Blood Res.
2016 Dec;51(4):268-273. 10.5045/br.2016.51.4.268.
Iron deficiency anemia in infants and toddlers
- Affiliations
-
- 1Department of Pediatrics, Inha University College of Medicine, Incheon, Korea. pedkim@inha.ac.kr
- KMID: 2364318
- DOI: http://doi.org/10.5045/br.2016.51.4.268
Abstract
- BACKGROUND
In Korea, the prevalence of anemia and iron deficiency anemia (IDA) among older infants and young children remains high. To detect IDA early and to reduce its adverse impact, we assessed the characteristics of infants and young children who had IDA or were at risk of developing IDA, or who exhibited characteristics associated with severe anemia.
METHODS
Among the 1,782 IDA-affected children aged 6 months to 18 years who visited the hospital, we retrospectively analyzed the medical records and laboratory data of 1,330 IDA-affected children aged 6-23 months who were diagnosed between 1996 and 2013. We excluded patients with a C-reactive protein level ≥5 mg/dL.
RESULTS
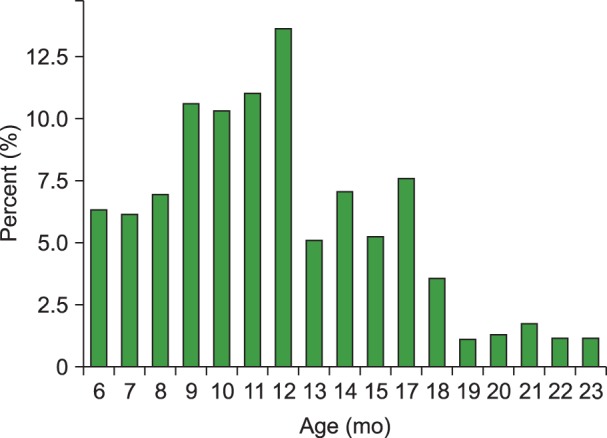
IDA was predominant in boys (2.14:1) during infancy and early childhood. The peak IDA incidence was noted among infants aged 9-12 months. Only 7% patients exhibited symptoms of IDA, while 23.6% patients with severe IDA demonstrated classic symptoms/signs of IDA. Low birth weight (LBW) infants with IDA demonstrated low adherence to iron supplementation. In a multivariate analysis, prolonged breastfeeding without iron fortification (odds ratio [OR] 5.70), and a LBW (OR 6.49) were identified as risk factors of severe anemia.
CONCLUSION
LBW infants need more attention in order to increase their adherence to iron supplementation. For the early detection of IDA, nutritional status of all infants, and iron batteries of high-risk infants (LBW infants, infants with prolonged breastfeeding, picky eaters, and/or infants with the presence of IDA symptoms) should be evaluated at their health screening visits.
MeSH Terms
Figure
Reference
-
1. World Health Organization. Iron deficiency anaemia: assessment, prevention and control: A guide for programme managers. Geneva, Switzerland: World Health Organization;2001. Accessed October 2, 2015. at http://www.who.int/nutrition/publications/micronutrients/anaemia_iron_deficiency/WHO_NHD_01.3/en/index.html.2. Hopkins D, Emmett P, Steer C, Rogers I, Noble S, Emond A. Infant feeding in the second 6 months of life related to iron status: an observational study. Arch Dis Child. 2007; 92:850–854. PMID: 17537759.
Article3. Looker AC, Dallman PR, Carroll MD, Gunter EW, Johnson CL. Prevalence of iron deficiency in the United States. JAMA. 1997; 277:973–976. PMID: 9091669.
Article4. Zlotkin SH, Christofides AL, Hyder SM, Schauer CS, Tondeur MC, Sharieff W. Controlling iron deficiency anemia through the use of home-fortified complementary foods. Indian J Pediatr. 2004; 71:1015–1019. PMID: 15572823.
Article5. Soh P, Ferguson EL, McKenzie JE, Homs MY, Gibson RS. Iron deficiency and risk factors for lower iron stores in 6-24-month-old New Zealanders. Eur J Clin Nutr. 2004; 58:71–79. PMID: 14679370.
Article6. Grant CC, Wall CR, Brunt D, Crengle S, Scragg R. Population prevalence and risk factors for iron deficiency in Auckland, New Zealand. J Paediatr Child Health. 2007; 43:532–538. PMID: 17635681.
Article7. World Health Organization. The global prevalence of anaemia in 2011. Geneva, Switzerland: World Health Organization;2015.8. Korean Statistical Information Service. National health insurance statistical annual report classification of 298 disease categories by age, national health insurance service, health insurance review, and assessment service. Daejeon, Korea: Korean Statistical Information Service;2014. Accessed June 30, 2016. at http://kosis.kr/statHtml/statHtml.do?orgId=350&tblId=TX_35001_A061&conn_path=I2.9. Pollitt E. Iron deficiency and cognitive function. Annu Rev Nutr. 1993; 13:521–537. PMID: 8369157.
