Results of Free Flap Reconstruction After Ablative Surgery in the Head and Neck
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Kyungpook National University College of Medicine, Daegu, Korea.
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. ahnsh30@snu.ac.kr
- KMID: 2360789
- DOI: http://doi.org/10.3342/ceo.2015.8.2.167
Abstract
OBJECTIVES
Due to the complex anatomy and function of the head and neck region, the reconstruction of ablative defects in this area is challenging. In addition, an increasing interest in improving the quality of life of patients and achieving good functional results has highlighted the importance of free flaps. The aim of this study was to summarize the results of free flap reconstruction and salvage of free flaps in a single institute, and to analyze differences in the results by the flap donor site, recipient site, and learning curve.
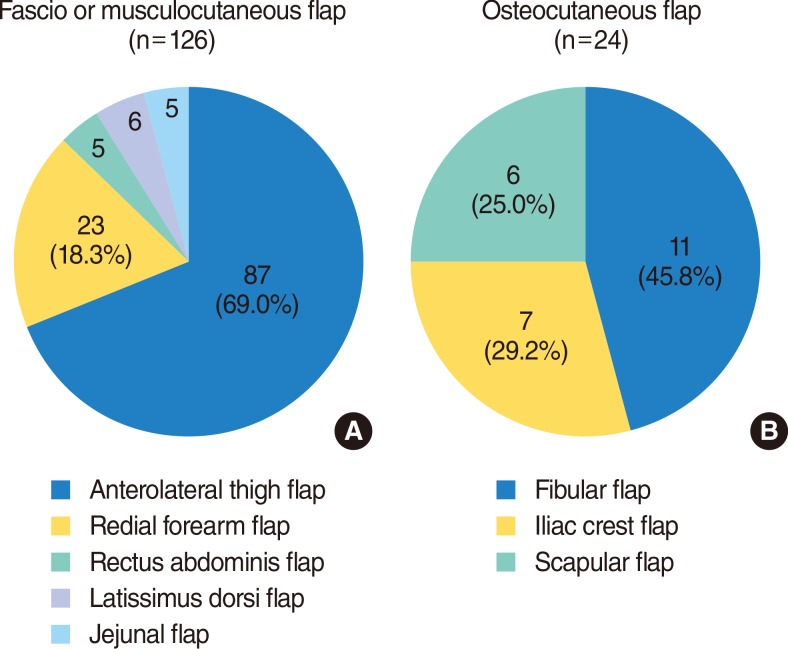
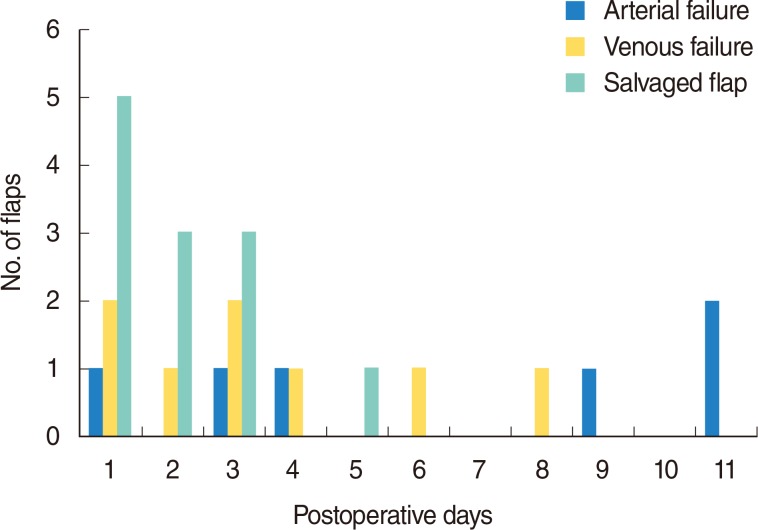
METHODS
The medical records of patients who underwent free flap reconstruction from 2004-2012 were reviewed retrospectively. One hundred and fifty free flaps were used in 134 patients, who had an average age of 57.7 years. The types of flaps applied, primary defect sites, success rates, results of salvage operations for compromised flap, and the learning curve were analyzed.
RESULTS
The anterolateral thigh flap was preferred for the reconstruction of head and neck defects. The overall success rate was 90.7%, with 14 cases of failure. A total of 19 salvage operations (12.7%) for compromised flap were performed, and 12 flaps (63.2%) were salvaged successfully. Dependency on the facial vessels as recipient vessels was statistically different when oral and oropharyngeal defects were compared to hypopharyngeal and laryngeal defects. The learning curve for microvascular surgery showed decrease in the failure rate after 50 cases.
CONCLUSION
The free flap technique is safe but involves a significant learning period and requires careful postoperative monitoring of the patient. Early intervention is important for the salvage of free flaps and for lowering the failure rate.
MeSH Terms
Figure
Cited by 3 articles
-
Testing a New Anticoagulation Method for Free Flap Reconstruction of Head and Neck Cancers
Ebrahim Karimi, Seyyed Hadi Samimi Ardestani, Mehrdad Jafari, Ali Bagheri Hagh
Clin Exp Otorhinolaryngol. 2016;9(4):370-373. doi: 10.21053/ceo.2015.01781.Externally Monitored Versus Conventional Buried Flaps in Laryngopharyngeal Reconstruction
Myung Jin Ban, Gina Na, Sungchul Ko, Joohyun Kim, Nam Hun Heo, Eun Chang Choi, Jae Hong Park, Won Shik Kim
Clin Exp Otorhinolaryngol. 2021;14(4):407-413. doi: 10.21053/ceo.2020.00234.Cumulative Sum Analysis of the Learning Curve of Free Flap Reconstruction in Head and Neck Cancer Patients
Seung Hoon Han, Young Chul Kim, Tack-Kyun Kwon, Doh Young Lee
Clin Exp Otorhinolaryngol. 2022;15(2):177-182. doi: 10.21053/ceo.2021.01053.
