Investig Clin Urol.
2016 Jan;57(1):3-13. 10.4111/icu.2016.57.1.3.
The artificial urinary sphincter and male sling for postprostatectomy incontinence: Which patient should get which procedure?
- Affiliations
-
- 1Department of Urology, Stanford University School of Medicine, Stanford, CA, USA. ccomiter@stanford.edu
- KMID: 2363119
- DOI: http://doi.org/10.4111/icu.2016.57.1.3
Abstract
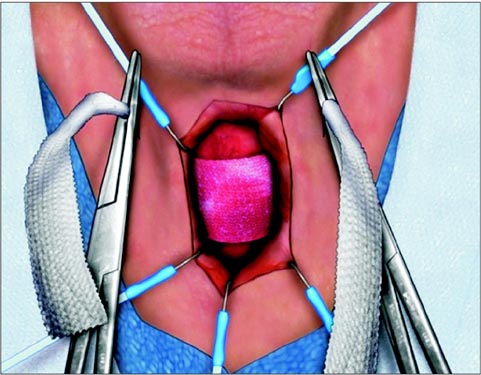
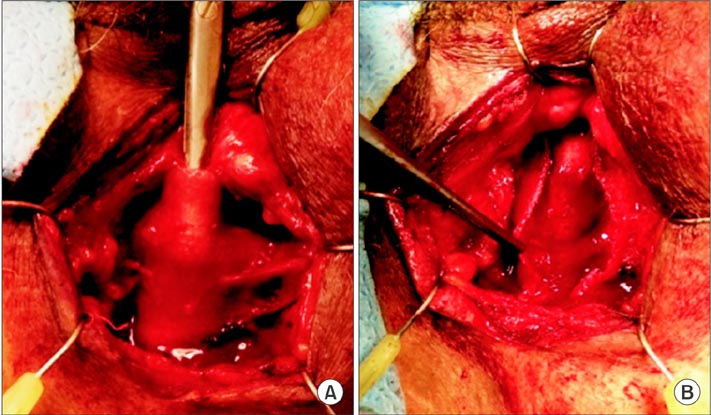
- Surgery is the most efficacious treatment for postprostatectomy incontinence. The ideal surgical approach depends on a variety of patient factors including history of prior incontinence surgery or radiation treatment, bladder contractility, severity of leakage, and patient expectations. Most patients choose to avoid a mechanical device, opting for the male sling over the artificial urinary sphincter. The modern male sling has continued to evolve with respect to device design and surgical technique. Various types of slings address sphincteric incompetence via different mechanisms of action. The recommended surgery, however, must be individualized to the patient based on degree of incontinence, detrusor contractility, and urethral compliance. A thorough urodynamic evaluation is indicated for the majority of patients, and the recommendation for an artificial urinary sphincter, a transobturator sling, or a quadratic sling will depend on urodynamic findings and the patient's particular preference. As advancements in this field evolve, and our understanding of the pathophysiology of incontinence and mechanisms of various devices improves, we expect to see continued evolution in device design.
Keyword
MeSH Terms
Figure
Reference
-
1. Nam RK, Herschorn S, Loblaw DA, Liu Y, Klotz LH, Carr LK, et al. Population based study of long-term rates of surgery for urinary incontinence after radical prostatectomy for prostate cancer. J Urol. 2012; 188:502–506.2. Chughtai B, Sedrakyan A, Isaacs AJ, Mao J, Lee R, Te A, et al. National study of utilization of male incontinence procedures. Neurourol Urodyn. 2014; 10. 18. [Epub]. DOI: 10.1002/nau.22683.3. Herschorn S, Bruschini H, Comiter C, Grise P, Hanus T, Kirschner-Hermanns R, et al. Surgical treatment of stress incontinence in men. Neurourol Urodyn. 2010; 29:179–190.4. Lai HH, Hsu EI, Teh BS, Butler EB, Boone TB. 13 years of experience with artificial urinary sphincter implantation at Baylor College of Medicine. J Urol. 2007; 177:1021–1025.5. Comiter CV. Surgery Insight: surgical management of postprostatectomy incontinence: the artificial urinary sphincter and male sling. Nat Clin Pract Urol. 2007; 4:615–624.6. Kumar A, Litt ER, Ballert KN, Nitti VW. Artificial urinary sphincter versus male sling for post-prostatectomy incontinence: what do patients choose? J Urol. 2009; 181:1231–1235.7. Stern JA, Clemens JQ, Tiplitsky SI, Matschke HM, Jain PM, Schaeffer AJ. Long-term results of the bulbourethral sling procedure. J Urol. 2005; 173:1654–1656.8. Welk BK, Herschorn S. The male sling for post-prostatectomy urinary incontinence: a review of contemporary sling designs and outcomes. BJU Int. 2012; 109:328–344.9. Rehder P, Berger T, Kiss G, Madersbacher H, Gozzi C. Advance male sling: anatomic evidence of retrourethral position after tensioning without direct urethral compression. Eur Urol Suppl. 