J Korean Med Sci.
2016 Nov;31(Suppl 2):S108-S113. 10.3346/jkms.2016.31.S2.S108.
Burden of Disease Study and Priority Setting in Korea: an Ethical Perspective
- Affiliations
-
- 1Department of Medical Education and Humanities, School of Medicine, Kyung Hee University, Seoul, Korea.
- 2Department of Medical Education, School of Medicine, Ewha Womans University, Seoul, Korea.
- 3Department of Preventive Medicine, School of Medicine, Kyung Hee University, Seoul, Korea. parenchyme@gmail.com
- KMID: 2360660
- DOI: http://doi.org/10.3346/jkms.2016.31.S2.S108
Abstract
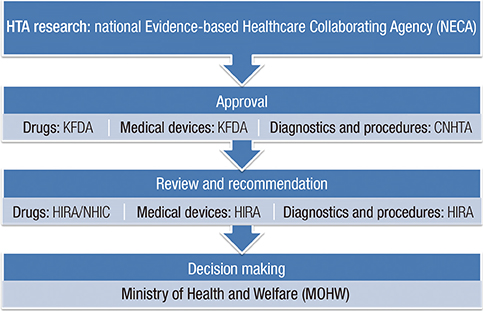
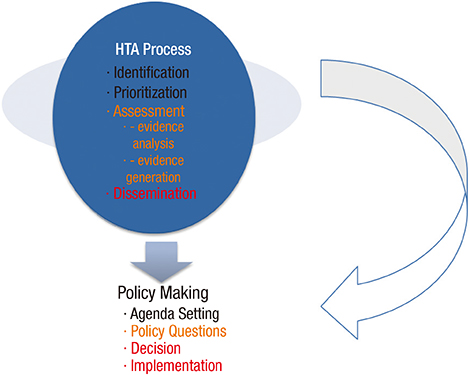
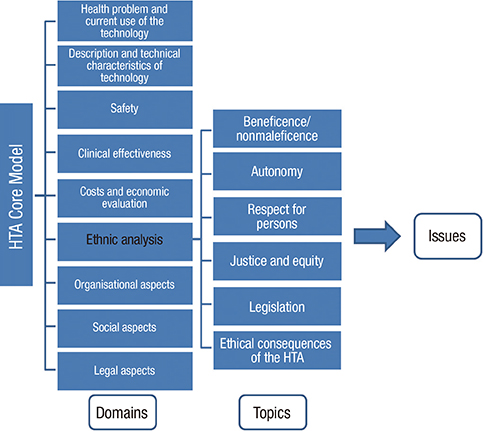
- When thinking about priority setting in access to healthcare resources, decision-making requires that cost-effectiveness is balanced against medical ethics. The burden of disease has emerged as an important approach to the assessment of health needs for political decision-making. However, the disability adjusted life years approach hides conceptual and methodological issues regarding the claims and value of disabled people. In this article, we discuss ethical issues that are raised as a consequence of the introduction of evidence-based health policy, such as economic evidence, in establishing resource allocation priorities. In terms of ethical values in health priority setting in Korea, there is no reliable rationale for the judgment used in decision-making as well as for setting separate and distinct priorities for different government bodies. An important question, therefore, is which ethical values guiding the practice of decision-making should be reconciled with the economic evidence found in Korean healthcare. The health technology assessment core model from the European network for Health Technology Assessment (EUnetHTA) project is a good example of incorporating ethical values into decision-making. We suggest that a fair distribution of scarce healthcare resources in South Korea can be achieved by considering the ethical aspects of healthcare.
MeSH Terms
Figure
Cited by 2 articles
-
Comparative Research for the Healthcare Budget and Burden of Disease in Perspective Resource Allocation
So-Youn Park, Seok-Jun Yoon, Hyesook Park, Min-Woo Jo, In-Hwan Oh
J Korean Med Sci. 2019;34(Suppl 1):. doi: 10.3346/jkms.2019.34.e81.Korean National Burden of Disease: The Importance of Diabetes Management
Chung-Nyun Kim, Yoon-Sun Jung, Young-Eun Kim, Minsu Ock, Seok-Jun Yoon
Diabetes Metab J. 2024;48(4):518-530. doi: 10.4093/dmj.2024.0087.
