Investig Clin Urol.
2016 Jan;57(1):45-49. 10.4111/icu.2016.57.1.45.
Chromosomal aberrations in benign prostatic hyperplasia patients
- Affiliations
-
- 1Department of Urology, Faculty of Medicine, Suleyman Demirel University, Isparta, Turkey. muammeraltok@sdu.edu.tr
- 2Department of Medical Genetics, Faculty of Medicine, Suleyman Demirel University, Isparta, Turkey.
- 3Department of Urology, Haydarpasa Numune Education and Research Hospital, Istanbul, Turkey.
- 4Department of Urology, Fatih Sultan Mehmet Education and Research Hospital, Istanbul, Turkey.
- KMID: 2363123
- DOI: http://doi.org/10.4111/icu.2016.57.1.45
Abstract
- PURPOSE
To investigate the chromosomal changes in patients with benign prostatic hyperplasia (BPH).
MATERIALS AND METHODS
A total of 54 patients diagnosed with clinical BPH underwent transurethral prostate resection to address their primary urological problem. All patients were evaluated by use of a comprehensive medical history and rectal digital examination. The preoperative evaluation also included serum prostate-specific antigen (PSA) measurement and ultrasonographic measurement of prostate volume. Prostate cancer was detected in one patient, who was then excluded from the study. We performed conventional cytogenetic analyses of short-term cultures of 53 peripheral blood samples obtained from the BPH patients.
RESULTS
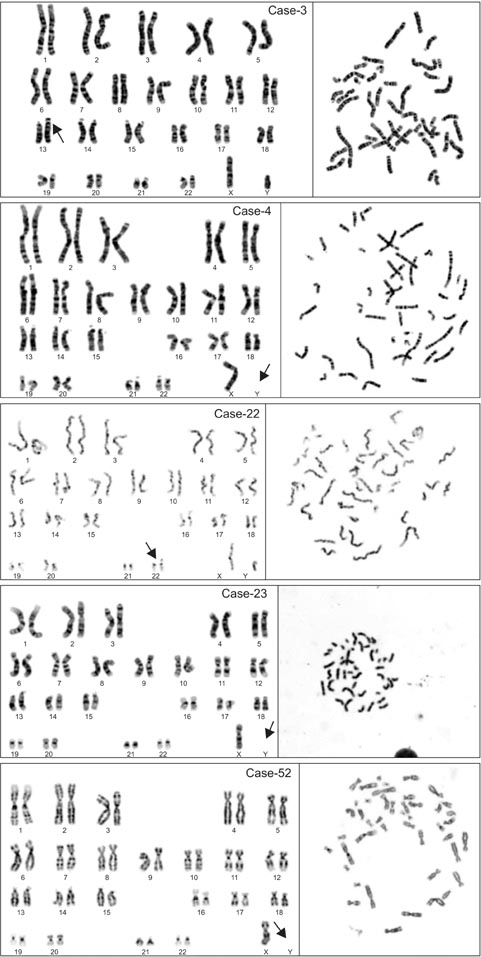
The mean (+/-standard deviation) age of the 53 patients was 67.8+/-9.4 years. The mean PSA value of the patients was 5.8+/-7.0 ng/mL. The mean prostate volume was 53.6+/-22.9 mL. Chromosomal abnormalities were noted in 5 of the 53 cases (9.4%). Loss of the Y chromosome was the most frequent chromosomal abnormality and was observed in three patients (5.7%). There was no statistically significant relationship among age, PSA, prostate volume, and chromosomal changes.
CONCLUSIONS
Loss of the Y chromosome was the main chromosomal abnormality found in our study. However, this coexistence did not reach a significant level. Our study concluded that loss of the Y chromosome cannot be considered relevant for the diagnosis of BPH as it is for prostate cancer. Because BPH usually occurs in aging men, loss of the Y chromosome in BPH patients may instead be related to the aging process.
