Korean J Pain.
2017 Jan;30(1):66-70. 10.3344/kjp.2017.30.1.66.
A brief report on a technical description of ultrasound-guided lumbar sympathetic block
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. jymoon0901@gmail.com
- 2Department of Anesthesiology and Pain Medicine, National Police Hospital, Seoul, Korea.
- 3Department of Anesthesiology and Pain Medicine, Apollo Speciality Hospitals, OMR, Chennai, India.
- KMID: 2365344
- DOI: http://doi.org/10.3344/kjp.2017.30.1.66
Abstract
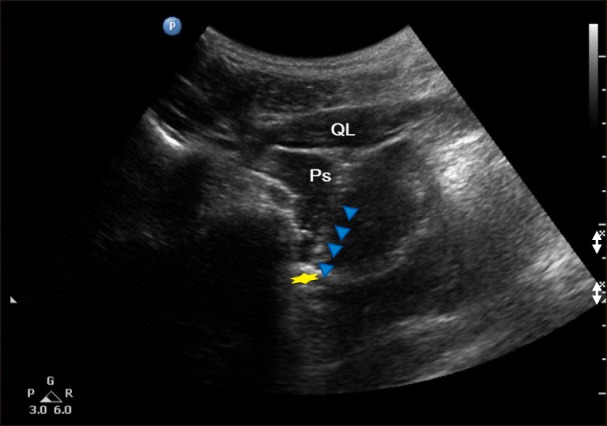
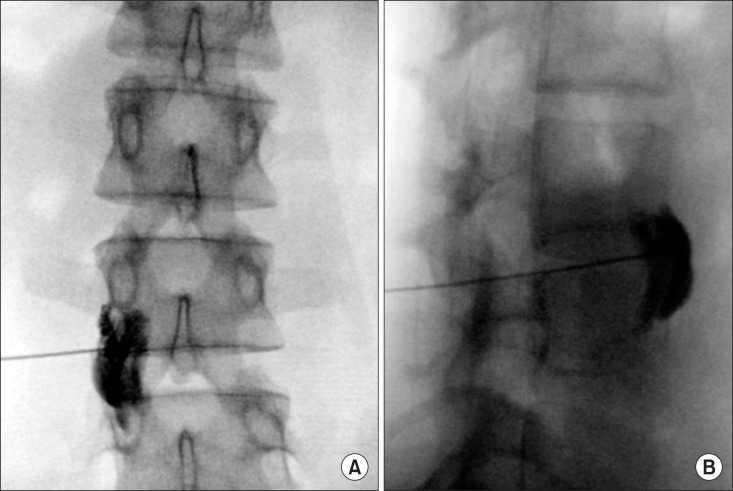
- The lumbar sympathetic ganglion block (LSGB) is widely used for diagnosing and treating sympathetically maintained pain disorders. The LSGB has been conventionally carried out under fluoroscopy or computed tomography guidance. However, as ultrasound technology improved, ultrasound-guided interventions have been expanding their territory to deeper structures. Ultrasound guidance provides many benefits including protecting vascular injection, shortening procedure time in some cases, and reducing the emission of radiation. In this report, we describe a successful case of a US-guided LSGB without major complications. We expect that US-guided LSGBs can be implemented and furnished in the daily outpatient clinical setting by highly trained pain physicians.
Keyword
Figure
Cited by 1 articles
-
The pros and cons of ultrasound-guided procedures in pain medicine
Jee Youn Moon
Korean J Pain. 2024;37(3):201-210. doi: 10.3344/kjp.23358.
Reference
-
1. Chaturvedi A, Dash HH. Sympathetic blockade for the relief of chronic pain. J Indian Med Assoc. 2001; 99:698–703. PMID: 12022220.2. Rigaud J, Delavierre D, Sibert L, Labat JJ. Sympathetic nerve block in the management of chronic pelvic and perineal pain. Prog Urol. 2010; 20:1124–1131. PMID: 21056394.3. Oi Y, Nakamura K, Sakamoto A, Ogawa R, Watari J, Okajima Y, et al. Helical CT guided lumar sympathetic ganglion block. Masui. 1996; 45:888–891. PMID: 8741484.4. Manchikanti L, Cash KA, Moss TL, Pampati V. Radiation exposure to the physician in interventional pain management. Pain Physician. 2002; 5:385–393. PMID: 16886017.
Article5. Jee H, Lee JH, Kim J, Park KD, Lee WY, Park Y. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: a randomized, blinded, controlled study. Skeletal Radiol. 2013; 42:69–78. PMID: 22609989.
Article6. Park Y, Lee JH, Park KD, Ahn JK, Park J, Jee H. Ultrasound-guided vs. fluoroscopy-guided caudal epidural steroid injection for the treatment of unilateral lower lumbar radicular pain: a prospective, randomized, single-blind clinical study. Am J Phys Med Rehabil. 2013; 92:575–586. PMID: 23636087.
Article7. Narouze S. Ultrasound-guided stellate ganglion block: safety and efficacy. Curr Pain Headache Rep. 2014; 18:424. PMID: 24760493.
Article8. Gofeld M, Lee CW. Ultrasound-guided superior hypogastric plexus block: a cadaveric feasibility study with fluoroscopic confirmation. Pain Pract. 2016; [in press].
Article9. Moura RN, De Moura EG, Bernardo WM, Otoch JP, Bustamante FA, Albers DV, et al. Endoscopic-ultrasound versus percutaneous-guided celiac plexus block for chronic pancreatitis pain. A systematic review and meta-analysis. Rev Gastroenterol Peru. 2015; 35:333–341. PMID: 26802887.10. Kirvelä O, Svedström E, Lundbom N. Ultrasonic guidance of lumbar sympathetic and celiac plexus block: a new technique. Reg Anesth. 1992; 17:43–46. PMID: 1599894.11. Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007; 8:326–331. PMID: 17610454.
Article12. Nordmann GR, Lauder GR, Grier DJ. Computed tomography guided lumbar sympathetic block for complex regional pain syndrome in a child: a case report and review. Eur J Pain. 2006; 10:409–412. PMID: 15979912.
Article13. Finlayson RJ, Etheridge JP, Tiyaprasertkul W, Nelems B, Tran DQ. A randomized comparison between ultrasound- and fluoroscopy-guided c7 medial branch block. Reg Anesth Pain Med. 2015; 40:52–57. PMID: 25478757.
Article14. Karmakar MK, Ho AM, Li X, Kwok WH, Tsang K, Ngan Kee WD. Ultrasound-guided lumbar plexus block through the acoustic window of the lumbar ultrasound trident. Br J Anaesth. 2008; 100:533–537. PMID: 18344573.
Article15. Kim DH, Kim KH, Kim YC. Minimally invasive percutaneous spinal techniques. Philadelphia (PA): Elsevier;2011.16. Kim WH, Kim SK, Lee CJ, Kim TH, Sim WS. Determination of adequate entry angle of lumbar sympathetic ganglion block in Korean. Korean J Pain. 2010; 23:11–17. PMID: 20552067.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-Guided Intervention in Lumbar Spine
- Ultrasound Guided Nerve Block at Vertebra and Lower Extremity
- Ultrasound-Guided Lumbar Transforaminal Epidural Injection: A Narrative Review
- A Case of Erection Failure due to Unilateral Lumbar Sympathetic Block
- Degenerative Diseases and Ultrasound-guided Intervention in Lumbar Spine