Investig Clin Urol.
2016 Dec;57(Suppl 2):S165-S171. 10.4111/icu.2016.57.S2.S165.
Standardized 4-step technique of bladder neck dissection during robot-assisted radical prostatectomy
- Affiliations
-
- 1Section of Urology, Department of Surgery, Centre Hospitalier de l'Université de Montréal, Montréal, QC, Canada. dr.mansouralnazari@gmail.com
- KMID: 2361682
- DOI: http://doi.org/10.4111/icu.2016.57.S2.S165
Abstract
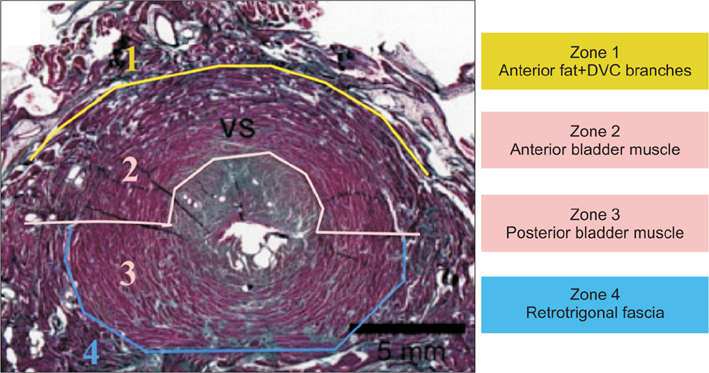
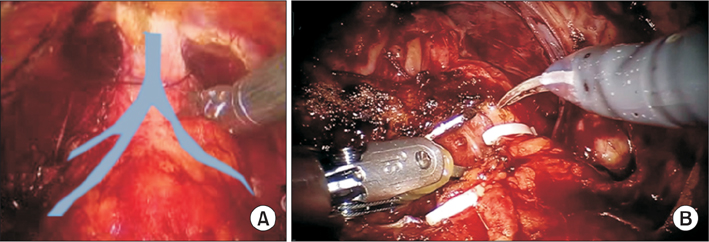
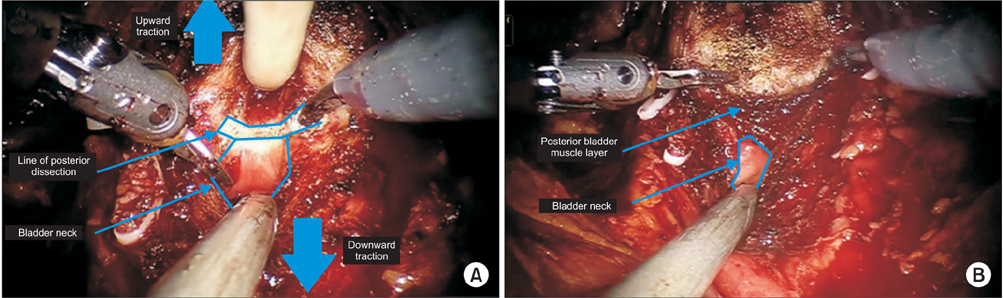
- Bladder neck (BN) dissection is considered one of the most challenging steps during robot-assisted radical prostatectomy. Better understanding of the BN anatomy, coupled with a standardized approach may facilitate dissection while minimizing complications. We describe in this article the 4 anatomic spaces during standardized BN dissection, as well other technical maneuvers of managing difficult scenarios including treatment of a large median lobe or patients with previous transurethral resection of the prostate. The first step involves the proper identification of the BN followed by slow horizontal dissection of the first layer (the dorsal venous complex and perivesicle fat). The second step proceeds with reconfirming the location of the BN followed by midline dissection of the second anatomical layer (the anterior bladder muscle and mucosa) using the tip of the monopolar scissor until the catheter is identified. The deflated catheter is then grasped by the assistant to apply upward traction on the prostate from 2 directions along with downward traction on the posterior bladder wall by the tip of the suction instrument. This triangulation allows easier, and safer visual, layer by layer, dissection of the third BN layer (the posterior bladder mucosa and muscle wall). The forth step is next performed by blunt puncture of the fourth layer (the retrotrigonal fascia) aiming to enter into the previously dissected seminal vesical space. Finally, both vas deferens and seminal vesicles are pulled through the open BN and handed to the assistant for upper traction to initiate Denovillier's dissection and prostate pedicle/neurovascular bundle control.
MeSH Terms
Figure
Reference
-
1. Hu JC, Gu X, Lipsitz SR, Barry MJ, D'Amico AV, Weinberg AC, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA. 2009; 302:1557–1564.2. Berryhill R Jr, Jhaveri J, Yadav R, Leung R, Rao S, El-Hakim A, et al. Robotic prostatectomy: a review of outcomes compared with laparoscopic and open approaches. Urology. 2008; 72:15–23.3. Tholomier C, Bienz M, Hueber PA, Trinh QD, Hakim AE, Alhathal N, et al. Oncological and functional outcomes of 722 robot-assisted radical prostatectomy (RARP) cases: The largest Canadian 5-year experience. Can Urol Assoc J. 2014; 8:195–201.4. Piechaud T, Annino F. Bladder neck dissection during robotic-assisted laparoscopic radical prostatectomy. In : John H, Wiklund P, editors. Robotic urology. Berlin: Springer;2013. p. 247–258.5. Walsh PC, Retik AB, Vaughan ED, editors. Campbell's urology. 8th ed. St. Louis: Elsevier;2003.6. Tewari A, El-Hakim A, Rao S, Raman JD. Identification of the retrotrigonal layer as a key anatomical landmark during robotically assisted radical prostatectomy. BJU Int. 2006; 98:829–832.7. Valdivieso RF, Hueber PA, Zorn KC. Robot assisted radical prostatectomy: how I do it. Part II: Surgical technique. Can J Urol. 2013; 20:7073–7078.8. Valdivieso RF, Hueber PA, Zorn KC. Robot assisted radical prostatectomy: how I do it. Part I: Patient preparation and positioning. Can J Urol. 2013; 20:6957–6961.9. Alenizi AM, Valdivieso R, Rajih E, Meskawi M, Toarta C, Bienz M, et al. Factors predicting prolonged operative time for individual surgical steps of robot-assisted radical prostatectomy (RARP): a single surgeon's experience. Can Urol Assoc J. 2015; 9:E417–E422.10. Katz MH, Eng MK, Deklaj T, Zorn KC. Technique for ureteral stent placement during robot-assisted radical prostatectomy: safety measure during vesicourethral anastomosis when ureteral orifices are too close for comfort. J Endourol. 2009; 23:827–829.11. Gupta NP, Singh P, Nayyar R. Outcomes of robot-assisted radical prostatectomy in men with previous transurethral resection of prostate. BJU Int. 2011; 108:1501–1505.12. Stolzenburg JU, Schwalenberg T, Horn LC, Neuhaus J, Constantinides C, Liatsikos EN. Anatomical landmarks of radical prostatecomy. Eur Urol. 2007; 51:629–639.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Floating Hem-o-Lok Clips in the Bladder without Stone Formation after Robot-Assisted Laparoscopic Radical Prostatectomy
- Erratum: Robot-Assisted Laparoscopic Radical Prostatectomy
- The Effectiveness of Cystography-Measured Bladder Neck Elevation at Predicting the Return of Continence After Robot-Assisted Radical Prostatectomy
- Infected Lymphocele Extending to the Leg after Robot-Assisted Radical Prostatectomy and Pelvic Lymph Node Dissection
- Surgical Clip-Related Complications after Radical Prostatectomy