Reference
-
1. World Bank. World Development Report 1993: Investing in Health. New York, NY: Oxford University Press;1993.2. Murray CJ. Rethinking DALYs. In : Murray CJ, Lopez AD, editors. The Global Burden of Disease: a Comprehensive Assessment of Mortality and Disability from Diseases, Injuries and Risk Factors in 1990 and Projected to 2020 (Global Burden of Disease and Injury Series Vol. 1). Cambridge, MA: Harvard University Press;1996. p. 1–98.3. Ruger JP. Ethics in American health 1: ethical approaches to health policy. Am J Public Health. 2008; 98:1751–1756.4. Arnesen T, Nord E. The value of DALY life: problems with ethics and validity of disability adjusted life years. BMJ. 1999; 319:1423–1425.5. Gibson JL, Martin DK, Singer PA. Priority setting for new technologies in medicine: a transdisciplinary study. BMC Health Serv Res. 2002; 2:14.6. Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC; Panel on Cost-Effectiveness in Health and Medicine. The role of cost-effectiveness analysis in health and medicine. JAMA. 1996; 276:1172–1177.7. Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009; 24:63–71.8. Jones RS. Health-Care Reform in Korea: OECD Economics Department Working Papers No. 797. Paris: OECD Publishing;2010.9. Ahn J, Kim G, Suh HS, Lee SM. Social values and healthcare priority setting in Korea. J Health Organ Manag. 2012; 26:343–350.10. Kim Y. Towards universal coverage: an evaluation of the benefit enhancement plan for four major conditions in Korean National Health Insurance. J Korean Med Assoc. 2014; 57:198–203.11. Health Insurance Review and Assessment Service (KR). HIRA information system [Internet]. accessed on 27 November 2015. Available at http://www.hira.or.kr/dummy.do?pgmid=HIRAA070001000510.12. Clark S, Weale A. Social values in health priority setting: a conceptual framework. J Health Organ Manag. 2012; 26:293–316.13. Saarni SI, Gylling HA. Evidence based medicine guidelines: a solution to rationing or politics disguised as science? J Med Ethics. 2004; 30:171–175.14. Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ. 2001; 323:334–336.15. Shekelle PG, Woolf SH, Eccles M, Grimshaw J. Clinical guidelines: developing guidelines. BMJ. 1999; 318:593–596.16. Kristensen FB, Lampe K, Chase DL, Lee-Robin SH, Wild C, Moharra M, Garrido MV, Nielsen CP, Røttingen JA, Neikter SA, et al. Practical tools and methods for health technology assessment in Europe: structures, methodologies, and tools developed by the European Network for Health Technology Assessment, EUnetHTA. Int J Technol Assess Health Care. 2009; 25:Suppl 2. 1–8.17. Saarni SI, Hofmann B, Lampe K, Lühmann D, Mäkelä M, Velasco-Garrido M, Autti-Rämö I. Ethical analysis to improve decision-making on health technologies. Bull World Health Organ. 2008; 86:617–623.18. Lampe K, Mäkelä M, Garrido MV, Anttila H, Autti-Rämö I, Hicks NJ, Hofmann B, Koivisto J, Kunz R, Kärki P, et al. The HTA core model: a novel method for producing and reporting health technology assessments. Int J Technol Assess Health Care. 2009; 25:Suppl 2. 9–20.19. EUnetHTA (FI). Joint action 2, work package 8: HTA Core Model® version 2.1 [Internet]. accessed on 12 November 2015. Available at http://meka.thl.fi/htacore/model/HTACoreModel2.1PublicDraft.pdf.20. EUnetHTA (FI). Work package 4: Core HTA on drug eluting stents, pilot assessment [Internet]. accessed on 30 November 2015. Available at http://www.eunethta.eu/outputs/core-hta-drug-eluting-stents.21. Deyo RA, Patrick DL. Medical innovations and American culture. In : Deyo RA, Patrick DL, editors. Hope or Hype: the Obsession with Medical Advances and the High Cost of False Promises. New York, NY: AMACOM;2005. p. 13–25.22. Park DA, Ahn J, Yun JE, Rhee J, Lee NR, Son SK, Lim S, Lee MJ, Lee SH, Oh EH. The System Development of Clinical Study for Conditional Coverage with Evidence Generation. Seoul: National Evidence-based Healthcare Collaborating Agency;2015.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Setting a Health Policy Research Agenda for Controlling Cancer Burden in Korea
- Ethical Priority Setting for Successful Publishing by Iranian Scientists
- Study on the Criteria for Priority-Setting and Application in Expanding Health Insurance Benefit of Preventive Medical Service: The Case of Obesity
- Effects of Clinical Nurses' Ethical Climate and Ethical Nursing Competence on Moral Distress
- Understanding of medical ethics among medical students and residents