Korean J Urol.
2015 Dec;56(12):811-816. 10.4111/kju.2015.56.12.811.
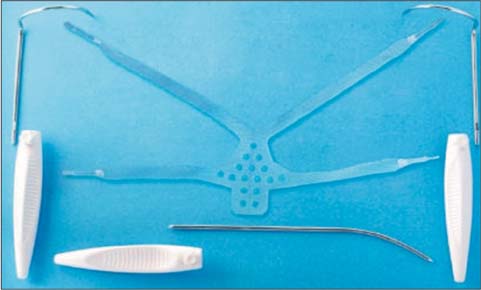
Simultaneous treatment of anterior vaginal wall prolapse and stress urinary incontinence by using transobturator four arms polypropylene mesh
- Affiliations
-
- 1Urology-Nephrology Research Center, Labbafinejad Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 2Kerman University of Medical Sciences, Kerman, Iran. azdaneshpajooh@yahoo.com
- KMID: 2359873
- DOI: http://doi.org/10.4111/kju.2015.56.12.811
Abstract
- PURPOSE
To evaluate the medium-term efficacy and safety of transobturator four-arm polypropylene mesh in the treatment of high-stage anterior vaginal wall prolapse and concomitant stress urinary incontinence (SUI).
MATERIALS AND METHODS
Between September 2010 and August 2013, a prospective single-center trial was performed to evaluate women with stage> or =3 anterior vaginal wall prolapse with or without SUI who presented to Labbafinejad Hospital, Teheran, Iran, and underwent anterior vaginal wall repair with polypropylene mesh. Pre- and postoperative evaluation included history; physical examination using the Pelvic Organ Prolapse Quantification system and cough stress test, both before and after reduction of prolapsed structures; Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire (PFIQ); urinalysis and culture; and a postvoid residual assessment. Complications were reported at a mean of 2 years of follow-up.
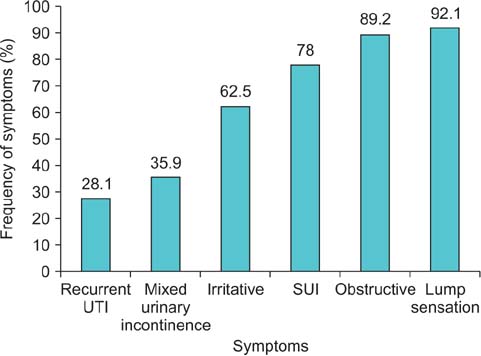
RESULTS
A total of 71 patients underwent cystocele repair with the transobturator four-arm polypropylene mesh. Seven of the patients were lost to follow-up. There were no perioperative complications. The anatomical success rate was 87.5%. The subjective success rate was 92.1%. The PFDI and PFIQ were significantly improved after surgery (p<0.001). Among those with the simultaneous complaint of SUI, 82% were cured without any additional procedure. Three patients (4.6%) experienced vaginal mesh extrusion. Two patients (3.1%) reported worsening of dyspareunia after surgery.
CONCLUSIONS
The four arms polypropylene mesh is an effective device for simultaneous correction of anterior vaginal wall prolapse and SUI with a low complication rate at a medium-term follow-up. The majority of the subgroup with concomitant SUI were cured without a second simultaneous procedure.
MeSH Terms
Figure
Reference
-
1. Moore RD, Beyer RD, Jacoby K, Freedman SJ, McCammon KA, Gambla MT. Prospective multicenter trial assessing type I, polypropylene mesh placed via transobturator route for the treatment of anterior vaginal prolapse with 2-year follow-up. Int Urogynecol J. 2010; 21:545–552.2. Rane A, Iyer J, Kannan K, Corstiaans A. Prospective study of the Perigee™ system for treatment of cystocele - our five-year experience. Aust N Z J Obstet Gynaecol. 2012; 52:28–33.3. Keys T, Campeau L, Badlani G. Synthetic mesh in the surgical repair of pelvic organ prolapse: current status and future directions. Urology. 2012; 80:237–243.4. Park HK, Paick SH, Lee BK, Kang MB, Jun KK, Kim HG. Initial experience with concomitant prolift™ system and tension-free vaginal tape procedures in patients with stress urinary incontinence and cystocele. Int Neurourol J. 2010; 14:43–47.5. Borstad E, Kulseng-Hanssen S, Moghimi K, Sandved M, Majida M, Western K, et al. An incontinence procedure performed at the time of prolapse repair might be unnecessary surgery [Abstract]. Neuroulogy and urodynamics. 2006; 25:551–552. Abstract No. 356. Palma P, Riccetto C, Muller V, Rogerio F, Sarsotti C, Ortiz C, et al. Nazca: a monoprosthesis for the simultaneous correction of cystocele and urinary stress incontinence - a multicentric trial. Urology. 2007; 70:Supplement 3A. 193–194.7. Chapple CR, Milsom I. Urinary incontinence and pelvic prolapse. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders;2012. p. 1900–1903.8. Handel LN, Frenkl TL, Kim YH. Results of cystocele repair: a comparison of traditional anterior colporrhaphy, polypropylene mesh and porcine dermis. J Urol. 2007; 178:153–156.9. Lucente V, Murphy M, Saiz C. Vaginal prolapse repair: suture repair versus mesh augmentation: a urogynecology perspective. Urol Clin North Am. 2012; 39:325–333.10. Clark AL, Gregory T, Smith VJ, Edwards R. Epidemiologic evaluation of reoperation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol. 2003; 189:1261–1267.11. Maher C, Baessler K, Glazener CM, Adams EJ, Hagen S. Surgical management of pelvic organ prolapse in women: a short version Cochrane review. Neurourol Urodyn. 2008; 27:3–12.12. Nieminen K, Hiltunen R, Takala T, Heiskanen E, Merikari M, Niemi K, et al. Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. Am J Obstet Gynecol. 2010; 203:235.e1–235.e8.13. Wu MP, Long CH, Liang CH. Staged or concomitant surgery for correcting pelvic organ prolapse and stress urinary incontinence. Incont Pelvic Floor Dysfunct. 2010; 4:93–98.14. Sergent F, Sentilhes L, Resch B, Verspyck E, Medeiros R, Descamps P, et al. Treatment of concomitant prolapse and stress urinary incontinence via a transobturator subvesical mesh without independent suburethral tape. Acta Obstet Gynecol Scand. 2010; 89:223–229.15. Marks BK, Goldman HB. Controversies in the management of mesh-based complications: a urology perspective. Urol Clin North Am. 2012; 39:419–428.16. Zoorob D, Karram M. Management of mesh complications and vaginal constriction: a urogynecology perspective. Urol Clin North Am. 2012; 39:413–418.17. Nguyen JN, Burchette RJ. Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol. 2008; 111:891–898.18. Withagen MI, Milani AL, den Boon J, Vervest HA, Vierhout ME. Trocar-guided mesh compared with conventional vaginal repair in recurrent prolapse: a randomized controlled trial. Obstet Gynecol. 2011; 117(2 Pt 1):242–250.19. Altman D, Vayrynen T, Engh ME, Axelsen S, Falconer C. Nordic Transvaginal Mesh Group. Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med. 2011; 364:1826–1836.20. Vollebregt A, Fischer K, Gietelink D, van der Vaart CH. Primary surgical repair of anterior vaginal prolapse: a randomised trial comparing anatomical and functional outcome between anterior colporrhaphy and trocar-guided transobturator anterior mesh. BJOG. 2011; 118:1518–1527.21. Lopes ED, Lemos NL, Carramão Sda S, Lunardelli JL, Ruano JM, Aoki T, et al. Transvaginal polypropylene mesh versus sacrospinous ligament fixation for the treatment of uterine prolapse: 1-year follow-up of a randomized controlled trial. Int Urogynecol J. 2010; 21:389–394.22. Abed H, Rahn DD, Lowenstein L, Balk EM, Clemons JL, Rogers RG, et al. Incidence and management of graft erosion, wound granulation, and dyspareunia following vaginal prolapse repair with graft materials: a systematic review. Int Urogynecol J. 2011; 22:789–798.23. Sentilhes L, Berthier A, Sergent F, Verspyck E, Descamps P, Marpeau L. Sexual function in women before and after transvaginal mesh repair for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:763–772.24. Nieminen K, Hiltunen R, Heiskanen E, Takala T, Niemi K, Merikari M, et al. Symptom resolution and sexual function after anterior vaginal wall repair with or without polypropylene mesh. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:1611–1616.25. Gauruder-Burmester A, Koutouzidou P, Tunn R. Effect of vaginal polypropylene mesh implants on sexual function. Eur J Obstet Gynecol Reprod Biol. 2009; 142:76–80.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter to the editor: Comment on "Simultaneous treatment of anterior vaginal wall prolapse and stress urinary incontinence by using transobturator four arms polypropylene mesh"
- The authors reply: Simultaneous treatment of anterior vaginal wall prolapse and stress urinary incontinence by using transobturator four arms polypropylene mesh
- Vaginal Approaches Using Synthetic Mesh to Treat Pelvic Organ Prolapse
- Treatment of Anterior Vaginal Wall Prolapse Using Transvaginal Anterior Mesh With Apical Fixation: A Prospective Multicenter Study With up to 2 Years of Follow-up
- Vaginal Erosion and Pelvic Abscess after Anterior Intravaginal Slingplasty (IVS) in Patient with Stress Urinary Incontinence