2008; 7:87.10. Comiter CV, Nitti V, Elliot C, Rhee E. A new quadratic sling for male stress incontinence: retrograde leak point pressure as a measure of urethral resistance. J Urol. 2012; 187:563–568.11. Hubner WA, Gallistl H, Rutkowski M, Huber ER. Adjustable bulbourethral male sling: experience after 101 cases of moderate-to-severe male stress urinary incontinence. BJU Int. 2011; 107:777–782.12. Sousa-Escandon A, Cabrera J, Mantovani F, Moretti M, Ioanidis E, Kondelidis N, et al. Adjustable suburethral sling (male remeex system) in the treatment of male stress urinary incontinence: a multicentric European study. Eur Urol. 2007; 52:1473–1479.13. Kao TC, Cruess DF, Garner D, Foley J, Seay T, Friedrichs P, et al. Multicenter patient self-reporting questionnaire on impotence, incontinence and stricture after radical prostatectomy. J Urol. 2000; 163:858–864.14. Kundu SD, Roehl KA, Eggener SE, Antenor JA, Han M, Catalona WJ. Potency, continence and complications in 3,477 consecutive radical retropubic prostatectomies. J Urol. 2004; 172(6 Pt 1):2227–2231.15. Twiss C, Fleischmann N, Nitti VW. Correlation of abdominal leak point pressure with objective incontinence severity in men with post-radical prostatectomy stress incontinence. Neurourol Urodyn. 2005; 24:207–210.16. Nitti VW, Mourtzinos A, Brucker BM. SUFU Pad Test Study Group. Correlation of patient perception of pad use with objective degree of incontinence measured by pad test in men with post-prostatectomy incontinence: the SUFU Pad Test Study. J Urol. 2014; 192:836–842.17. Giannantoni A, Mearini E, Zucchi A, Costantini E, Mearini L, Bini V, et al. Bladder and urethral sphincter function after radical retropubic prostatectomy: a prospective long-term study. Eur Urol. 2008; 54:657–664.18. Lai HH, Hsu EI, Boone TB. Urodynamic testing in evaluation of postradical prostatectomy incontinence before artificial urinary sphincter implantation. Urology. 2009; 73:1264–1269.19. Afraa TA, Campeau L, Mahfouz W, Corcos J. Urodynamic parameters evolution after artificial urinary sphincter implantation for post-radical prostatectomy incontinence with concomitant bladder dysfunction. Can J Urol. 2011; 18:5695–5698.20. Giannantoni A, Mearini E, Di Stasi SM, Mearini L, Bini V, Pizzirusso G, et al. Assessment of bladder and urethral sphincter function before and after radical retropubic prostatectomy. J Urol. 2004; 171:1563–1566.21. Matsukawa Y, Hattori R, Komatsu T, Funahashi Y, Sassa N, Gotoh M. De novo detrusor underactivity after laparoscopic radical prostatectomy. Int J Urol. 2010; 17:643–648.22. Trigo Rocha F, Gomes CM, Mitre AI, Arap S, Srougi M. A prospective study evaluating the efficacy of the artificial sphincter AMS 800 for the treatment of postradical prostatectomy urinary incontinence and the correlation between preoperative urodynamic and surgical outcomes. Urology. 2008; 71:85–89.23. Elliott CS, Comiter CV. Maximum isometric detrusor pressure to measure bladder strength in men with postprostatectomy incontinence. Urology. 2012; 80:1111–1115.24. Griffiths D. Detrusor contractility: order out of chaos. Scand J Urol Nephrol Suppl. 2004; (215):93–100.25. Sullivan MP, DuBeau CE, Resnick NM, Cravalho EG, Yalla SV. Continuous occlusion test to determine detrusor contractile performance. J Urol. 1995; 154:1834–1840.26. McIntosh SL, Griffiths CJ, Drinnan MJ, Robson WA, Ramsden PD, Pickard RS. Noninvasive measurement of bladder pressure. Does mechanical interruption of the urinary stream inhibit detrusor contraction? J Urol. 2003; 169:1003–1006.27. Bauer RM, Mayer ME, Gratzke C, Soljanik I, Buchner A, Bastian PJ, et al. Prospective evaluation of the functional sling suspension for male postprostatectomy stress urinary incontinence: results after 1 year. Eur Urol. 2009; 56:928–933.28. Rehder P, Freiin von Gleissenthall G, Pichler R, Glodny B. The treatment of postprostatectomy incontinence with the retroluminal transobturator repositioning sling (Advance): lessons learnt from accumulative experience. Arch Esp Urol. 2009; 