Reference
-
1. Urken ML, Weinberg H, Buchbinder D, Moscoso JF, Lawson W, Catalano PJ, et al. Microvascular free flaps in head and neck reconstruction: Report of 200 cases and review of complications. Arch Otolaryngol Head Neck Surg. 1994; 6. 120(6):633–640. PMID: 8198786.
Article2. Kroll SS, Schusterman MA, Reece GP, Miller MJ, Evans GR, Robb GL, et al. Choice of flap and incidence of free flap success. Plast Reconstr Surg. 1996; 9. 98(3):459–463. PMID: 8700982.
Article3. Nakatsuka T, Harii K, Asato H, Takushima A, Ebihara S, Kimata Y, et al. Analytic review of 2372 free flap transfers for head and neck reconstruction following cancer resection. J Reconstr Microsurg. 2003; 8. 19(6):363–368. PMID: 14515225.
Article4. Nahabedian MY, Singh N, Deune EG, Silverman R, Tufaro AP. Recipient vessel analysis for microvascular reconstruction of the head and neck. Ann Plast Surg. 2004; 2. 52(2):148–155. PMID: 14745264.
Article5. Suominen S, Ahovuo J, Asko-Seljavaara S. Donor site morbidity of radial forearm flaps: A clinical and ultrasonographic evaluation. Scand J Plast Reconstr Surg Hand Surg. 1996; 3. 30(1):57–61. PMID: 8711443.6. Koshima I, Fukuda H, Yamamoto H, Moriguchi T, Soeda S, Ohta S. Free anterolateral thigh flaps for reconstruction of head and neck defects. Plast Reconstr Surg. 1993; 9. 92(3):421–428. PMID: 8341740.
Article7. Koshima I, Yamamoto H, Hosoda M, Moriguchi T, Orita Y, Nagayama H. Free combined composite flaps using the lateral circumflex femoral system for repair of massive defects of the head and neck regions: An introduction to the chimeric flap principle. Plast Reconstr Surg. 1993; 9. 92(3):411–420. PMID: 8341739.8. Chantrain G, Deraemaecker R, Andry G, Dor P. Wide vertical hemipharyngolaryngectomy with immediate glottic and pharyngeal reconstruction using a radial forearm free flap: preliminary results. Laryngoscope. 1991; 8. 101(8):869–875. PMID: 1865736.9. Kroll SS, Schusterman MA, Reece GP, Miller MJ, Evans GR, Robb GL, et al. Timing of pedicle thrombosis and flap loss after free-tissue transfer. Plast Reconstr Surg. 1996; 12. 98(7):1230–1233. PMID: 8942909.
Article10. Hidalgo DA, Disa JJ, Cordeiro PG, Hu QY. A review of 716 consecutive free flaps for oncologic surgical defects: refinement in donor-site selection and technique. Plast Reconstr Surg. 1998; 9. 102(3):722–732. PMID: 9727437.
Article11. Hidalgo DA, Jones CS. The role of emergent exploration in free-tissue transfer: a review of 150 consecutive cases. Plast Reconstr Surg. 1990; 9. 86(3):492–498. PMID: 2201050.12. Genden EM, Rinaldo A, Suarez C, Wei WI, Bradley PJ, Ferlito A. Complications of free flap transfers for head and neck reconstruction following cancer resection. Oral Oncol. 2004; 11. 40(10):979–984. PMID: 15509488.
Article13. Shaw WW. Microvascular free flaps: the first decade. Clin Plast Surg. 1983; 1. 10(1):3–20. PMID: 6340914.14. Shestak KC, Jones NF. Microsurgical free-tissue transfer in the elderly patient. Plast Reconstr Surg. 1991; 8. 88(2):259–263. PMID: 1852818.
Article15. Bui DT, Cordeiro PG, Hu QY, Disa JJ, Pusic A, Mehrara BJ. Free flap reexploration: indications, treatment, and outcomes in 1193 free flaps. Plast Reconstr Surg. 2007; 6. 119(7):2092–2100. PMID: 17519706.
Article16. Jones NF, Jarrahy R, Song JI, Kaufman MR, Markowitz B. Postoperative medical complications--not microsurgical complications--negatively influence the morbidity, mortality, and true costs after microsurgical reconstruction for head and neck cancer. Plast Reconstr Surg. 2007; 6. 119(7):2053–2060. PMID: 17519700.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Experience of Free Flap Reconstruction for Head and Neck Defect
- Six Cases of Reconstruction with Latissimus Dorsi Pedicled Flap for Head and Neck Defects in the Era of Free Flap Reconstruction
- Reconstruction of Midfacial Defect Using Various Free Flap
- The Clinical Study on the Most Common Donor Sites in Head and Neck Reconstruction using Free Flaps
- Book Review: Atlas of Regional and Free Flap for Head and Neck Reconstruction 2nd Edition