DOI: http://doi.org/10.3344/kjp.2016.29.2.123
Abstract
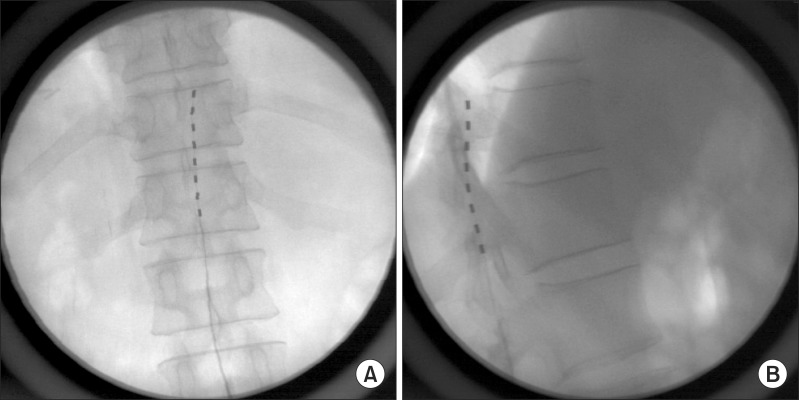
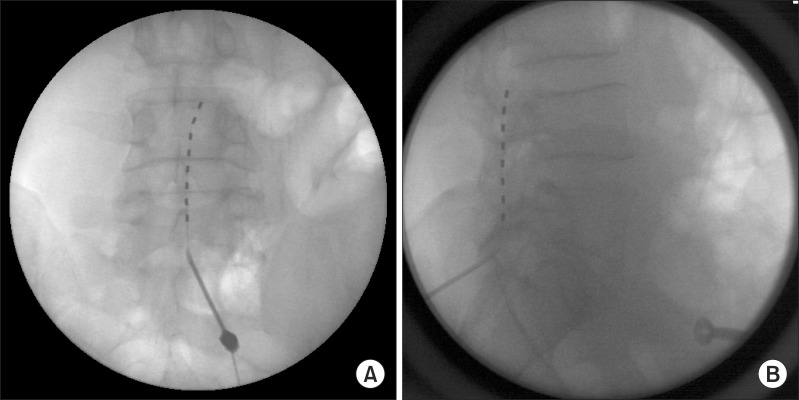
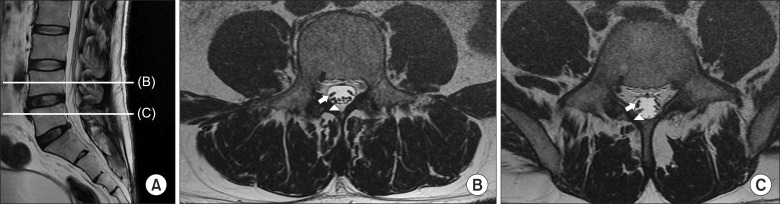
- Phantom limb pain is a phenomenon in which patients experience pain in a part of the body that no longer exists. In several treatment modalities, spinal cord stimulation (SCS) has been introduced for the management of intractable post-amputation pain. A 46-year-old male patient complained of severe ankle and foot pain, following above-the-knee amputation surgery on the right side amputation surgery three years earlier. Despite undergoing treatment with multiple modalities for pain management involving numerous oral and intravenous medications, nerve blocks, and pulsed radiofrequency (RF) treatment, the effect duration was temporary and the decreases in the patient's pain score were not acceptable. Even the use of SCS did not provide completely satisfactory pain management. However, the trial lead positioning in the cauda equina was able to stimulate the site of the severe pain, and the patient's pain score was dramatically decreased. We report a case of successful pain management with spinal cauda equina stimulation following the failure of SCS in the treatment of intractable phantom limb pain.
Keyword
MeSH Terms
Figure
Reference
-
1. Flor H. Phantom-limb pain: characteristics, causes, and treatment. Lancet Neurol. 2002; 1:182–189. PMID: 12849487.
Article2. Kim SY, Kim YY. Mirror therapy for phantom limb pain. Korean J Pain. 2012; 25:272–274. PMID: 23091690.
Article3. Ephraim PL, Wegener ST, MacKenzie EJ, Dillingham TR, Pezzin LE. Phantom pain, residual limb pain, and back pain in amputees: results of a national survey. Arch Phys Med Rehabil. 2005; 86:1910–1919. PMID: 16213230.
