Ann Hepatobiliary Pancreat Surg.
2016 Nov;20(4):204-210. 10.14701/ahbps.2016.20.4.204.
Pseudoaneurysm of the splenic artery - an uncommon cause of delayed hemorrhage after pancreaticoduodenectomy
- Affiliations
-
- 1Center of Interventional Radiology and Medical Imaging, Fundeni Clinical Institute, Bucharest, Romania.
- 2Center of General Surgery and Liver Transplant, Fundeni Clinical Institute, Bucharest, Romania. traian.dumitrascu76@gmail.com
- KMID: 2362473
- DOI: http://doi.org/10.14701/ahbps.2016.20.4.204
Abstract
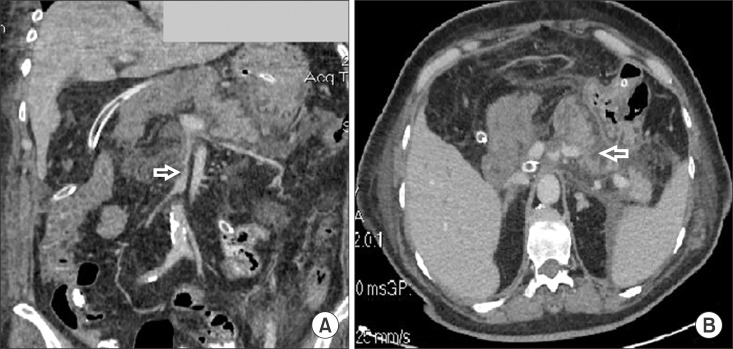
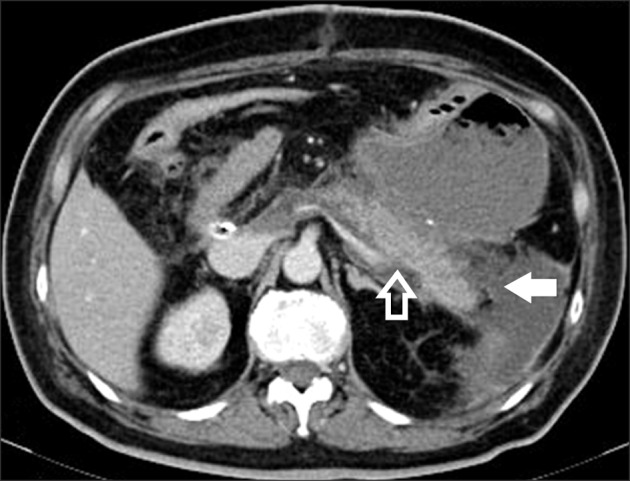
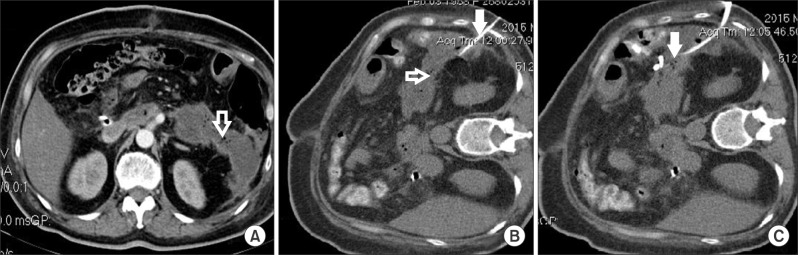
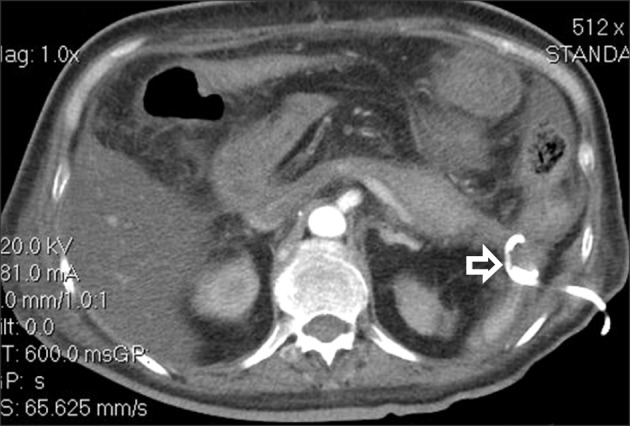
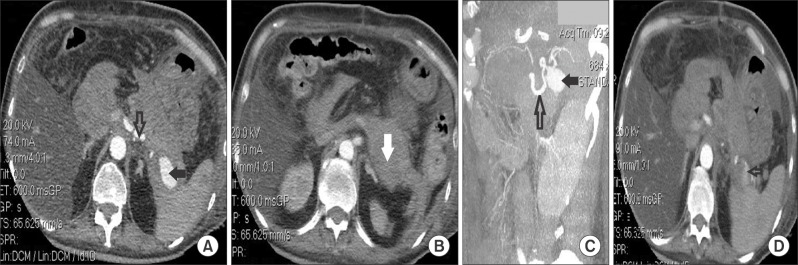
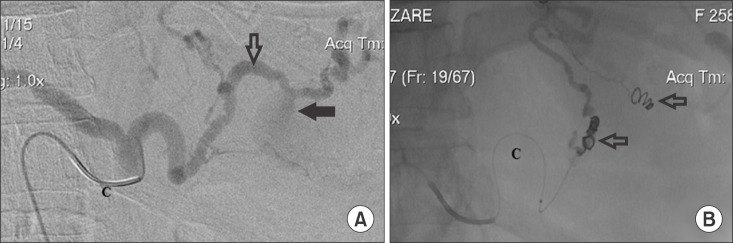
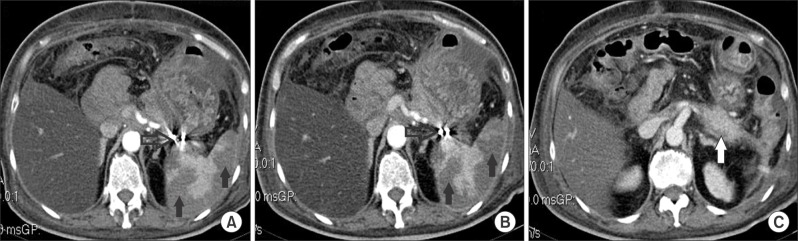
- Delayed post-pancreatectomy hemorrhage (PPH) is a relatively uncommon, but feared, complication after pancreaticoduodenectomy (PD). A splenic artery pseudoaneurysm is a rare cause of delayed PPH after a PD. This paper describes the case of a patient with PD used to treat a distal bile duct cholangiocarcinoma complicated with a clinically significant pancreatic fistula and secondary intraabdominal abscess. Computed tomography-guided drainage of the abscess was performed with an apparently favourable outcome; the patient was discharged on postoperative day (POD) 35 and the abdominal drains were removed on POD 50. On POD 80, the patient was readmitted for a severe digestive hemorrhage. Computed tomography revealed a pseudoaneurysm of the splenic artery with a subsequent hematoma formation. Immediately, an angiography was performed and coils were successfully mounted. This case illustrates the rare possibility of the development of a splenic artery pseudoaneurysm with severe delayed PPH after PD complicated with a clinically significant pancreatic fistula, even after the patient was discharged from the hospital. An interventional radiology approach represents the first treatment option in hemodynamically stable patients with high success rates.