62:860–870.29. Soljanik I, Gozzi C, Becker AJ, Stief CG, Bauer RM. Risk factors of treatment failure after retrourethral transobturator male sling. World J Urol. 2012; 30:201–206.30. Bauer RM, Gozzi C, Roosen A, Khoder W, Trottmann M, Waidelich R, et al. Impact of the repositioning test on postoperative outcome of retroluminar transobturator male sling implantation. Urol Int. 2013; 90:334–338.31. Comiter C, Payne C, Vecchiotti R. Abstract 2160: A prospective analysis of video-urodynamic data to measure urethral mobility in men with post-prostatectomy incontinence. J Urol. 2011; 185:4 Suppl. e864–e865. Abstract No. 216032. Kim SP, Sarmast Z, Daignault S, Faerber GJ, McGuire EJ, Latini JM. Long-term durability and functional outcomes among patients with artificial urinary sphincters: a 10-year retrospective review from the University of Michigan. J Urol. 2008; 179:1912–1916.33. Comiter CV. The male perineal sling: intermediate-term results. Neurourol Urodyn. 2005; 24:648–653.34. Carmel M, Hage B, Hanna S, Schmutz G, Tu le M. Long-term efficacy of the bone-anchored male sling for moderate and severe stress urinary incontinence. BJU Int. 2010; 106:1012–1016.35. De Ridder D, Rehder P. The advance male sling: anatomic features in relation to mode of action. Eur Urol Suppl. 2011; 10:383–389.36. Rehder P, Haab F, Cornu JN, Gozzi C, Bauer RM. Treatment of postprostatectomy male urinary incontinence with the transobturator retroluminal repositioning sling suspension: 3-year follow-up. Eur Urol. 2012; 62:140–145.37. Zuckerman JM, Edwards B, Henderson K, Beydoun HA, Mc-Cammon KA. Extended outcomes in the treatment of male stress urinary incontinence with a transobturator sling. Urology. 2014; 83:939–945.38. Osman NI. Slings in the management of male stress urinary incontinence. Curr Opin Urol. 2013; 23:528–535.39. Rehder P, Mitterberger MJ, Pichler R, Kerschbaumer A, Glodny B. The 1 year outcome of the transobturator retroluminal repositioning sling in the treatment of male stress urinary incontinence. BJU Int. 2010; 106:1668–1672.40. Cornu JN, Sebe P, Ciofu C, Peyrat L, Cussenot O, Haab F. Mid-term evaluation of the transobturator male sling for post-prostatectomy incontinence: focus on prognostic factors. BJU Int. 2011; 108:236–240.41. Bauer RM, Mayer ME, May F, Gratzke C, Buchner A, Soljanik I, et al. Complications of the AdVance transobturator male sling in the treatment of male stress urinary incontinence. Urology. 2010; 75:1494–1498.42. Comiter CV, Rhee EY. The 'ventral urethral elevation plus' sling: a novel approach to treating stress urinary incontinence in men. BJU Int. 2008; 101:187–191.43. Comiter CV, Rhee EY, Tu LM, Herschorn S, Nitti VW. The virtue sling--a new quadratic sling for postprostatectomy incontinence--results of a multinational clinical trial. Urology. 2014; 84:433–438.44. Bauer RM, Rutkowski M, Kretschmer A, Casuscelli J, Stief CG, Huebner W, et al. Efficacy and complications of the adjustable sling system ArgusT for male incontinence: results of a prospective 2-center study. Urology. 2015; 85:316–320.45. Trost L, Elliott DS. Male stress urinary incontinence: a review of surgical treatment options and outcomes. Adv Urol. 2012; 2012:287489.46. Chung E, Smith P, Malone G, Cartmill R. Adjustable versus non-adjustable male sling for post-prostatectomy urinary incontinence: a prospective clinical trial comparing patient choice, clinical outcomes and satisfaction rate with a minimum follow up of 24 months. Neurourol Urodyn. 2015; 02. 