Korean J Gastroenterol.
2016 Sep;68(3):161-165. 10.4166/kjg.2016.68.3.161.
A Case of Idiopathic Severe Acute Pancreatitis following Cesarean Section Delivery
- Affiliations
-
- 1Department of Internal Medicine and Liver Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. drjaihwan@snu.ac.kr
- KMID: 2358720
- DOI: http://doi.org/10.4166/kjg.2016.68.3.161
Abstract
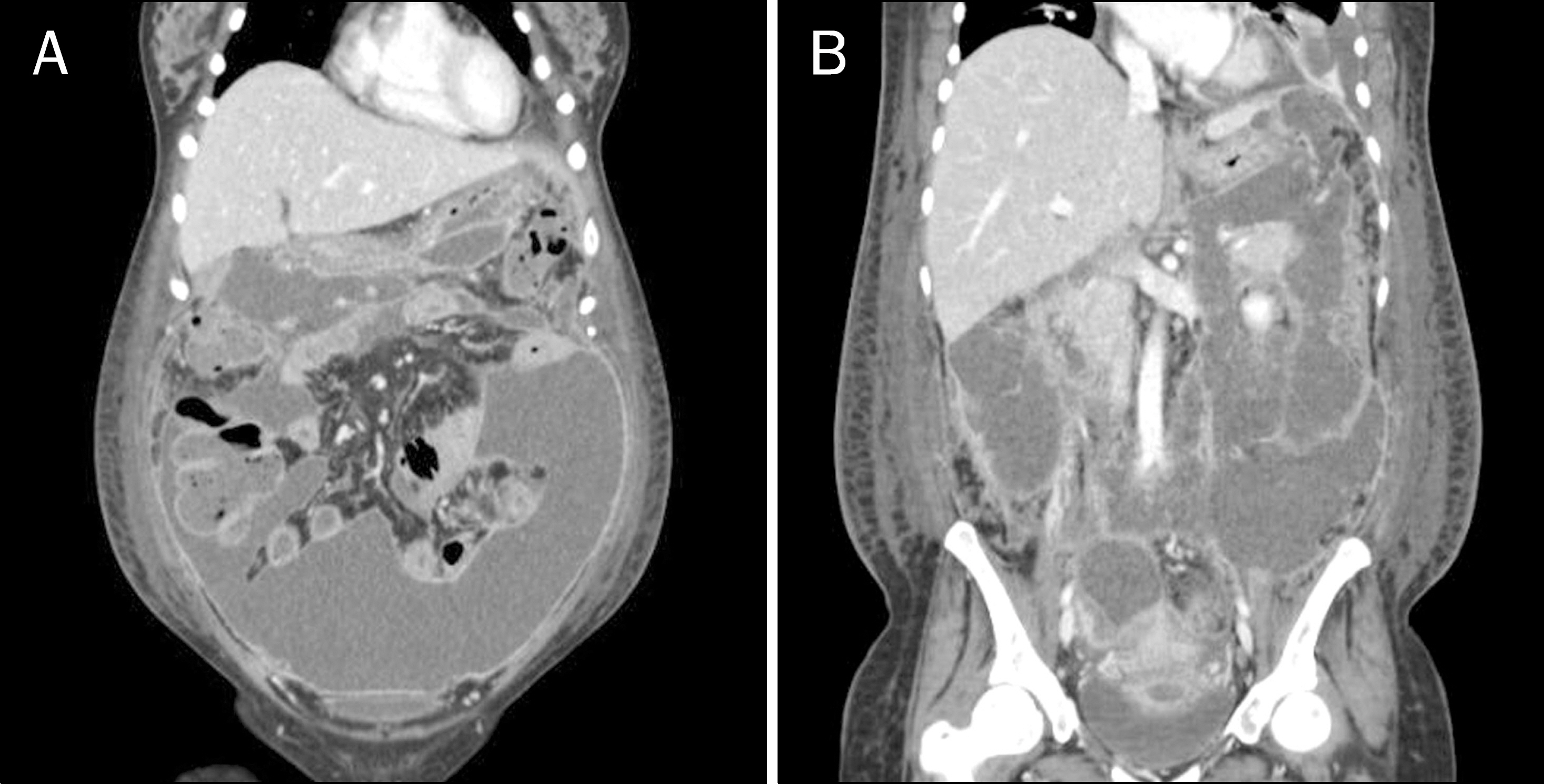
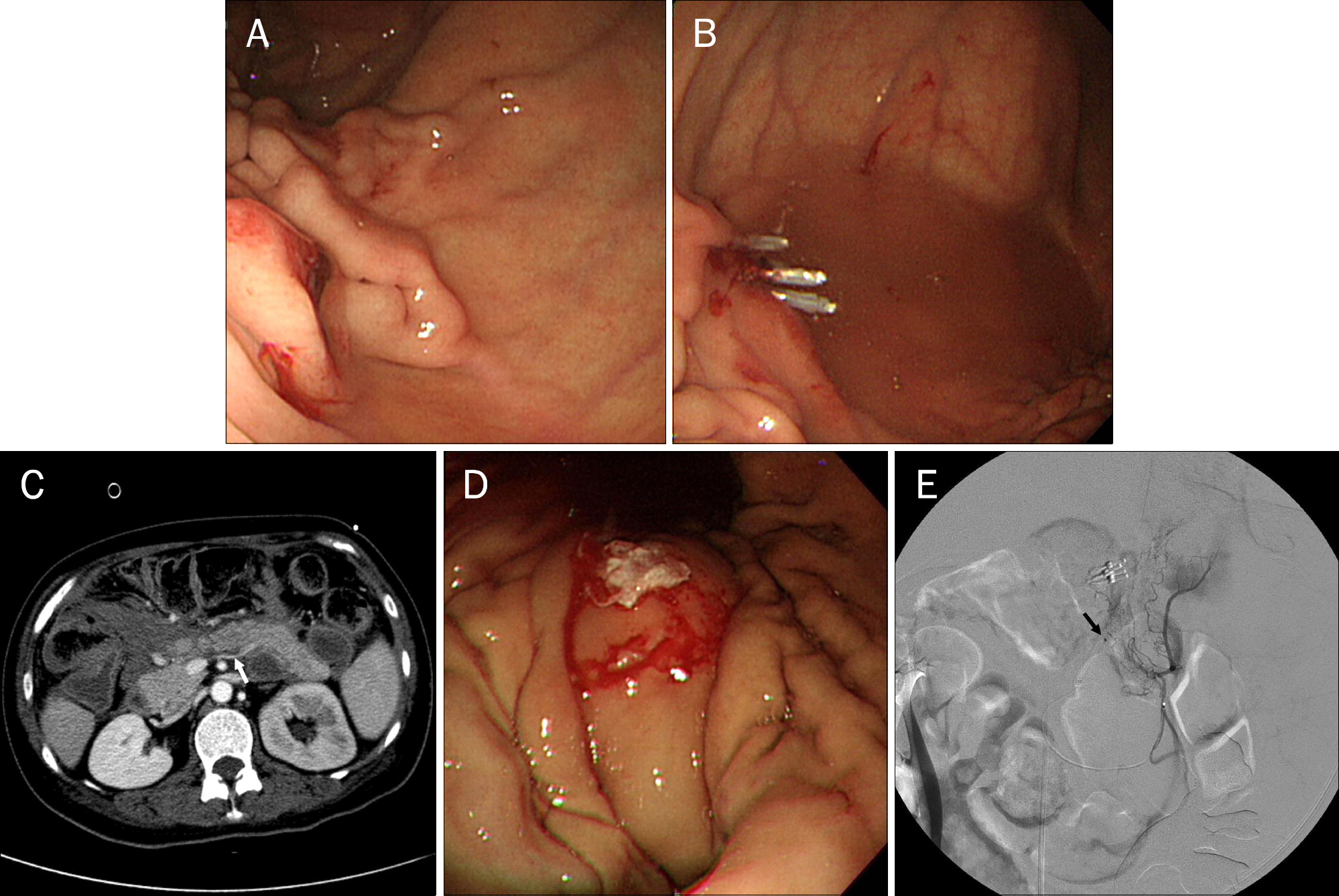
- Acute pancreatitis rarely occurs in the postpartum period. Furthermore, there are very few reports of it after cesarean section delivery. A 35-year-old woman presented with dyspnea and abdominal distension on the third day after cesarean section delivery. Under a suspicion of acute pancreatitis, she was initially managed with conservative treatment. However, she developed intra-abdominal fluid collections and gastric bleeding, which were managed with percutaneous drainage, endoscopic hemostasis, and angiographic embolization. She was discharged with good clinical recovery. Postpartum pancreatitis, especially after cesarean section, is rare; however, its management is not different from that for usual pancreatitis.