Keyword
MeSH Terms
Figure
Reference
-
1. Popescu I, Dumitraşcu T. Pancreatoduodenectomy--past, present and future. Chirurgia (Bucur). 2011; 106:287–296. PMID: 21853734.2. Dumitrascu T, Dima S, Brasoveanu V, Stroescu C, Herlea V, Moldovan S, et al. Impact of a portal/superior mesenteric vein resection during pancreatico-duodenectomy for pancreatic head adenocarcinoma. Minerva Chir. 2014; 69:301–313. PMID: 25493393.3. Schmidt CM, Turrini O, Parikh P, House MG, Zyromski NJ, Nakeeb A, et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Arch Surg. 2010; 145:634–640. PMID: 20644125.4. Gooiker GA, van Gijn W, Wouters MW, Post PN, van de Velde CJ, Tollenaar RA. Signalling Committee Cancer of the Dutch Cancer Society. Systematic review and meta-analysis of the volume-outcome relationship in pancreatic surgery. Br J Surg. 2011; 98:485–494. PMID: 21500187.
Article5. Swanson RS, Pezzi CM, Mallin K, Loomis AM, Winchester DP. The 90-day mortality after pancreatectomy for cancer is double the 30-day mortality: more than 20,000 resections from the national cancer data base. Ann Surg Oncol. 2014; 21:4059–4067. PMID: 25190121.
Article6. Mathur A, Luberice K, Ross S, Choung E, Rosemurgy A. Pancreaticoduodenectomy at high-volume centers: surgeon volume goes beyond the Leapfrog criteria. Ann Surg. 2015; 262:e37–e39. PMID: 26164432.7. Cameron JL, He J. Two thousand consecutive pancreaticoduodenectomies. J Am Coll Surg. 2015; 220:530–536. PMID: 25724606.
Article8. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13. PMID: 16003309.
Article9. Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007; 142:20–25. PMID: 17629996.10. Ansari D, Tingstedt B, Lindell G, Keussen I, Ansari D, Andersson R. Hemorrhage after major pancreatic resection: incidence, risk factors, management, and outcome. Scand J Surg. 2016; pii: 1457496916631854. [in press].
