Investig Clin Urol.
2017 Jan;58(1):20-26. 10.4111/icu.2017.58.1.20.
Lymph node density predicts recurrence and death after inguinal lymph node dissection for penile cancer
- Affiliations
-
- 1The James Buchanan Brady Urological Institute, Department of Urology, The Johns Hopkins University School of Medicine, Baltimore, MD, USA. mark.ball@jhmi.edu
- 2Department of Pathology, The Johns Hopkins University School of Medicine, Baltimore, MD, USA.
- KMID: 2365092
- DOI: http://doi.org/10.4111/icu.2017.58.1.20
Abstract
- PURPOSE
To determine the impact of lymph node density (LND) on survival after inguinal lymph node dissection (ILND) for penile cancer.
MATERIALS AND METHODS
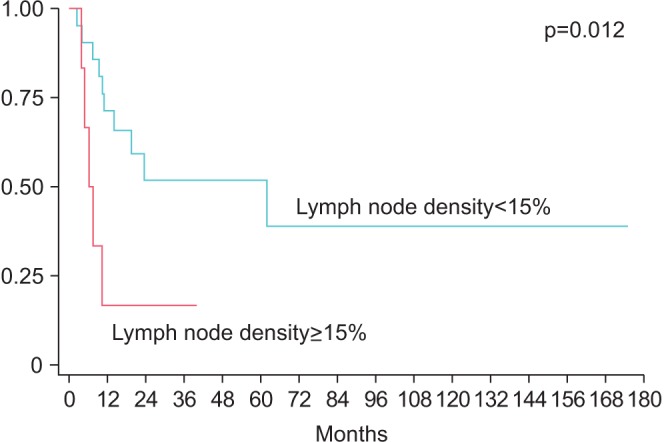
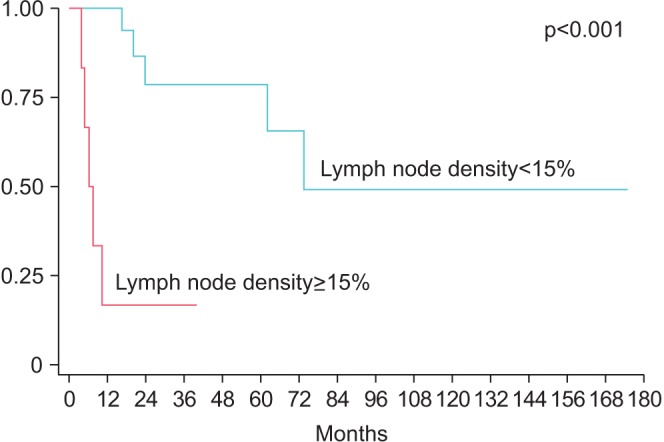
Our institutional penile cancer database was queried for patients who underwent ILND. Clinicopathologic characteristics including LND and total number of positive lymph nodes (LNs) were analyzed to determine impact on recurrence-free survival (RFS) and overall survival (OS). LND, or the percent of positive LN out of total LN, was calculated as a categorical variable at varying thresholds.
RESULTS
Twenty-eight patients with complete follow-up were identified. Indications for ILND were stage >T2 in 20 patients (71.4%), palpable adenopathy in 7 (25%), high grade T1 in 1 (3.6%). Median node yield was 17.5 (interquartile range, 12−22), and positive LNs were found in 14 patients (50%). RFS and OS were significantly lower for patients with >15% LN density (median RFS: 62 months vs. 6.3 months, p=0.0120; median OS: 73.6 months vs. 6.3 months, p<0.001). Controlling for age, medical comorbidities, number of positive LN, T stage, pelvic LN status and indication, LN density >15% was independently associated with worse RFS (hazard ratio [HR], 3.6; p=0.04) and OS (HR, 73.6; p=0.002). The c-index for LND was higher than total positive LNs for RFS (0.64 vs. 0.54) and OS (0.79 vs. 0.61).
CONCLUSIONS
In this small, retrospective penile cancer cohort, the presence of nodal involvement >15% was associated with decreased RFS and OS, and outperformed total number of positive LN as a prognostic indicator.
MeSH Terms
Figure
Cited by 1 articles
-
Lymph node density predicts recurrence and death after inguinal lymph node dissection for penile cancer
Mark W. Ball, Zeyad R. Schwen, Joan S. Ko, Alexa Meyer, George J. Netto, Arthur L. Burnett, Trinity J. Bivalacqua
Investig Clin Urol. 2017;58(1):20-26. doi: 10.4111/icu.2017.58.1.20.