Article4. Sherman RA, Sherman CJ, Gall NG. A survey of current phantom limb pain treatment in the United States. Pain. 1980; 8:85–99. PMID: 6988765.
Article5. Nielson KD, Adams JE, Hosobuchi Y. Phantom limb pain. Treatment with dorsal column stimulation. J Neurosurg. 1975; 42:301–307. PMID: 1117328.6. Lee KH, Lee SE, Jung JW, Jeon SY. Spinal cord stimulation for intractable visceral pain due to sphincter of oddi dysfunction. Korean J Pain. 2015; 28:57–60. PMID: 25589948.
Article7. Jeon YH. Spinal cord stimulation in pain management: a review. Korean J Pain. 2012; 25:143–150. PMID: 22787543.
Article8. Wolter T. Spinal cord stimulation for neuropathic pain: current perspectives. J Pain Res. 2014; 7:651–663. PMID: 25429237.
Article9. Kooijman CM, Dijkstra PU, Geertzen JH, Elzinga A, van der Schans CP. Phantom pain and phantom sensations in upper limb amputees: an epidemiological study. Pain. 2000; 87:33–41. PMID: 10863043.
Article10. Houghton AD, Nicholls G, Houghton AL, Saadah E, McColl L. Phantom pain: natural history and association with rehabilitation. Ann R Coll Surg Engl. 1994; 76:22–25. PMID: 8117013.11. Weeks SR, Anderson-Barnes VC, Tsao JW. Phantom limb pain: theories and therapies. Neurologist. 2010; 16:277–286. PMID: 20827116.12. Baron R, Binder A, Wasner G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. 2010; 9:807–819. PMID: 20650402.
Article13. Woodhouse A. Phantom limb sensation. Clin Exp Pharmacol Physiol. 2005; 32:132–134. PMID: 15730449.
Article14. Ramachandran VS, Hirstein W. The perception of phantom limbs. The D. O. Hebb lecture. Brain. 1998; 121:1603–1630. PMID: 9762952.
Article15. Ramachandran VS, Stewart M, Rogers-Ramachandran DC. Perceptual correlates of massive cortical reorganization. Neuroreport. 1992; 3:583–586. PMID: 1421112.
Article16. Flor H, Nikolajsen L, Staehelin Jensen T. Phantom limb pain: a case of maladaptive CNS plasticity? Nat Rev Neurosci. 2006; 7:873–881. PMID: 17053811.
Article17. Eldabe S, Burger K, Moser H, Klase D, Schu S, Wahlstedt A, et al. Dorsal root ganglion (DRG) stimulation in the treatment of phantom limb pain (PLP). Neuromodulation. 2015; 18:610–616. PMID: 26268453.
Article18. George AT, Dudding TC, Gurmany S, Kamm MA, Nicholls RJ, Vaizey CJ. Pudendal nerve stimulation for bowel dysfunction in complete cauda equina syndrome. Ann Surg. 2014; 259:502–507. PMID: 23579581.
Article19. Shin JH, Kim YC, Jang IK, Kim JH, Park SY, Lee SC. Occipital nerve stimulation in a patient with an intractable chronic headache: a case report. Korean J Anesthesiol. 2011; 60:298–301. PMID: 21602983.
Article20. Verrills P, Russo M. Peripheral nerve stimulation for back pain. Prog Neurol Surg. 2015; 29:127–138. PMID: 26393502.
Article21. Park CH, Kim BI. Sacral nerve stimulation through the sacral hiatus. Korean J Pain. 2012; 25:195–197. PMID: 22787552.
Article22. Alo KM, Yland MJ, Redko V, Feler C, Naumann C. Lumbar and sacral nerve root stimulation (NRS) in the treatment of chronic pain: a novel anatomic approach and neuro stimulation technique. Neuromodulation. 1999; 2:23–31. PMID: 22151059.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trial Stimulation of the Spinal Cord for Relief of Pain: A 6-year Experience
- An Unexpected Improvement of the Symptom from Herniated Intervertebral Disc during Trial of Spinal Cord Stimulation for the Post-herpetic Neuralgia: A case report
- Spinal Cord Stimulation in Management of Intractable Chronic Pain: A 5-Year Experience
- Cauda Equina Syndrome after Spinal Manipulative Therapy: A case report
- Spinal cord stimulation for intractable post-thoracotomy pain syndrome: A case report