J Korean Soc Radiol.
2016 Dec;75(6):480-486. 10.3348/jksr.2016.75.6.480.
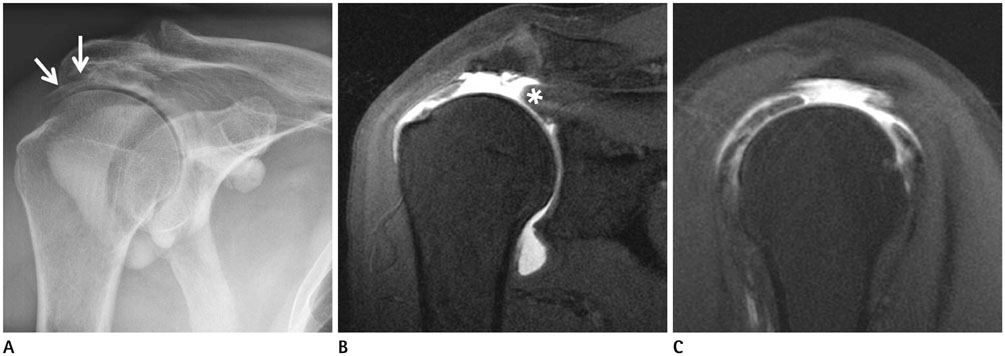
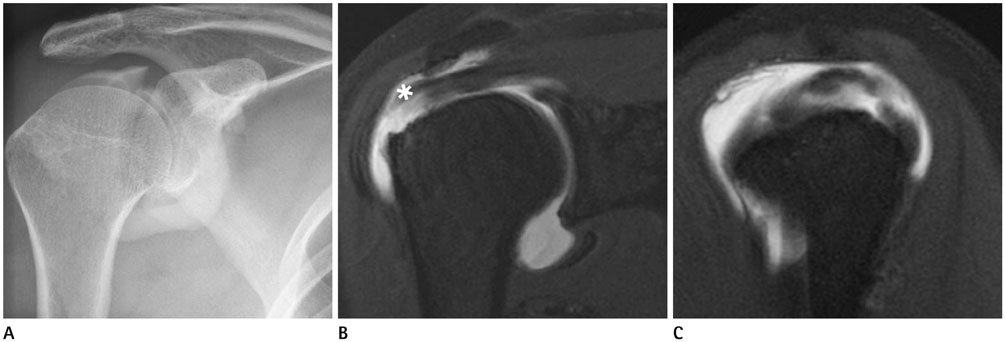
Discrepancy between Fluoroscopic Arthrography and Magnetic Resonance Arthrography in Patients with Arthroscopically Confirmed Supraspinatus Tendon Tears: The Additional Benefit of Cine Fluoroscopic Arthrography Images
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiological Science, Medical Convergence Research Institute, and Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea. jss@yuhs.ac
- 2Department of Radiology, Inje University College of Medicine, Haeundae Paik Hospital, Busan, Korea.
- KMID: 2360436
- DOI: http://doi.org/10.3348/jksr.2016.75.6.480
Abstract
- PURPOSE
To determine the additional diagnostic benefits of fluoroscopic arthrography (FA) in patients with full-thickness supraspinatus tendon (SST) tears by comparing FA images with magnetic resonance arthrography (MRA) images.
MATERIALS AND METHODS
This study included FA and MRA images of 53 patients who were confirmed to have full-thickness SST tears by arthroscopy. In the FA analysis, the presence of contrast leakage into the subacromial-subdeltoid bursa was recorded. In the MRA analysis, contrast leakage, retraction of a torn tendon, width and length of the tear, and supraspinatus atrophy were evaluated. Patients were divided into the concordant group or the discordant group based on the presence of contrast leakage to compare the characteristics of SST tears. We used Fisher's exact test and two-sample t-test for the comparison.
RESULTS
Of the 53 patients, 34 were included in the concordant group and 19 were included in the discordant group. In the concordant group, the grades of retraction were higher than those in the discordant group; the width and length of the tears were larger. Muscle atrophy was more severe in the concordant group.
CONCLUSION
A full-thickness SST tear did not always exhibit contrast leakage on FA, particularly small SST tears or tears with low-grade retraction. FA can provide diagnostic information regarding the severity of full-thickness SST tears by itself.
MeSH Terms
Figure
Reference
-
1. Spick C, Szolar DH, Reittner P, Preidler KW, Tillich M. MR arthrography of the shoulder: do we need local anesthesia? Eur J Radiol. 2014; 83:980–983.2. de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol. 2009; 192:1701–1707.3. Elentuck D, Palmer WE. Direct magnetic resonance arthrography. Eur Radiol. 2004; 14:1956–1967.4. Jacobson JA, Lin J, Jamadar DA, Hayes CW. Aids to successful shoulder arthrography performed with a fluoroscopically guided anterior approach. Radiographics. 2003; 23:373–378. discussion 379.5. Hodler J, Kursunoglu-Brahme S, Snyder SJ, Cervilla V, Karzel RP, Schweitzer ME, et al. Rotator cuff disease: assessment with MR arthrography versus standard MR imaging in 36 patients with arthroscopic confirmation. Radiology. 1992; 182:431–436.6. Flannigan B, Kursunoglu-Brahme S, Snyder S, Karzel R, Del Pizzo W, Resnick D. MR arthrography of the shoulder: comparison with conventional MR imaging. AJR Am J Roentgenol. 1990; 155:829–832.7. Jbara M, Chen Q, Marten P, Morcos M, Beltran J. Shoulder MR arthrography: how, why, when. Radiol Clin North Am. 2005; 43:683–692. viii8. Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990; (254):81–86.9. Mellado JM, Calmet J, Olona M, Esteve C, Camins A, Pérez Del Palomar L, et al. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. AJR Am J Roentgenol. 2005; 184:1456–1463.10. Warner JJ, Higgins L, Parsons IM 4th, Dowdy P. Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2001; 10:37–46.11. Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand. 1996; 67:264–268.12. Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. AJR Am J Roentgenol. 2008; 190:1105–1111.13. Hegedus EJ, Zavala J, Kissenberth M, Cook C, Cassas K, Hawkins R, et al. Positive outcomes with intra-articular glenohumeral injections are independent of accuracy. J Shoulder Elbow Surg. 2010; 19:795–801.14. Malfair D. Therapeutic and diagnostic joint injections. Radiol Clin North Am. 2008; 46:439–453. v
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Dynamic Cine-Arthrography for Wrist Instability as Correlated with Arthroscopic Palmer Classification
- Feasibility of Ultrasonography and MR Arthrography during Evaluation of Rotator Cuff Injury
- Arthrography of the ankle sprains
- 16-Slice MDCT Arthrography of the Shoulder: Accuracy for Detection of Glenoid Labral and Rotator Cuff Tears
- Evaluation of Meniscal Tears of Knee by Post - arthrographic High Resolution CT