14. [Epub]. DOI: 10.1002/nau.22731.47. Jimenez Parra JD, Cebrian Lostal JL, Hualde Alfaro A, Alvarez Bandres S, Garcia García D, Torres Varas L, et al. REMEEX® system for the treatment of male urinary stress incontinence: our experience. Actas Urol Esp. 2010; 34:802–805.48. Comiter CV, Sullivan MP, Yalla SV. Retrograde leak point pressure for evaluating postradical prostatectomy incontinence. Urology. 1997; 49:231–236.49. Bamshad BR, Hadley HR, Ruckle HC, Lui PD. Perfusion sphincterometry for objective evaluation of postprostatectomy intrinsic sphincter deficiency. Urology. 1999; 53:968–973.50. Comiter CV, Sullivan MP, Yalla SV. Correlation among maximal urethral closure pressure, retrograde leak point pressure, and abdominal leak point pressure in men with postprostatectomy stress incontinence. Urology. 2003; 62:75–78.51. Choe JM, Battino BS, Bell TE. Retrograde perfusion sphincterometry with a flexible cystoscope: method of troubleshooting the AMS 800. Urology. 2000; 56:317–319.52. Ullrich NF, Comiter CV. The male sling for stress urinary incontinence: urodynamic and subjective assessment. J Urol. 2004; 172:204–206.53. Samli M, Singla AK. Absorbable versus nonabsorbable graft: outcome of bone anchored male sling for post-radical prostatectomy incontinence. J Urol. 2005; 173:499–502.54. Giberti C, Gallo F, Schenone M, Cortese P, Ninotta G. The bone anchor suburethral synthetic sling for iatrogenic male incontinence: critical evaluation at a mean 3-year followup. J Urol. 2009; 181:2204–2208.55. Li H, Gill BC, Nowacki AS, Montague DK, Angermeier KW, Wood HM, et al. Therapeutic durability of the male transobturator sling: midterm patient reported outcomes. J Urol. 2012; 187:1331–1335.56. Collado Serra A, Resel Folkersma L, Domínguez-Escrig JL, Gomez-Ferrer A, Rubio-Briones J, Solsona Narbon E. AdVance/AdVance XP transobturator male slings: preoperative degree of incontinence as predictor of surgical outcome. Urology. 2013; 81:1034–1039.57. Anderson CA, Omar MI, Campbell SE, Hunter KF, Cody JD, Glazener CM. Conservative management for postprostatectomy urinary incontinence. Cochrane Database Syst Rev. 2015; 1:CD001843.58. Lepor H, Kaci L. The impact of open radical retropubic prostatectomy on continence and lower urinary tract symptoms: a prospective assessment using validated self-administered outcome instruments. J Urol. 2004; 171:1216–1219.59. Cornu JN, Sebe P, Ciofu C, Peyrat L, Beley S, Tligui M, et al. The AdVance transobturator male sling for postprostatectomy incontinence: clinical results of a prospective evaluation after a minimum follow-up of 6 months. Eur Urol. 2009; 56:923–927.60. Bauer RM, Soljanik I, Fullhase C, Karl A, Becker A, Stief CG, et al. Mid-term results for the retroluminar transobturator sling suspension for stress urinary incontinence after prostatectomy. BJU Int. 2011; 108:94–98.61. Fischer MC, Huckabay C, Nitti VW. The male perineal sling: assessment and prediction of outcome. J Urol. 2007; 177:1414–1418.62. Castle EP, Andrews PE, Itano N, Novicki DE, Swanson SK, Ferrigni RG. The male sling for post-prostatectomy incontinence: mean followup of 18 months. J Urol. 2005; 173:1657–1660.63. Schaeffer AJ, Clemens JQ, Ferrari M, Stamey TA. The male bulbourethral sling procedure for post-radical prostatectomy incontinence. J Urol. 1998; 159:1510–1515.64. Torrey R, Rajeshuni N, Ruel N, Muldrew S, Chan K. Radiation history affects continence outcomes after advance transobturator sling placement in patients with post-prostatectomy incontinence. Urology. 2013; 82:713–717.65. Tuygun C, Imamoglu A, Gucuk A, Goktug G, Demirel F. Comparison of outcomes for adjustable bulbourethral male sling and artificial urinary sphincter after previous artificial urinary sphincter erosion. Urology. 