Keyword
MeSH Terms
Figure
Reference
-
1. McVary KT, Roehrborn CG, Avins AL, Barry MJ, Bruskewitz RC, Donnell RF, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011; 185:1793–1803.2. David M, Berman RR, Veltri RW. Development, molecular biology, and physiology of the prostate. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders;2012. p. 2533–2569.3. Dal Cin P, Van Den Berghe H. Chromosome abnormalities in benign prostatic hyperplasia. In : Petrovich Z, Baert L, editors. Benign prostatic hyperplasia: innovations in management. New York: Springer-Verlag;1994. p. 49–56.4. Balachandar V, Kumar BL, Devi SM, Sangeetha R, Manikantan P, Kumar SS, et al. Identification of chromosome aberrations among benign prostatic hyperplasia patients in tamilnadu, Southern India. Int J Hum Genet. 2010; 10:159–164.5. Aly MS, Dal Cin P, Van de Voorde W, van Poppel H, Ameye F, Baert L, et al. Chromosome abnormalities in benign prostatic hyperplasia. Genes Chromosomes Cancer. 1994; 9:227–233.6. Casalone R, Portentoso P, Granata P, Minelli E, Righi R, Meroni E, et al. Chromosome changes in benign prostatic hyperplasia and their significance in the origin of prostatic carcinoma. Cancer Genet Cytogenet. 1993; 68:126–130.7. Brothman AR, Lesho LJ, Somers KD, Schellhammer PF, Ladaga LE, Merchant DJ. Cytogenetic analysis of four primary prostatic cultures. Cancer Genet Cytogenet. 1989; 37:241–248.8. Shaffer LG, McGowan-Jordan J, Schmid M, editors. ISCN 2013: an international system for human cytogenetic nomenclature. Basel: Karger;2013.9. Roehrborn CG. Benign prostatic hyperplasia: etiology, pathophysiology, epidemiology, and natural history. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders;2012. p. 2570–2610.10. Mitelman F. Catalog of chromosome aberrations in cancer. 4th ed. New York: Wiley;1991.11. Hagmar L, Bonassi S, Stromberg U, Brøgger A, Knudsen LE, Norppa H, et al. Chromosomal aberrations in lymphocytes predict human cancer: a report from the European Study Group on Cytogenetic Biomarkers and Health (ESCH). Cancer Res. 1998; 58:4117–4121.12. Bonassi S, Abbondandolo A, Camurri L, Dal Pra L, De Ferrari M, Degrassi F, et al. Are chromosome aberrations in circulating lymphocytes predictive of future cancer onset in humans? Preliminary results of an Italian cohort study. Cancer Genet Cytogenet. 1995; 79:133–135.13. Jellinghaus W, Okada K, Ragg C, Gerhard H, Schröder FH. Chromosomal studies of human prostatic tumors in vitro. Invest Urol. 1976; 14:16–19.14. Gu Y, Li H, Miki J, Kim KH, Furusato B, Sesterhenn IA, et al. Phenotypic characterization of telomerase-immortalized primary non-malignant and malignant tumor-derived human prostate epithelial cell lines. Exp Cell Res. 2006; 312:831–843.15. Nadal M, Pera G, Pujadas J, Abril J, Gonzalez L, Aguilo F, et al. Aneuploidy of chromosome Y in prostate tumors and seminal vesicles: a possible sign of aging rather than an indicator of carcinogenesis? Mol Carcinog. 2007; 46:543–552.16. Donnell RF. Benign prostate hyperplasia: a review of the year's progress from bench to clinic. Curr Opin Urol. 2011; 21:22–26.17. Mottet N, Bastian PJ, Bellmunt J, van den Bergh RC, Bolla M, van Casteren NJ, et al. Guideline on prostate cancer. Anheim (NL): European Association of Urology;2014.18. Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015; 67:1099–1109.19. Van Dekken H, Alers J. Loss of chromosome Y in prostatic cancer cells but not in stromal tissue. Cancer Genet Cytogenet. 1993; 66:131–132.20. Catalan J, Autio K, Kuosma E, Norppa H. Age-dependent inclusion of sex chromosomes in lymphocyte micronuclei of man. Am J Hum Genet. 1998; 63:1464–1472.21. Stone JF, Sandberg AA. Sex chromosome aneuploidy and aging. Mutat Res. 1995; 338:107–113.22. Guttenbach M, Koschorz B, Bernthaler U, Grimm T, Schmid M. Sex chromosome loss and aging: in situ hybridization studies on human interphase nuclei. Am J Hum Genet. 1995; 57:1143–1150.23. Fitzgerald PH, McEwan CM. Total aneuploidy and age-related sex chromosome aneuploidy in cultured lymphocytes of normal men and women. Hum Genet. 1977; 39:329–337.24. Guttenbach M, Schakowski R, Schmid M. Aneuploidy and ageing: sex chromosome exclusion into micronuclei. Hum Genet. 1994; 94:295–298.25. Brothman AR, Maxwell TM, Cui J, Deubler DA, Zhu XL. Chromosomal clues to the development of prostate tumors. Prostate. 1999; 38:303–312.26. Christensen GB, Baffoe-Bonnie AB, George A, Powell I, Bailey-Wilson JE, Carpten JD, et al. Genome-wide linkage analysis of 1,233 prostate cancer pedigrees from the International Consortium for Prostate Cancer Genetics using novel sumLINK and sumLOD analyses. Prostate. 2010; 70:735–744.27. Sun J, Zheng SL, Wiklund F, Isaacs SD, Li G, Wiley KE, et al. Sequence variants at 22q13 are associated with prostate cancer risk. Cancer Res. 2009; 69:10–15.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Prominently Large Glans penis as a Possible sign of Benign Prostatic Hyperplasia
- Review of Chromosomal Analyses Performed in a Single Hospital
- The Effects of Abdominal Obesity on the Increased Prevalence Rate of Hypertension and Diabetes Mellitus in Benign Prostatic Hyperplasia Patients
- The influence of age and endocrine factors on the volume of benign prostatic hyperplasia
- Juvenile Benign Prostatic Hyperplasia: A Case Report