Article11. Asai K, Zaydfudim V, Truty M, Reid-Lombardo KM, Kendrick M, Que F, et al. Management of a delayed post-pancreatoduodenectomy haemorrhage using endovascular techniques. HPB (Oxford). 2015; 17:902–908. PMID: 26235930.12. Correa-Gallego C, Brennan MF, D'Angelica MI, DeMatteo RP, Fong Y, Kingham TP, et al. Contemporary experience with postpancreatectomy hemorrhage: results of 1,122 patients resected between 2006 and 2011. J Am Coll Surg. 2012; 215:616–621. PMID: 22921325.
Article13. Ding X, Zhu J, Zhu M, Li C, Jian W, Jiang J, et al. Therapeutic management of hemorrhage from visceral artery pseudoaneurysms after pancreatic surgery. J Gastrointest Surg. 2011; 15:1417–1425. PMID: 21584822.
Article14. Huo Y, Chi J, Zhang J, Liu W, Liu D, Li J, et al. Endovascular intervention for delayed post-pancreaticoduodenectomy hemorrhage: clinical features and outcomes of transcatheter arterial embolization and covered stent placement. Int J Clin Exp Med. 2015; 8:7457–7466. PMID: 26221289.15. Jilesen AP, Tol JA, Busch OR, van Delden OM, van Gulik TM, Nieveen van Dijkum EJ, et al. Emergency management in patients with late hemorrhage after pancreatoduodenectomy for a periampullary tumor. World J Surg. 2014; 38:2438–2447. PMID: 24791669.
Article16. Lee HG, Heo JS, Choi SH, Choi DW. Management of bleeding from pseudoaneurysms following pancreaticoduodenectomy. World J Gastroenterol. 2010; 16:1239–1244. PMID: 20222168.
Article17. Roulin D, Cerantola Y, Demartines N, Schäfer M. Systematic review of delayed postoperative hemorrhage after pancreatic resection. J Gastrointest Surg. 2011; 15:1055–1062. PMID: 21267670.
Article18. Wellner UF, Kulemann B, Lapshyn H, Hoeppner J, Sick O, Makowiec F, et al. Postpancreatectomy hemorrhage--incidence, treatment, and risk factors in over 1,000 pancreatic resections. J Gastrointest Surg. 2014; 18:464–475. PMID: 24448997.
Article19. Ching KC, Santos E, McCluskey KM, Orons PD, Bandi R, Friend CJ, et al. Covered stents and coil embolization for treatment of postpancreatectomy arterial hemorrhage. J Vasc Interv Radiol. 2016; 27:73–79. PMID: 26611883.
Article20. Camerlo A, Turrini O, Marciano S, Sarran A, Berdah S, Delpero JR, et al. Delayed arterial hemorrhage after pancreaticoduodenectomy: is conservation of hepatic arterial flow vital? Pancreas. 2010; 39:260–262. PMID: 20182313.21. Yekebas EF, Wolfram L, Cataldegirmen G, Habermann CR, Bogoevski D, Koenig AM, et al. Postpancreatectomy hemorrhage: diagnosis and treatment: an analysis in 1669 consecutive pancreatic resections. Ann Surg. 2007; 246:269–280. PMID: 17667506.22. Tien YW, Lee PH, Yang CY, Ho MC, Chiu YF. Risk factors of massive bleeding related to pancreatic leak after pancreaticoduodenectomy. J Am Coll Surg. 2005; 201:554–559. PMID: 16183493.
Article23. Agrawal GA, Johnson PT, Fishman EK. Splenic artery aneurysms and pseudoaneurysms: clinical distinctions and CT appearances. AJR Am J Roentgenol. 2007; 188:992–999. PMID: 17377035.
Article24. Cazejust J, Raynal M, Bessoud B, Tubiana JM, Menu Y. Diagnosis and radiological treatment of digestive haemorrhage following supramesocolic surgery. Diagn Interv Imaging. 2012; 93:e148–e158. PMID: 22421279.
Article25. Darnis B, Lebeau R, Chopin-Laly X, Adham M. Postpancreatectomy hemorrhage (PPH): predictors and management from a prospective database. Langenbecks Arch Surg. 2013; 398:441–448. PMID: 23435636.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Splenic Artery Pseudoaneurysm Complicating Chronic Pancreatitis: A Case Report
- Management of a Bleeding Pseudoaneurysm after Pancreaticoduodenectomy: 27 cases experience in single-center
- Renal Artery Pseudoaneurysm after Blunt Renal Trauma
- Delayed Hemorrhage from Gastroduodenal Artery Pseudoaneurysm following Endoscopic Ultrasound-Guided Fine Needle Aspiration of Pancreatic Head Mass
- Hepatic artery pseudoaneurysm after pancreaticoduodenectomy treated with coil embolization in combination with portomesenteric venous stenting