Article10. Carter RC, Jacobson JL, Burden MJ, et al. Iron deficiency anemia and cognitive function in infancy. Pediatrics. 2010; 126:e427–e434. PMID: 20660551.
Article11. Lozoff B, Jimenez E, Hagen J, Mollen E, Wolf AW. Poorer behavioral and developmental outcome more than 10 years after treatment for iron deficiency in infancy. Pediatrics. 2000; 105:E51. PMID: 10742372.
Article12. Khedr E, Hamed SA, Elbeih E, El-Shereef H, Ahmad Y, Ahmed S. Iron states and cognitive abilities in young adults: neuropsychological and neurophysiological assessment. Eur Arch Psychiatry Clin Neurosci. 2008; 258:489–496. PMID: 18574611.
Article13. World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. Geneva, Switzerland: World Health Organization;2011. Accessed January 11, 2016. at http://www.who.int/vmnis/indicators/haemoglobin.pdf.14. World Health Organization. Serum ferritin concentrations for the assessment of iron status and iron deficiency in populations. Vitamin and Mineral Nutrition Information System. Geneva, Switzerland: World Health Organization;2011. Accessed January 11, 2016. at http://www.who.int/vmnis/indicators/serum_ferritin.pdf.15. Wu AC, Lesperance L, Bernstein H. Screening for iron deficiency. Pediatr Rev. 2002; 23:171–178. PMID: 11986493.
Article16. Lozoff B, Kaciroti N, Walter T. Iron deficiency in infancy: applying a physiologic framework for prediction. Am J Clin Nutr. 2006; 84:1412–1421. PMID: 17158425.
Article17. Domellöf M, Lönnerdal B, Dewey KG, Cohen RJ, Rivera LL, Hernell O. Sex differences in iron status during infancy. Pediatrics. 2002; 110:545–552. PMID: 12205258.18. Wieringa FT, Berger J, Dijkhuizen MA, et al. Sex differences in prevalence of anaemia and iron deficiency in infancy in a large multi-country trial in South-East Asia. Br J Nutr. 2007; 98:1070–1076. PMID: 17537292.
Article19. Choi JW, Kim CS, Pai SH. Erythropoietic activity and soluble transferrin receptor level in neonates and maternal blood. Acta Paediatr. 2000; 89:675–679. PMID: 10914961.
Article20. Calvo EB, Galindo AC, Aspres NB. Iron status in exclusively breast-fed infants. Pediatrics. 1992; 90:375–379. PMID: 1518691.
Article21. Shin PJ, Bae CW, Choi YM. A comparative study of red blood cell indices and anemia by feeding patterns. J Korean Pediatr Soc. 1999; 42:1104–1110.22. Baker RD, Greer FR. Committee on Nutrition American Academy of Pediatrics. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0-3 years of age). Pediatrics. 2010; 126:1040–1050. PMID: 20923825.
Article23. Berglund S, Westrup B, Domellöf M. Iron supplements reduce the risk of iron deficiency anemia in marginally low birth weight infants. Pediatrics. 2010; 126:e874–e883. PMID: 20819898.
Article24. Park SH, Kim JS, Jun YH, Kim SK. Weaning food practice in low birth weight infants with iron deficiency anemia. Clin Pediatr Hematol Oncol. 2014; 21:52–58.
Article25. Ministry of Health and Welfare. Korea Health Statistics 2014: Korea National Health and Nutrition Examination Survey (KNHANES VI-2). Cheongju, Korea: Korea Centers for Disease Control and Prevention;2015.26. Kim BY, Choi EH, Kang SK, Jun YH, Hong YJ, Kim SK. Weaning food practice and assessment in children with iron deficiency anemia. Korean J Pediatr Gastroenterol Nutr. 2009; 12:215–220.
Article27. Kim YH, Lee SG, Kim SH, Song YJ, Chung JY, Park MJ. Nutritional status of Korean toddlers: From the Korean National Health and Nutrition Examination Survey 2007∼2009. Korean J Pediatr Gastroenterol Nutr. 2011; 14:161–170.
Article28. Siu AL. US Preventive Services Task Force. Screening for iron deficiency anemia in young children: USPSTF recommendation statement. Pediatrics. 2015; 136:746–752. PMID: 26347426.
Article29. Kim HJ, Kim DH, Lee JE, et al. Is it possible to predict the iron status from an infant’s diet history? Pediatr Gastroenterol Hepatol Nutr. 2013; 16:95–103. PMID: 24010113.
Article30. World Health Organization. Essential nutrition actions: Improving maternal, newborn, infant and young child health and nutrition. Geneva, Switzerland: World Health Organization;2013. Accessed July 1, 2016. at http://www.who.int/nutrition/publications/infantfeeding/essential_nutrition_actions/en/.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Iron Deficiency Anemia in Infants
- Intravenous Iron Sucrose for Three Children with Iron Deficiency Anemia Failing to Respond to Oral Iron Therapy
- Molecular perspective of iron uptake, related diseases, and treatments
- H. pylori-associated Iron-Deficiency Anemia
- A comparative study on iron deficiency anemia based on feeding patterns of nine-month-old infants