Korean J Neurotrauma.
2016 Oct;12(2):135-139. 10.13004/kjnt.2016.12.2.135.
The Impact of Engorged Vein within Traumatic Posterior Neck Muscle Identified in Preoperative Computed Tomography Angiography to Estimated Blood Loss during Posterior Upper Cervical Spine Surgery
- Affiliations
-
- 1Department of Neurosurgery and Medical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea. csfdiver@naver.com
- 2Department of Neuroradiology, Pusan National University Hospital, Busan, Korea.
- KMID: 2356787
- DOI: http://doi.org/10.13004/kjnt.2016.12.2.135
Abstract
OBJECTIVE
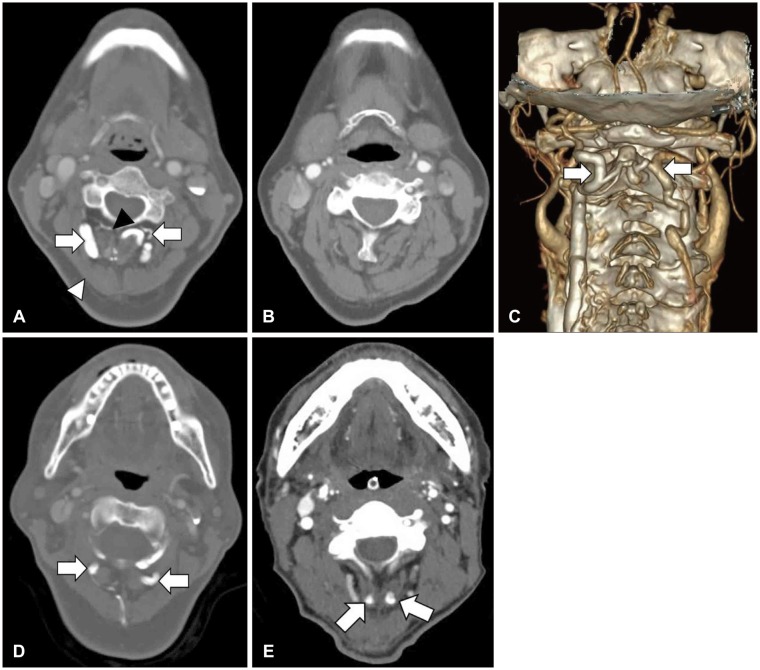
Injuries of upper cervical spine are potentially fatal. Thus, appropriate diagnosis and treatment is essential. In our institute, preoperative computed tomography angiography (CTA) has been performed for evaluation of injuries of bony and vascular structure. The authors confirmed the engorged venous plexus within injured posterior neck muscle. We have this research to clarify the relationship between the engorged venous plexus and engorged vein.
METHODS
A retrospective review identified 23 adult patients who underwent 23 posterior cervical spine surgeries for treatment of upper cervical injury between 2013 and 2015. Preoperative CTA was used to identify of venous engorgement within posterior neck muscle. The male to female ratio was 18:5 and the mean age was 53.5 years (range, 25-78 years). Presence of venous engorgement and estimated blood loss (EBL) were analyzed retrospectively.
RESULTS
The EBL of group with venous engorgement was 454.55 mL. The EBL of group without venous engorgement was 291.67 mL. The EBL of group with venous engorgement was larger than control group in significant.
CONCLUSION
The presence of engorged venous plexus is important factor of intraoperative bleeding. Preoperative CTA for identifying of presence of engorged venous plexus and fine operative techniques is important to decrease of blood loss during posterior cervical spine surgery.
MeSH Terms
Figure
Reference
-
1. Arnautović KI, al-Mefty O, Pait TG, Krisht AF, Husain MM. The suboccipital cavernous sinus. J Neurosurg. 1997; 86:252–262. PMID: 9010427.
Article2. Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978; 60:279–284. PMID: 348703.
Article3. Caruso RD, Rosenbaum AE, Chang JK, Joy SE. Craniocervical junction venous anatomy on enhanced MR images: the suboccipital cavernous sinus. AJNR Am J Neuroradiol. 1999; 20:1127–1131. PMID: 10445456.4. Denaro V, Di Martino A. Cervical spine surgery: an historical perspective. Clin Orthop Relat Res. 2011; 469:639–648. PMID: 21213087.
Article5. Dickman CA, Sonntag VK. Posterior C1-C2 transarticular screw fixation for atlantoaxial arthrodesis. Neurosurgery. 1998; 43:275–280. discussion 280-281. PMID: 9696080.
Article6. Duan S, Lv S, Ye F, Lin Q. Imaging anatomy and variation of vertebral artery and bone structure at craniocervical junction. Eur Spine J. 2009; 18:1102–1108. PMID: 19288143.
Article7. Elgafy H, Bransford RJ, McGuire RA, Dettori JR, Fischer D. Blood loss in major spine surgery: are there effective measures to decrease massive hemorrhage in major spine fusion surgery? Spine (Phila Pa 1976). 2010; 35:S47–S56. PMID: 20407351.8. Farey ID, Nadkarni S, Smith N. Modified Gallie technique versus transarticular screw fixation in C1-C2 fusion. Clin Orthop Relat Res. 1999; 126–135.
Article9. Goel A, Bhatjiwale M, Desai K. Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg. 1998; 88:962–968. PMID: 9609289.
Article10. Haid RW Jr, Subach BR, McLaughlin MR, Rodts GE Jr, Wahlig JB Jr. C1-C2 transarticular screw fixation for atlantoaxial instability: a 6-year experience. Neurosurgery. 2001; 49:65–68. discussion 69-70. PMID: 11440461.
Article11. Huang DG, Hao DJ, He BR, Wu QN, Liu TJ, Wang XD, et al. Posterior atlantoaxial fixation: a review of all techniques. Spine J. 2015; 15:2271–2281. PMID: 26165477.
Article12. Joaquim AF, Ghizoni E, Tedeschi H, Lawrence B, Brodke DS, Vaccaro AR, et al. Upper cervical injuries - a rational approach to guide surgical management. J Spinal Cord Med. 2014; 37:139–151. PMID: 24559418.
Article13. Khanfour AA, El Sekily NM. Relation of the vertebral artery segment from C1 to C2 vertebrae: an anatomical study. Alex J Med. 2015; 51:143–151.
Article14. Menezes AH, Traynelis VC. Anatomy and biomechanics of normal craniovertebral junction (a) and biomechanics of stabilization (b). Childs Nerv Syst. 2008; 24:1091–1100. PMID: 18389261.
Article15. Moskovich R, Crockard HA. Atlantoaxial arthrodesis using interlaminar clamps. An improved technique. Spine (Phila Pa 1976). 1992; 17:261–267. PMID: 1566161.16. Rogers WA. Fractures and dislocations of the cervical spine; an end-result study. J Bone Joint Surg Am. 1957; 39-A:341–376. PMID: 13416330.17. Stillerman CB, Wilson JA. Atlanto-axial stabilization with posterior transarticular screw fixation: technical description and report of 22 cases. Neurosurgery. 1993; 32:948–954. discussion 954-955. PMID: 8327097.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tinnitus Caused by Traumatic Posterior Auricular Artery-Internal Jugular Vein Fistula
- Epidural Hematoma Presenting with Severe Neck Pain without Neurological Deficit - A Late Complication of Posterior Cervical Spine Surgery: Presentation of Three Unusual Cases
- Posterior Cervical Plate Fixation in Cervical Injuries
- Intervertebral Foraminal Widening Caused by the Tortuous Cervical Vertebral Artery
- Circumferential Operations of the Cervical Spine