Ann Surg Treat Res.
2017 Jan;92(1):42-46. 10.4174/astr.2017.92.1.42.
Usefulness of intraopertive ultrasonography during directional atherectomy using SilverHawk/TurboHawk system
- Affiliations
-
- 1Division of Vascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dikim@skku.edu
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2364713
- DOI: http://doi.org/10.4174/astr.2017.92.1.42
Abstract
- PURPOSE
Directional atherectomy (DA) was introduced for the management of infrainguinal arterial stenosis or occlusive lesions. The procedure success rate in the DEFINITIVE LE study was determined using radiologic imaging. The aim of our study was to determine the usefulness of intraoperative ultrasonography (USG) during DA for evaluating the early results of this procedure.
METHODS
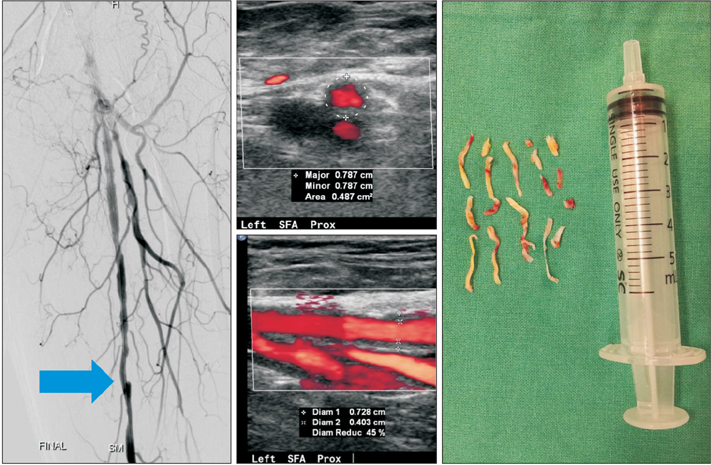
Patients who underwent DA from January to December 2014 were reviewed retrospectively. Twenty lesions from 14 patients with femoral artery stenosis (>70% stenosis) with short segment occlusive lesions (<2 cm in length) were treated. Among 20 lesions, 3 were treated with the TurboHawk system with a protective device due to lesion calcification. The percentage of stenosis during and after DA was determined with USG.
RESULTS
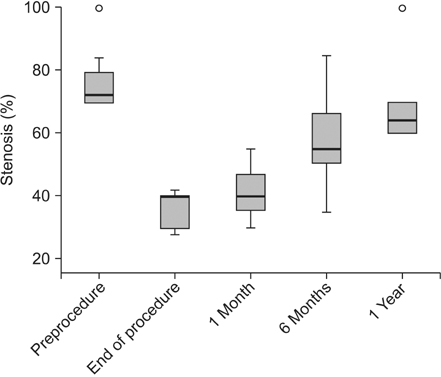
Median follow-up was 5.1 months, and the procedural success rate (<30% stenosis at the end of the procedure) was 100% on angiography, but only 30% on intraoperative USG. On USG, median residual stenosis was 40% (range, 28%-42%) at the end of DA, 40% (range, 30%-55%) at 1 month, 55% (range, 35%-85%) at 6 months, and 64% (range, 60%-100%) at 1 year. There was one dissection, but no cases of perforation, pseudoaneurysm, or thrombosis. Primary patency, which was defined as a peak systolic velocity ratio ≤3.5 with no reintervention at 6 months, was found in 18 lesions (90%), and 11 of 14 patients (78.6%) were free of ischemic symptoms such as claudication at 6 months.
CONCLUSION
Our results demonstrated that DA with intraoperative USG is an effective treatment option for short segment occlusive lesions of the femoral artery.
Keyword
MeSH Terms
Figure
Reference
-
1. Dotter CT, Frische LH, Judkins MP, Mueller R. The “nonsurgical” treatment of iliofemoral arteriosclerotic obstruction. Radiology. 1966; 86:871–875.2. Rogers JH, Laird JR. Overview of new technologies for lower extremity revascularization. Circulation. 2007; 116:2072–2085.3. McKinsey JF, Zeller T, Rocha-Singh KJ, Jaff MR, Garcia LA. DEFINITIVE LE Investigators. Lower extremity revascularization using directional atherectomy: 12-month prospective results of the DEFINITIVE LE study. JACC Cardiovasc Interv. 2014; 7:923–933.4. Zeller T, Rastan A, Sixt S, Schwarzwalder U, Schwarz T, Frank U, et al. Long-term results after directional atherectomy of femoro-popliteal lesions. J Am Coll Cardiol. 2006; 48:1573–1578.5. Jaff MR. Advances in the management of patients with vascular disease. Expert Rev Cardiovasc Ther. 2012; 10:151–153.6. Diethrich EB, Irshad K, Reid DB. Virtual histology and color flow intravascular ultrasound in peripheral interventions. Semin Vasc Surg. 2006; 19:155–162.7. Prati F, Regar E, Mintz GS, Arbustini E, Di Mario C, Jang IK, et al. Expert review document on methodology, terminology, and clinical applications of optical coherence tomography: physical principles, methodology of image acquisition, and clinical application for assessment of coronary arteries and atherosclerosis. Eur Heart J. 2010; 31:401–415.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experience with Directional Atherectomy in Infrainguinal Peripheral Arterial Disease with Using a Silverhawk Plaque Excision Device
- Early and Late Clinical Outcomes after Directional Coronary Atherectomy
- Directional Coronary Atherectomy (Simpson AtheroCath) : Reasons for Device Selection, Angiographic and Histologic Findings, and Its Mechanisms
- Below the Knee Intervention Using Multidisciplinary Methods Including an Antegrade, Retrograde Approach Without the Use of a Sheath but With a Plaque Excision Device
- Coronary Artery Proliferation and Remodeling after Coronary Artery Stenting and Directional Coronary Atherectomy