Korean J Gastroenterol.
2016 Sep;68(3):156-160. 10.4166/kjg.2016.68.3.156.
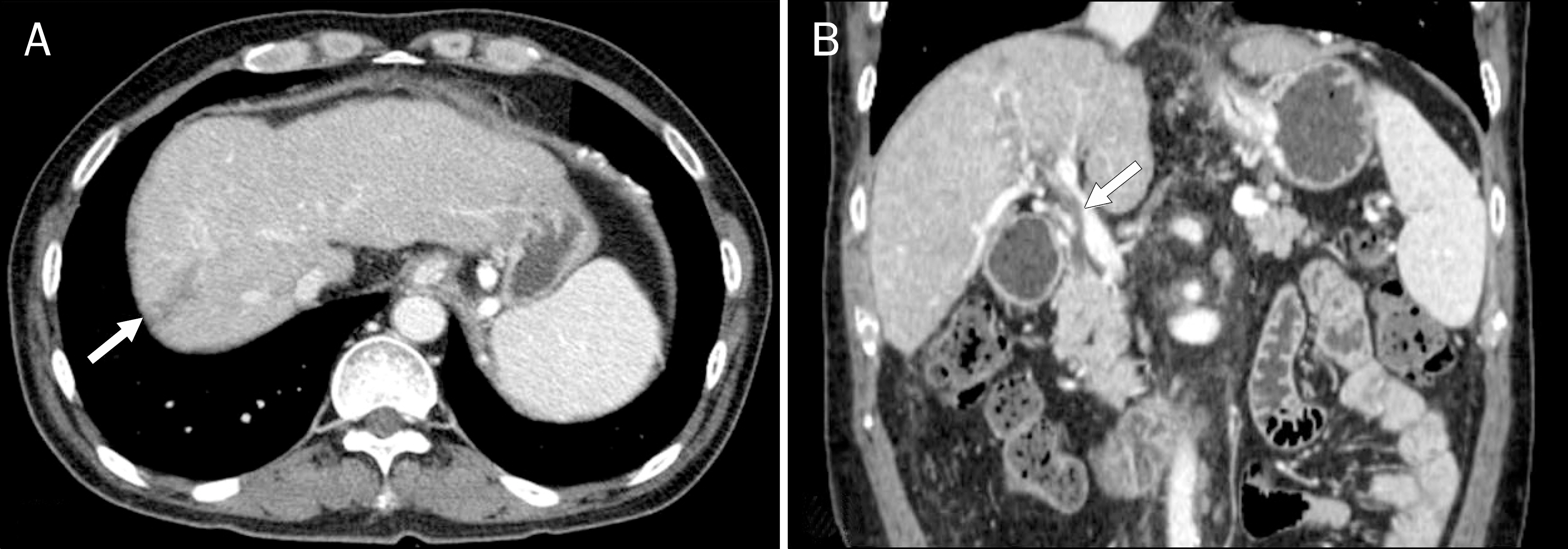
Hepatic Infarction Caused by Portal Vein Thrombophlebitis Misdiagnosed as Infiltrative Hepatic Malignancy with Neoplastic Thrombus
- Affiliations
-
- 1Department of Internal Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea. phn223@cha.ac.kr
- 2Division of Gastroenterology and Hepatology, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- KMID: 2358719
- DOI: http://doi.org/10.4166/kjg.2016.68.3.156
Abstract
- Portal vein thrombosis (PVT) is a form of venous thrombosis that usually presents in chronic form without any sequalae in patients with hepatocellular carcinoma (HCC) or liver cirrhosis. Accurate differential diagnosis of bland PVT from neoplastic PVT is an important step for planning treatment options, but the acute form can be challenging. Here we present a case of acute hepatic infarction caused by acute bland PVT combined with pylephlebitis, which was misdiagnosed as infiltrative hepatic malignancy with neoplastic PVT owing to the perplexing imaging results and elevated tumor markers.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Bauer W, Dale HH, Poulsson LT, Richards DW. The control of circulation through the liver. J Physiol. 1932; 74:343–375.
Article2. Ponziani FR, Zocco MA, Campanale C, et al. Portal vein thrombosis: insight into physiopathology, diagnosis, and treatment. World J Gastroenterol. 2010; 16:143–155.