Reference
-
1. Leijte JA, Gallee M, Antonini N, Horenblas S. Evaluation of current TNM classification of penile carcinoma. J Urol. 2008; 180:933–938. PMID: 18635216.2. Pandey D, Mahajan V, Kannan RR. Prognostic factors in nodepositive carcinoma of the penis. J Surg Oncol. 2006; 93:133–138. PMID: 16425300.
Article3. Protzel C, Alcaraz A, Horenblas S, Pizzocaro G, Zlotta A, Hakenberg OW. Lymphadenectomy in the surgical management of penile cancer. Eur Urol. 2009; 55:1075–1088. PMID: 19264390.
Article4. Ornellas AA, Kinchin EW, Nóbrega BL, Wisnescky A, Koifman N, Quirino R. Surgical treatment of invasive squamous cell carcinoma of the penis: Brazilian National Cancer Institute long-term experience. J Surg Oncol. 2008; 97:487–495. PMID: 18425779.
Article5. Ornellas AA, Seixas AL, de Moraes JR. Analyses of 200 lymphadenectomies in patients with penile carcinoma. J Urol. 1991; 146:330–332. PMID: 1830347.6. Ravi R. Correlation between the extent of nodal involvement and survival following groin dissection for carcinoma of the penis. Br J Urol. 1993; 72(5 Pt 2):817–819. PMID: 8281416.
Article7. Zhu Y, Ye DW, Yao XD, Zhang SL, Dai B, Zhang HL. New N staging system of penile cancer provides a better reflection of prognosis. J Urol. 2011; 186:518–523. PMID: 21679992.
Article8. Hakenberg OW, Compérat EM, Minhas S, Necchi A, Protzel C, Watkin N, et al. EAU guidelines on penile cancer: 2014 update. Eur Urol. 2015; 67:142–150. PMID: 25457021.
Article9. Johnson TV, Hsiao W, Delman KA, Jani AB, Brawley OW, Master VA. Extensive inguinal lymphadenectomy improves overall 5-year survival in penile cancer patients: results from the Surveillance, Epidemiology, and End Results program. Cancer. 2010; 116:2960–2966. PMID: 20564401.
Article10. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010; 17:1471–1474. PMID: 20180029.
Article11. Liu JY, Li YH, Zhang ZL, Yao K, Ye YL, Xie D, et al. The risk factors for the presence of pelvic lymph node metastasis in penile squamous cell carcinoma patients with inguinal lymph node dissection. World J Urol. 2013; 31:1519–1524. PMID: 23455885.
Article12. Zhu Y, Gu CY, Ye DW. Population-based assessment of the number of lymph nodes removed in the treatment of penile squamous cell carcinoma. Urol Int. 2014; 92:186–193. PMID: 24246932.13. Li ZS, Yao K, Chen P, Zou ZJ, Qin ZK, Liu ZW, et al. Disease-specific survival after radical lymphadenectomy for penile cancer: prediction by lymph node count and density. Urol Oncol. 2014; 32:893–900. PMID: 24994488.
Article14. Lughezzani G, Catanzaro M, Torelli T, Piva L, Biasoni D, Stagni S, et al. Relationship between lymph node ratio and cancer-specific survival in a contemporary series of patients with penile cancer and lymph node metastases. BJU Int. 2015; 116:727–733. PMID: 24128128.
Article15. Svatek RS, Munsell M, Kincaid JM, Hegarty P, Slaton JW, Busby JE, et al. Association between lymph node density and disease specific survival in patients with penile cancer. J Urol. 2009; 182:2721–2727. PMID: 19837433.
Article16. Zhu Y, Gu CY, Ye DW. Validation of the prognostic value of lymph node ratio in patients with penile squamous cell carcinoma: a population-based study. Int Urol Nephrol. 2013; 45:1263–1271. PMID: 23877663.17. Daneshmand S, Quek ML, Stein JP, Lieskovsky G, Cai J, Pinski J, et al. Prognosis of patients with lymph node positive prostate cancer following radical prostatectomy: long-term results. J Urol. 2004; 172(6 Pt 1):2252–2255. PMID: 15538242.18. Kassouf W, Leibovici D, Munsell MF, Dinney CP, Grossman HB, Kamat AM. Evaluation of the relevance of lymph node density in a contemporary series of patients undergoing radical cystectomy. J Urol. 2006; 176:53–57. PMID: 16753366.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Implication of Lateral Pelvic Lymph Node Metastasis in Rectal Cancer Treated with Neoadjuvant Chemoradiotherapy
- Treatment of Malignant Melanoma Using Sentinel Lymph Node Dissection
- Advantages of Splenic Hilar Lymph Node Dissection in Proximal Gastric Cancer Surgery
- Sentinel Lymph Node Biopsy in the Oral Cavity Cancer
- A Clinical Review of Lymph Node Metastases for Papillary Thyroid Cancer