2009; 73:1363–1367.66. Margreiter M, Farr A, Sharma V, Schauer I, Klingler HC. Urethral buttressing in patients undergoing artificial urinary sphincter surgery. J Urol. 2013; 189:1777–1781.67. Guralnick ML, Miller E, Toh KL, Webster GD. Transcorporal artificial urinary sphincter cuff placement in cases requiring revision for erosion and urethral atrophy. J Urol. 2002; 167:2075–2078.68. Trost L, Elliott D. Small intestinal submucosa urethral wrap at the time of artificial urinary sphincter placement as a salvage treatment option for patients with persistent/recurrent incontinence following multiple prior sphincter failures and erosions. Urology. 2012; 79:933–938.69. Wang R, McGuire EJ, He C, Faerber GJ, Latini JM. Long-term outcomes after primary failures of artificial urinary sphincter implantation. Urology. 2012; 79:922–928.70. Martinez EJ, Zuckerman JM, Henderson K, Edwards B, Mc-Cammon K. Evaluation of salvage male transobturator sling placement following recurrent stress urinary incontinence after failed transobturator sling. Urology. 2015; 85:478–482.71. Soljanik I, Becker AJ, Stief CG, Gozzi C, Bauer RM. Repeat retrourethral transobturator sling in the management of recurrent postprostatectomy stress urinary incontinence after failed first male sling. Eur Urol. 2010; 58:767–772.72. Ajay D, Zhang H, Gupta S, Selph JP, Belsante MJ, Lentz AC, et al. The artificial urinary sphincter is superior to a secondary transobturator male sling in cases of a primary sling failure. J Urol. 2015; 194:1038–1042.73. Kim PH, Pinheiro LC, Atoria CL, Eastham JA, Sandhu JS, Elkin EB. Trends in the use of incontinence procedures after radical prostatectomy: a population based analysis. J Urol. 2013; 189:602–608.74. Belot PY, Fassi-Fehri H, Crouzet S, Codas R, Badet L, Gelet A, et al. Treatment of stress urinary incontinence after prostate surgery: results of the artificial urinary sphincter after suburethral sling failure. Prog Urol. 2012; 22:644–649.75. Romano SV, Metrebian SE, Vaz F, Muller V, D'Ancona CA, de Souza EA, et al. Long-term results of a phase III multicentre trial of the adjustable male sling for treating urinary incontinence after prostatectomy: minimum 3 years. Actas Urol Esp. 2009; 33:309–314.76. Abdou A, Cornu JN, Sebe P, Ciofu C, Peyrat L, Cussenot O, et al. Salvage therapy with artificial urinary sphincter after Advance™ male sling failure for post-prostatectomy incontinence: a first clinical experience. Prog Urol. 2012; 22:650–656.77. Lentz AC, Peterson AC, Webster GD. Outcomes following artificial sphincter implantation after prior unsuccessful male sling. J Urol. 2012; 187:2149–2153.78. Staskin DR, Comiter CV. Surgical treatment of male sphincteric urinary incontinence: the male perineal sling and artificial urinary sphincter. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders;2007. p. 2391–2404.79. Comiter C. Surgery for postprostatectomy incontinence: which procedure for which patient? Nat Rev Urol. 2015; 12:91–99.80. Al-Najar A, Kaufmann S, Boy S, Naumann CM, Junemann PK, Van Der Horst C. Management of recurrent post-prostatectomy incontinence after previous failed retrourethral male slings. Can Urol Assoc J. 2011; 5:107–111.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sling Surgery for Male Urinary Incontinence Including Post Prostatectomy Incontinence: A Challenge to the Urologist
- Artificial Urinary Sphincter for Postradical Prostatectomy Urinary Incontinence — Is It the Best Option?
- Initial 4 Cases Experience of Male Sling Procedure for the Treatment in Patients with Post-prostatectomy Incontinence
- The Current Role of the Artificial Urinary Sphincter in Male and Female Urinary Incontinence
- Intercavernous Embedding of Bulboperineal Urethra for Postprostatectomy Incontinence: Report of a Case