Article3. Li C, Hu J, Zhou D, et al. Differentiation of bland from neoplastic thrombus of the portal vein in patients with hepatocellular carcinoma: application of susceptibility-weighted MR imaging. BMC Cancer. 2014; 14:590.
Article4. Lang SA, Loss M, Wohlgemuth WA, Schlitt HJ. Clinical management of acute portal/mesenteric vein thrombosis. Viszeralmedizin. 2014; 30:394–400.
Article5. Chawla YK, Bodh V. Portal vein thrombosis. J Clin Exp Hepatol. 2015; 5:22–40.
Article6. Shah V. Molecular mechanisms of increased intrahepatic resistance in portal hypertension. J Clin Gastroenterol. 2007; 41(Suppl 3):S259–S261.
Article7. Harding DJ, Perera MT, Chen F, Olliff S, Tripathi D. Portal vein thrombosis in cirrhosis: controversies and latest developments. World J Gastroenterol. 2015; 21:6769–6784.
Article8. Plessier A, Darwish-Murad S, Hernandez-Guerra M, et al. Acute portal vein thrombosis unrelated to cirrhosis: a prospective multicenter follow-up study. Hepatology. 2010; 51:210–218.
Article9. Takizawa D, Kakizaki S, Sohara N, et al. Hepatocellular carcinoma with portal vein tumor thrombosis: clinical characteristics, prognosis, and patient survival analysis. Dig Dis Sci. 2007; 52:3290–3295.
Article10. Jelic S, Sotiropoulos GC. ESMO Guidelines Working Group. Hepatocellular carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010; 21(Suppl 5):v59–v64.
Article11. Engelbrecht M, Akin O, Dixit D, Schwartz L. Bland and tumor thrombi in abdominal malignancies: magnetic resonance imaging assessment in a large oncologic patient population. Abdom Imaging. 2011; 36:62–68.
Article12. Tublin ME, Dodd GD 3rd, Baron RL. Benign and malignant portal vein thrombosis: differentiation by CT characteristics. AJR Am J Roentgenol. 1997; 168:719–723.
Article13. Lee HK, Park SJ, Yi BH, Yeon EK, Kim JH, Hong HS. Portal vein thrombosis: CT features. Abdom Imaging. 2008; 33:72–79.
Article14. Kanellopoulou T, Alexopoulou A, Theodossiades G, Koskinas J, Archimandritis AJ. Pylephlebitis: an overview of non-cirrhotic cases and factors related to outcome. Scand J Infect Dis. 2010; 42:804–811.
Article15. Wong K, Weisman DS, Patrice KA. Pylephlebitis: a rare complication of an intraabdominal infection. J Community Hosp Intern Med Perspect. 2013; 3:DOI: doi:10.3402/jchimp.v312.20732.
Article16. DeLeve LD, Valla DC, Garcia-Tsao G. Vascular disorders of the liver. Hepatology. 2009; 49:1729–1764.
Article17. Lee YY, Tee HP, Mahadeva S. Role of prophylactic antibiotics in cirrhotic patients with variceal bleeding. World J Gastroenterol. 2014; 20:1790–1796.
Article18. Albert MB, Steinberg WM, Henry JP. Elevated serum levels of tumor marker CA19–9 in acute cholangitis. Dig Dis Sci. 1988; 33:1223–1225.
Article19. Pavai S, Yap SF. The clinical significance of elevated levels of serum CA 19–9. Med J Malaysia. 2003; 58:667–672.20. Singhal A, Lander E, Karachristos A, et al. Elevation of CA 125 and CA 19–9 in patients with end-stage liver disease. Int J Biol Markers. 2012; 27:e147–e151.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hepatic Infarction Complicating Acute Pancreatitis: A Case Report
- Portal and hepatic vein thrombosis after transjugular intrahepatic portosystemic shunt: Incidence in follow-up imaging and clinical implications
- Hepatic Resection in Patients with Hepatocellular Carcinoma Accompanied by Portal Vein Thrombus
- A Case of Hepatic Artery-Portal Vein Fistula
- Ultrasonographic Measurement of the Diameter of a Normal Bile Duct, Hepatic Artery and Portal Vein in Infants Younger Than 3 Months