MeSH Terms
Figure
Reference
-
References
1. Granger J, Remick D. Acute pancreatitis: models, markers, and mediators. Shock. 2005; 24(Suppl 1):45–51.
Article2. Wang GJ, Gao CF, Wei D, Wang C, Ding SQ. Acute pancreatitis: etiology and common pathogenesis. World J Gastroenterol. 2009; 15:1427–1430.
Article3. Papadakis EP, Sarigianni M, Mikhailidis DP, Mamopoulos A, Karagiannis V. Acute pancreatitis in pregnancy: an overview. Eur J Obstet Gynecol Reprod Biol. 2011; 159:261–266.
Article4. Ramin KD, Ramsey PS. Disease of the gallbladder and pancreas in pregnancy. Obstet Gynecol Clin North Am. 2001; 28:571–580.
Article5. Xu Q, Wang S, Zhang Z. A 23-year, single-center, retrospective analysis of 36 cases of acute pancreatitis in pregnancy. Int J Gynaecol Obstet. 2015; 130:123–126.
Article6. Eddy JJ, Gideonsen MD, Song JY, Grobman WA, O'Halloran P. Pancreatitis in pregnancy. Obstet Gynecol. 2008; 112:1075–1081.
Article7. Hernandez A, Petrov MS, Brooks DC, Banks PA, Ashley SW, Tavakkolizadeh A. Acute pancreatitis and pregnancy: a 10-year single center experience. J Gastrointest Surg. 2007; 11:1623–1627.
Article8. Redechová S, Féderová L, Hammerová L, Filkászová A, Horváthová D, Redecha M. Thrombotic microangiopathy in pregnancy complicated by acute hemorrhagic-necrotic pancreatitis during early puerperium. Ceska Gynekol. 2014; 79:190–192.9. Jeon SY, Jung E, Seol HJ, Hur YJ. Development of Purtscher-like retinopathy after pre-eclampsia combined with acute pancreatitis. Obstet Gynecol Sci. 2013; 56:261–264.
Article10. Raheem M, Lala A, Abukhalil I. An aggressive presentation of postpartum acute necrotizing pancreatitis. J Obstet Gynaecol. 2004; 24:703–704.
Article11. Guth A, Ekoundzola JR, Beauséjour B, Nassar J, Colin JP. Acute pancreatitis in the puerperium. Diagnostic problems following cesarean section. J Gynecol Obstet Biol Reprod (Paris). 1985; 14:753–756.12. Vonlaufen A, Wilson JS, Apte MV. Molecular mechanisms of pancreatitis: current opinion. J Gastroenterol Hepatol. 2008; 23:1339–1348.
Article13. Lankisch PG, Apte M, Banks PA. Acute pancreatitis. Lancet. 2015; 386:85–96.
Article14. White MT, Morgan A, Hopton D. Postoperative pancreatitis. A study of seventy cases. Am J Surg. 1970; 120:132–137.15. Gan SI, Edwards AL, Symonds CJ, Beck PL. Hypertriglyceridemia- induced pancreatitis: a case-based review. World J Gastroenterol. 2006; 12:7197–7202.16. Dominguez-Muñoz JE, Malfertheiner P, Ditschuneit HH, et al. Hyperlipidemia in acute pancreatitis. Relationship with etiology, onset, and severity of the disease. Int J Pancreatol. 1991; 10:261–267.17. Pitchumoni CS, Yegneswaran B. Acute pancreatitis in pregnancy. World J Gastroenterol. 2009; 15:5641–5646.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An anesthetic experience with cesarean section in a patient with vasovagal syncope: A case report
- Sudden Cardiac Arrest Postoperative Day due to Pulmonary Embolism
- A Study Female of Fecal Incontinence: Effects of Parity & Delivery method
- Effect of Labor Epidural Analgesia on Rates of Cesarean Section and Vacuum Delivery
- Takotsubo-Like Severe Left Ventricular Dysfunction After Cesarean Delivery in a 28-Year Old Woman